肝硬化食管胃静脉曲张出血患者胃镜治疗术后再出血的影响因素分析
DOI: 10.3969/j.issn.1001-5256.2021.09.018
Influencing factors of rebleeding after gastroscopy in patients with liver cirrhosis and esophagogastric variceal bleeding
-
摘要:
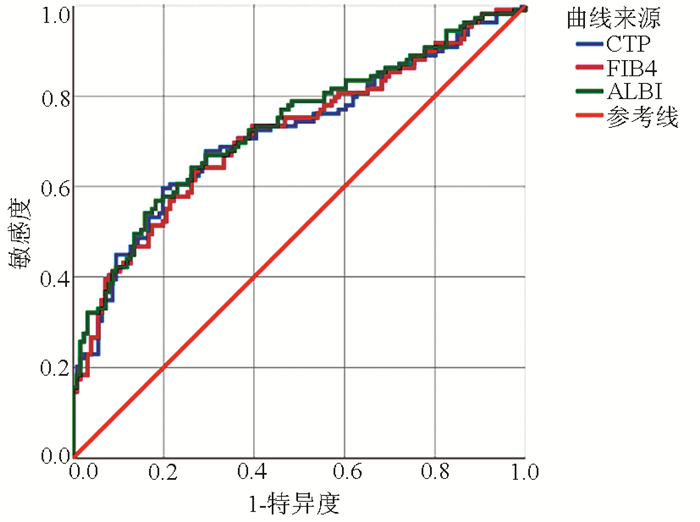
目的 分析肝硬化食管胃静脉曲张出血患者胃镜治疗术后再出血的影响因素。 方法 回顾性分析2017年1月1日—2018年12月31日于天津市第三中心医院住院的肝硬化食管胃静脉曲张出血并行胃镜治疗的患者临床资料,依据是否发生再出血及出血时间,分为未出血组(n=148)与出血组(n=119),分析影响胃镜治疗术后再出血的危险因素。计量资料两组间比较采用t检验或Mann-Whitney U秩和检验; 计数资料两组间比较采用χ2检验。采用Cox回归模型进行单因素及多因素分析。应用受试者工作特征(ROC)曲线评估Child-Turcotte-Pugh(CTP)评分、肝纤维化4因子指数(FIB-4)、白蛋白-胆红素(ALBI)评分预测胃镜治疗术后再出血的准确性; 使用MedCalc软件比较ROC曲线下面积(AUC)的差异。 结果 共纳入267例肝硬化食管胃静脉曲张出血患者,其中合并肝癌患者53例(19.9%)。119例患者发生再出血,总再出血率为44.6%,中位再出血时间为11.0(0~39.0)个月。Cox单因素分析结果显示肝癌(HR=0.377,P<0.001)、AST(HR=1.002,P=0.025)、血Na(HR=0.935,P=0.004)、FIB-4(HR=1.030,P=0.049)均与再出血相关; Cox多因素分析结果显示肝癌(HR=0.357,P<0.001)、AST(HR=1.003,P=0.030)、PT(HR=0.196,P=0.001)、CTP(HR=1.289,P=0.014)、FIB-4(HR=1.062,P=0.033)、ALBI(HR=0.433,P=0.011)均是再出血的独立影响因素。CTP、FIB-4、ALBI评分预测再出血的AUC分别为0.711(95%CI:0.647~0.776)、0.705(95%CI:0.640~0.770)、0.730(95%CI:0.667~0.793)。CTP、FIB-4、ALBI 3个评分的AUC比较,差异均无统计学意义(P值均>0.05)。 结论 肝硬化食管胃静脉曲张出血行胃镜治疗的患者,肝癌、AST、PT、CTP、FIB-4、ALBI均与胃镜治疗术后再出血有关,其中CTP、FIB-4、ALBI 3项评分对再出血结局均有很好的预测价值,且预测能力无差异。 Abstract:Objective To investigate the influencing factors for rebleeding after gastroscopy in patients with liver cirrhosis and esophagogastric variceal bleeding. Methods A retrospective analysis was performed for the clinical data of the patients with liver cirrhosis and esophagogastric variceal bleeding who were hospitalized in Tianjin Third Central Hospital from January 1, 2017 to December 31, 2018, and according to the presence or absence of rebleeding and bleeding time, the patients were divided into non-bleeding group (n=148) and bleeding group (n=119). The risk factors for rebleeding after gastroscopy were analyzed. The t-test or the Mann-Whitney U test was used for comparison of continuous data between two groups, and the chi-square test was used for comparison of categorical data between two groups. The Cox regression model was used for univariate and multivariate analyses. The receiver operating characteristic (ROC) curve was used to evaluate the accuracy of Child-Turcotte-Pugh (CTP), fibrosis-4 (FIB-4), and albumin-bilirubin (ALBI) scores in predicting rebleeding after gastroscopy, and MedCalc was used to compare the area under the ROC curve (AUC). Results A total of 267 patients with liver cirrhosis and esophagogastric variceal bleeding were enrolled, among whom 53 (19.9%) had liver cancer. A total of 119 patients suffered from rebleeding, with an overall rebleeding rate of 44.6% and a median time to rebleeding of 11.0 (0-39.0) months. The univariate Cox regression analysis showed that liver cancer (hazard ratio [HR]=0.377, P < 0.001), aspartate aminotransferase (AST) (HR=1.002, P=0.025), serum Na (HR=0.935, P=0.004), and FIB-4 (HR=1.030, P=0.049) were associated with rebleeding, and the multivariate Cox regression analysis showed that liver cancer (HR=0.357, P < 0.001), AST (HR=1.003, P=0.030), prothrombin time (PT) (HR=0.196, P=0.001), CTP score (HR=1.289, P=0.014), FIB-4 (HR=1.062, P=0.033), and ALBI score (HR=0.433, P=0.011) were independent risk factors for rebleeding. CTP, FIB-4, and ALBI scores had an AUC of 0.711 (95% confidence interval [CI]: 0.647-0.776), 0.705 (95% CI: 0.640-0.770), and 0.730 (95% CI: 0.667-0.793), respectively, in predicting rebleeding. There was no significant difference in AUC between CTP, FIB-4, and ALBI scores (P > 0.05). Conclusion Liver cancer, AST, PT, CTP score, FIB-4 score, and ALBI score are associated with rebleeding after gastroscopy in patients with liver cirrhosis and esophagogastric variceal bleeding, among which CTP, FIB-4, and ALBI scores have a good value in predicting rebleeding outcome, while there is no significant difference in predictive ability between them. -
Key words:
- Liver Cirrhosis /
- Esophageal and Gastric Varices /
- Gastroscopy /
- Hemorrhage /
- Root Cause Analysis
-
表 1 未出血组与出血组患者基线特征比较
变量 未出血组(n=148) 出血组(n=119) 统计值 P值 年龄(岁) 56.76±11.33 57.15±11.64 t=-0.279 0.780 性别[例(%)] χ2=0.030 0.899 男 93(62.8) 76(63.9) 女 55(37.2) 43(36.1) AST(U/L) 32.00(22.25~49.75) 37.00(24.00~69.00) Z=-1.541 0.123 ALT(U/L) 24.00(16.00~37.75) 24.00(18.00~41.00) Z=-0.927 0.354 TBil(μmol/L) 21.45(15.13~33.53) 18.80(14.10~32.60) Z=-1.132 0.258 Alb(g/L) 31.25±5.55 32.40±5.80 t=-1.656 0.099 PT(s) 16.89±2.88 16.38±2.97 t=1.410 0.160 INR 1.38±0.30 1.34±0.32 t=1.111 0.268 WBC(×109/L) 4.33(2.77~6.50) 4.46(2.98~6.68) Z=-0.706 0.480 PLT(×109/L) 72.00(52.00~107.75) 88.00(56.00~15.00) Z=-0.940 0.347 Hb(g/L) 84.05±18.89 85.03±21.07 t=-0.399 0.690 Cr(μmol/L) 61.55(52.08~81.78) 62.00(51.00~74.00) Z=-0.077 0.939 BUN(mmol/L) 7.30(5.14~9.81) 7.47(4.66~9.72) Z=-0.169 0.866 Na(mmol/L) 139.33±3.86 138.39±3.64 t=2.036 0.043 脾长(cm) 15.27±2.41 15.33±2.78 t=-0.177 0.860 肝癌[例(%)] χ2=8.381 0.005 否 128(86.5) 86(72.3) 是 20(13.5) 33(27.7) CTP分级[例(%)] χ2=0.792 0.673 A级 67(45.3) 58(48.7) B级 65(43.9) 46(38.7) C级 16(10.8) 15(12.6) PLTSLE评分(分) 444.76(335.45~690.68) 516.67(322.40~762.59) Z=-1.214 0.225 APRI评分(分) 1.12(0.71~1.91) 1.17(0.75~2.34) Z=-0.878 0.380 FIB-4评分(分) 5.53(3.31~8.21) 5.37(3.18~8.69) Z=-0.542 0.588 GBS评分(分) 10.61±3.03 10.47±3.22 t=0.376 0.707 ALBI评分(分) -1.47±0.57 -1.60±0.66 t=1.743 0.083 MELD评分(分) 11.82±3.87 11.14±3.81 t=1.425 0.155 是否随访内镜治疗[例(%)] χ2=0.114 0.799 是 53(35.8) 74(62.2) 否 95(64.2) 45(37.8) 内镜随访治疗(次) 0(0~1) 0(0~1) Z=-0.263 0.792 表 2 再出血影响因素Cox回归分析
因素 单因素分析 多因素分析 HR(95%CI) P值 HR(95%CI) P值 性别 1.065(0.732~1.548) 0.743 年龄 1.004(0.988~1.020) 0.661 肝癌 0.377(0.251~0.566) <0.001 0.357(0.220~0.581) <0.001 AST 1.002(1.000~1.003) 0.025 1.003(1.000~1.005) 0.030 ALT 1.002(0.998~1.005) 0.405 TBil 1.002(0.993~1.010) 0.697 Alb 1.014(0.983~1.047) 0.387 PT 0.957(0.892~1.028) 0.228 0.196(0.077~0.498) 0.001 INR 0.735(0.381~1.422) 0.361 PLT 1.001(0.997~1.004) 0.788 Hb 1.001(0.991~1.010) 0.890 Cr 0.999(0.994~1.004) 0.683 Na 0.935(0.893~0.979) 0.004 CTP评分 1.037(0.939~1.144) 0.474 1.289(1.053~1.576) 0.014 PLTSLE评分 1.000(1.000~1.001) 0.134 APRI评分 1.029(0.972~1.090) 0.329 FIB-4评分 1.030(1.000~1.061) 0.049 1.062(1.005~1.122) 0.033 GBS评分 0.996(0.940~1.055) 0.895 ALBI评分 0.870(0.643~1.177) 0.366 0.433(0.228~0.823) 0.011 MELD评分 0.977(0.928~1.027) 0.362 是否随访内镜治疗 1.091(0.753~1.582) 0.644 随访治疗次数 0.935(0.794~1.100) 0.416 -
[1] Chinese Society of Spleen and Portal Hypertension Surgery, Chinese Society of Surgery, Chinese Medical Association. Expert consensus on diagnosis and treatment of esophagogastric variceal bleeding in cirrhotic portal hypertension(2019 edition)[J]. Chin J Pract Surg, 2019, 39(12): 1241-1247. DOI: 10.19538/j.cjps.issn1005-2208.2019.12.01.中华医学会外科学分会脾及门静脉高压外科学组. 肝硬化门静脉高压症食管、胃底静脉曲张破裂出血诊治专家共识(2019版)[J]. 中国实用外科杂志, 2019, 39(12): 1241-1247. DOI: 10.19538/j.cjps.issn1005-2208.2019.12.01. [2] BOSCH J, GARCÍA-PAGÁN JC. Prevention of variceal rebleeding[J]. Lancet, 2003, 361(9361): 952-954. DOI: 10.1016/S0140-6736(03)12778-X. [3] Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Gastroenterology, Chinese Medical Association; Chinese Society of Endoscopy, Chinese Medical Association. Guidelines for the diagnosis and treatment of esophageal and gastric variceal bleeding in cirrhotic portal hypertension[J]. J Clin Hepatol, 2016, 32(2): 203-219. DOI: 10.3969/j.issn.1001-5256.2016.02.002.中华医学会肝病学分会, 中华医学会消化病学分会, 中华医学会内镜学分会. 肝硬化门静脉高压食管胃静脉曲张出血的防治指南[J]. 临床肝胆病杂志, 2016, 32(2): 203-219. DOI: 10.3969/j.issn.1001-5256.2016.02.002. [4] REN LM, DANG T, MENG XM, et al. Analysis of risk factors for early rebleeding after endoscopic treatment of cirrhotic esophageal varices bleeding[J/C]. Chin J Gastrointestinal Endoscopy (Electronic Edition), 2019, 6(2): 57-61. DOI: 10.3877/cma.j.issn.2095-7157.2019.02.002.任丽梅, 党彤, 孟宪梅, 等. 肝硬化食管静脉曲张出血内镜治疗后早期再出血的危险因素分析[J/CD]. 中华胃肠内镜电子杂志, 2019, 6(2): 57-61. DOI: 10.3877/cma.j.issn.2095-7157.2019.02.002. [5] ALTAMIRANO J, ZAPATA L, AGUSTIN S, et al. Predicting 6-week mortality after acute variceal bleeding: Role of classification and regression tree analysis[J]. Ann Hepatol, 2009, 8(4): 308-315. http://journals.indexcopernicus.com/fulltxt.php?ICID=900181 [6] KRIGE JE, SHAW JM, BORNMAN PC, et al. Early rebleeding and death at 6 weeks in alcoholic cirrhotic patients with acute variceal bleeding treated with emergency endoscopic injection sclerotherapy[J]. S Afr J Surg, 2009, 47(3): 72-74, 76-79. [7] ROUT G, SHARMA S, GUNJAN D, et al. Development and validation of a novel model for outcomes in patients with cirrhosis and acute variceal bleeding[J]. Dig Dis Sci, 2019, 64(8): 2327-2337. DOI: 10.1007/s10620-019-05557-y. [8] HWANG JH, SHERGILL AK, ACOSTA RD, et al. The role of endoscopy in the management of variceal hemorrhage[J]. Gastrointest Endosc, 2014, 80(2): 221-227. DOI: 10.1016/j.gie.2013.07.023. [9] LEUNG JC, LOONG TC, PANG J, et al. Invasive and non-invasive assessment of portal hypertension[J]. Hepatol Int, 2018, 12(Suppl 1): 44-55. DOI: 10.1007/s12072-017-9795-0. [10] ZHOU SY, DUAN ZH. Noninvasive diagnosis of esophageal varices in liver cirrhosis[J]. J Clin Hepatol, 2020, 36(8): 1842-1846. DOI: 10.3969/j.issn.1001-5256.2020.08.036.周胜云, 段志辉. 肝硬化食管静脉曲张的无创诊断[J]. 临床肝胆病杂志, 2020, 36(8): 1842-1846. DOI: 10.3969/j.issn.1001-5256.2020.08.036. [11] KRAJA B, MONE I, AKSHIJA I, et al. Predictors of esophageal varices and first variceal bleeding in liver cirrhosis patients[J]. World J Gastroenterol, 2017, 23(26): 4806-4814. DOI: 10.3748/wjg.v23.i26.4806. [12] HASSAN EM, OMRAN DA, EL BESHLAWEY ML, et al. Can transient elastography, Fib-4, Forns Index, and Lok Score predict esophageal varices in HCV-related cirrhotic patients?[J]. Gastroenterol Hepatol, 2014, 37(2): 58-65. DOI: 10.1016/j.gastrohep.2013.09.008. [13] KOTHARI HG, GUPTA SJ, GAIKWAD NR, et al. Role of non-invasive markers in prediction of esophageal varices and variceal bleeding in patients of alcoholic liver cirrhosis from central India[J]. Turk J Gastroenterol, 2019, 30(12): 1036-1043. DOI: 10.5152/tjg.2019.18334. [14] LIN PT, TENG W, JENG WJ, et al. The incidence and predictors of post transarterial chemoembolization variceal bleeding in hepatocellular carcinoma patients[J]. J Formos Med Assoc, 2020, 119(2): 635-643. DOI: 10.1016/j.jfma.2019.08.019. [15] CHAN AW, KUMADA T, TOYODA H, et al. Integration of albumin-bilirubin (ALBI) score into Barcelona Clinic Liver Cancer (BCLC) system for hepatocellular carcinoma[J]. J Gastroenterol Hepatol, 2016, 31(7): 1300-1306. DOI: 10.1111/jgh.13291. [16] HSIEH YC, LEE KC, WANG YW, et al. Correlation and prognostic accuracy between noninvasive liver fibrosismarkers and portal pressure in cirrhosis: Role of ALBI score[J]. PLoS One, 2018, 13(12): e0208903. DOI: 10.1371/journal.pone.0208903. [17] TOYODA H, LAI PB, O'BEIRNE J, et al. Long-term impact of liver function on curative therapy for hepatocellular carcinoma: Application of the ALBI grade[J]. Br J Cancer, 2016, 114(7): 744-750. DOI: 10.1038/bjc.2016.33. [18] ZOU D, QI X, ZHU C, et al. Albumin-bilirubin score for predicting the in-hospital mortality of acute upper gastrointestinal bleeding in liver cirrhosis: A retrospective study[J]. Turk J Gastroenterol, 2016, 27(2): 180-186. DOI: 10.5152/tjg.2016.15502. [19] XAVIER SA, VILAS-BOAS R, BOAL CARVALHO P, et al. Assessment of prognostic performance of Albumin-Bilirubin, Child-Pugh, and Model for End-stage Liver Disease scores in patients with liver cirrhosis complicated with acute upper gastrointestinal bleeding[J]. Eur J Gastroenterol Hepatol, 2018, 30(6): 652-658. DOI: 10.1097/MEG.0000000000001087. [20] FOUAD TR, ABDELSAMEEA E, ABDEL-RAZEK W, et al. Upper gastrointestinal bleeding in Egyptian patients with cirrhosis: Post-therapeutic outcome and prognostic indicators[J]. J Gastroenterol Hepatol, 2019, 34(9): 1604-1610. DOI: 10.1111/jgh.14659. -



 PDF下载 ( 2088 KB)
PDF下载 ( 2088 KB)

 下载:
下载:


