Clinical significance of homocysteine and neutrophil-to-lymphocyte ratio in patients with nonalcoholic fatty liver disease and type 2 diabetes mellitus
-
摘要:
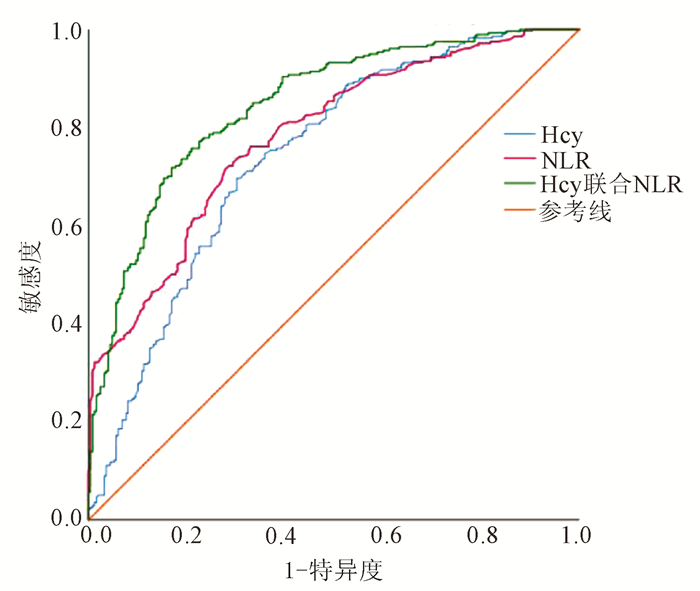
目的 探讨同型半胱氨酸(Hcy)及中性粒细胞与淋巴细胞比值(NLR)在非酒精性脂肪性肝病(NAFLD)合并2型糖尿病(T2DM)患者中的水平及临床意义。 方法 选取2019年1月—12月锦州医科大学附属第一医院内分泌科的NAFLD患者528例,根据其是否合并2型糖尿病分为未合并T2DM组及合并T2DM组,并随机选取未合并NAFLD的单纯性T2DM患者79例,记录3组患者的一般资料及实验室指标。计量资料符合正态分布数据组间比较采用单因素方差分析;计数资料组间比较采用χ2检验。危险因素分析采用二元logistic回归分析,用OR及其95%CI表示相对危险度。采用受试者工作特征曲线(ROC曲线)评价预测效能。 结果 合并T2DM组患者SBP、DBP及BMI显著高于未合并T2DM组(P值均<0.05)。Hcy、NLR、ALT、AST、GGT、UA、FBG两两组间比较差异均有统计学意义(P值均<0.05)。Neut、Lym及HDL-C在合并T2DM组与未合并T2DM组中比较差异有统计学意义(P值均<0.05)。TC在合并T2DM组与单纯T2DM组、未合并T2DM组与单纯T2DM组比较差异均有统计学意义(P值均<005)。SBP、HDL-C、NLR、Hcy为NAFLD合并T2DM的独立危险因素[OR(95%CI):1.040(1.015~1.065)、0.040(0.007~0.228)、6.285(1.504~27.108)、1.291(1.127~1.423),P值均<0.05]。Hcy预测NAFLD合并T2DM的曲线下面积为0.741(95%CI:0.698~0783,P<0.01),Youden指数为0.394,预测临界值为15.31 μmol/L,敏感度为69.6%,特异度为69.8%。NLR预测NAFLD合并T2DM的曲线下面积为0.782(95%CI:0.744~0.820,P<0.01),Youden指数为0.443,预测临界值为2.12,敏感度为72.1%,特异度为72.2%。Hcy联合NLR预测NAFLD合并T2DM的曲线下面积为0.845(95%CI:0.812~0.878,P<0.01),Youden指数为0549,敏感度为71.8%,特异度为83.1%。 结论 Hcy及NLR是NAFLD合并T2DM发生的危险因素,对于该疾病的发生具有预测价值。Hcy联合NLR检测可提高NAFLD合并T2DM的诊断效能,有助于临床医生早期识别。 Abstract:Objective To investigate the levels and clinical significance of homocysteine (Hcy) and neutrophil-to-lymphocyte ratio (NLR) in patients with nonalcoholic fatty liver disease (NAFLD) and type 2 diabetes mellitus (T2DM). Methods A total of 528 patients with NAFLD who were treated in Department of Endocrinology, The First Affiliated Hospital of Jinzhou Medical University, from January to December 2019 were enrolled, and according to the presence or absence of T2DM, they were divided into non-T2DM group and T2DM group. A total of 79 T2DM patients without NAFLD were selected randomly. General data and laboratory markers were recorded for the three groups. A one-way analysis of variance was used for comparison of normally distributed continuous data between groups, and the chi-square test was used for comparison of categorical data between groups; a binary logistic regression analysis was used to determine risk factors, and odds ratio (OR) and its 95% confidence interval (CI) were used to represent relative risk; the receiver operating characteristic (ROC) curve was used to evaluate predictive efficiency. Results The T2DM group had significantly higher systolic blood pressure (SBP), diastolic blood pressure, and body mass index than the non-T2DM group (all P < 0.05), and there were significant differences between any two of the three groups in Hcy, NLR, alanine aminotransferase, aspartate aminotransferase, gamma-glutamyl transpeptidase, uric acid, and fasting blood glucose (all P < 0.05). There were significant differences in neutrophil count, lymphocyte count, and high-density lipoprotein cholesterol (HDL-C) between the T2DM group and the non-T2DM group (all P < 0.05), and there was a significant difference in total cholesterol between the T2DM group and the simple T2DM group and between the non-T2DM group and the simple T2DM group (P < 0.05). SBP (OR=1.040, 95%CI: 1.015-1.065), HDL-C (OR=0.040, 95%CI: 0.007-0.228), NLR (OR=6.285, 95%CI: 1.504-27.108), and Hcy (OR=1.291, 95%CI: 1.127-1.423) were independent risk factors for NAFLD with T2DM. Hcy had an area under the ROC curve (AUC) of 0.741 (95%CI: 0.698-0.783, P < 0.01) in predicting NAFLD with T2DM, with a Youden index of 0.394, a sensitivity of 69.6%, and a specificity of 69.8% at the optimal cut-off value of 15.31 μmol/L. NLR had an AUC of 0.782 (95%CI: 0.744-0.820, P < 0.01) in predicting NAFLD with T2DM, with a Youden index of 0.443, a sensitivity of 72.1%, and a specificity of 72.2% at the optimal cut-off value of 2.12. Hcy combined with NLR had an AUC of 0.845 (95%CI: 0.812-0.878, P < 0.01) in predicting NAFLD with T2DM, with a Youden index of 0.549, a sensitivity of 71.8%, and a specificity of 83.1%. Conclusion Hcy and NLR are risk factors for NAFLD with T2DM and have a certain predictive value. Combined measurement of Hcy and NLR can improve the diagnostic efficiency of NAFLD with T2DM and help clinicians with diagnosis in the early stage. -
Key words:
- Non-Alcoholic Fatty Liver Disease /
- Diabetes Mellitus, Type 2 /
- Cysteine /
- Neutrophil /
- Lymphocytes
-
表 1 合并T2DM组与未合并T2DM组患者一般资料及实验室指标的比较
指标 未合并T2DM组(n=248) 合并T2DM组(n=280) 单纯T2DM组(n=79) 统计值 P值 冠心病史[例(%)] 76(30.6) 94(33.6) 23(29.1) χ2=0.821 0.663 吸烟[例(%)] 65(26.2) 76(27.1) 17(21.5) χ2=1.019 0.601 饮酒[例(%)] 71(28.6) 95(33.9) 17(21.5) χ2=4.965 0.084 高血压病史[例(%)] 48(19.4) 59(21.1) 19(24.1) χ2=0.834 0.659 高脂血症[例(%)] 86(34.7) 101(36.1) 27(34.2) χ2=0.158 0.924 高尿酸血症[例(%)] 56(22.6) 66(23.6) 17(21.5) χ2=0.171 0.918 男性[例(%)] 187(66.8) 187(66.8) 58(73.4) χ2=5.256 0.072 年龄(岁) 55.29±10.14 56.14±9.15 56.54±8.86 F=0.763 0.467 BMI(kg/m2) 26.46±2.73 27.47±3.051)2) 25.94±2.89 F=12.411 <0.01 SBP(mmHg) 129.82±16.89 145.71±18.611)2) 128.76±12.32 F=66.484 <0.01 DBP(mmHg) 81.78±11.39 88.37±11.301)2) 82.28±9.70 F=25.466 <0.01 TC(mmol/L) 5.31±0.81 5.30±0.922) 4.92±0.721) F=7.057 0.001 TG(mmol/L) 1.99±1.29 2.17±1.24 1.91±1.05 F=2.117 0.121 HDL-C(mmol/L) 1.41±0.21 1.26±0.231) 1.30±0.381) F=26.811 <0.01 LDL-C(mmol/L) 3.34±0.75 3.49±0.89 3.39±0.73 F=2.268 0.104 ALT(U/L) 28.63±9.03 32.11±15.341)2) 24.33±8.131) F=13.901 <0.01 AST(U/L) 20.34±5.97 21.69±8.581)2) 18.47±5.091) F=6.759 0.001 GGT(U/L) 34.31±21.14 39.06±23.471)2) 24.18±8.901) F=15.601 <0.01 NLR 1.85±0.59 2.71±0.971)2) 1.81±0.601) F=9.450 <0.01 Hcy(μmol/L) 14.13±3.10 16.70±2.581)2) 10.51±3.061) F=15.712 <0.01 Neut(×109/L) 3.75±0.94 4.89±1.081)2) 3.66±0.68 F=107.415 <0.01 Lym(×109/L) 2.16±0.61 1.96±0.581)2) 2.18±0.68 F=9.468 <0.01 UA(μmol/L) 361.36±83.82 384.78±77.711)2) 317.74±57.631) F=23.637 <0.01 FBG(mmol/L) 4.60±0.05 7.54±0.291)2) 10.24±2.151) F=178.664 <0.01 注:与未合并T2DM组比较,1) P<0.05;与单纯T2DM组比较,2) P<0.05。 表 2 NAFLD合并T2DM的独立危险因素的二元logistic回归分析
项目 B值 SE Wald χ2 OR 95%CI P值 SBP 0.039 0.012 10.351 1.040 1.015~1.065 0.001 HDL-C -3.215 0.885 13.192 0.040 0.007~0.228 <0.001 NLR 1.854 0.738 6.316 6.285 1.504~27.108 0.012 Hcy 0.256 0.049 26.862 1.291 1.127~1.423 <0.001 -
[1] FAN JG, ZENG J. Epidemic status and harm of non-alcoholic fatty liver disease[J]. Chin J Dig, 2020, 40(9): 577-580. DOI: 10.3760/cma.j.cn311367-20200526-00349.范建高, 曾静. 非酒精性脂肪性肝病的流行现状与危害[J]. 中华消化杂志, 2020, 40(9): 577-580. DOI: 10.3760/cma.j.cn311367-20200526-00349. [2] SHEKA AC, ADEYI O, THOMPSON J, et al. Nonalcoholic steatohepatitis: A review[J]. JAMA, 2020, 323(12): 1175-1183. DOI: 10.1001/jama.2020.2298. [3] de ALWIS NM, DAY CP. Non-alcoholic fatty liver disease: The mist gradually clears[J]. J Hepatol, 2008, 48(Suppl 1): s104-s112. DOI: 10.1016/j.jhep.2008.01.009. [4] TARGHER G, BYRNE CD. Clinical review: Nonalcoholic fatty liver disease: A novel cardiometabolic risk factor for type 2 diabetes and its complications[J]. J Clin Endocrinol Metab, 2013, 98(2): 483-495. DOI: 10.1210/jc.2012-3093. [5] PUCHAKAYALA BK, VERMA S, KANWAR P, et al. Histopathological differences utilizing the nonalcoholic fatty liver disease activity score criteria in diabetic (type 2 diabetes mellitus) and non-diabetic patients with nonalcoholic fatty liver disease[J]. World J Hepatol, 2015, 7(25): 2610-2618. DOI: 10.4254/wjh.v7.i25.2610. [6] CHEN LL, FU MX, MENG XB, et al. Clinical value of fasting C-peptide in assessing the progression of liver fibrosis in patients with NAFLD and T2DM[J]. J Prac Hepatol, 2020, 23(1): 38-41. DOI: 10.3969/j.issn.1672-5069.2020.01.012.陈丽丽, 符茂雄, 蒙绪标, 等. 空腹C肽评估NAFLD合并T2DM患者肝纤维化进展价值分析[J]. 实用肝脏病杂志, 2020, 23(1): 38-41. DOI: 10.3969/j.issn.1672-5069.2020.01.012. [7] MENG PY, ZHANG XY, YUAN HB, et al. Changes and significance of serum visfatin, Nesfatin-1, and insulin resistance in patients with type 2 diabetes mellitus and nonalcoholic fatty liver disease[J]. Pract Prev Med, 2020, 27(6): 745-747. DOI: 10.3969/j.issn.1006-3110.2020.06.031.孟佩盈, 张小英, 袁洪波, 等. T2DM并发NAFLD患者的血清内脂素, Nesfatin-1及胰岛素抵抗变化及其意义[J]. 实用预防医学, 2020, 27(6): 745-747. DOI: 10.3969/j.issn.1006-3110.2020.06.031. [8] CHEN YY, WANG ZQ, LI WH, et al. Association of serum homocysteine with cardiovascular and cerebrovascular diseases[J]. Int J Lab Med, 2016, 37(19): 2798-2799. DOI: 10.3969/j.issn.1673-4130.2016.19.066.陈园园, 王中全, 李文华, 等. 血清同型半胱氨酸与心脑血管病变的相关性研究[J]. 国际检验医学杂志, 2016, 37(19): 2798-2799. DOI: 10.3969/j.issn.1673-4130.2016.19.066. [9] XU XW, SHAO XZ, CAO J, et al. Serum levels of homocysteine and lipoprotein a in patients with acute cerebral hemorrhage and their diagnostic value[J]. Traum Crit Med, 2020, 8(6): 464-465, 468. DOI: 10.16048/j.issn.2095-5561.2020.06.19.许小伟, 邵祥忠, 曹建, 等. 急性脑出血患者血清同型半胱氨酸、脂蛋白a水平及其诊断价值研究[J]. 创伤与急危重病医学, 2020, 8(6): 464-465, 468. DOI: 10.16048/j.issn.2095-5561.2020.06.19. [10] SHEN XH, LI HW, CHEN H. The prognosis effects of neutrophil/lymphocyte ratio on myocardial perfusion in patients with myocardialinfarction[J]. Chin J Evid-Based Card Med, 2013, 5(1): 32-34. DOI: 1674-4055 (2013) 01-0032-03.沈絮华, 李虹伟, 陈晖. 中性粒细胞/淋巴细胞比值对心肌梗死患者心肌灌注及预后的评估[J]. 中国循证心血管医学杂志, 2013, 5(1): 32-34. DOI: 1674-4055 (2013) 01-0032-03. [11] ABDEL-RAZIK A, MOUSA N, SHABANA W, et al. A novel model using mean platelet volume and neutrophil to lymphocyte ratio as a marker of nonalcoholic steatohepatitis in NAFLD patients: Multicentric study[J]. Eur J Gastroenterol Hepatol, 2016, 28(1): e1-e9. DOI: 10.1097/MEG.0000000000000486. [12] XU J, BU N, JIAO Y, et al. Analysis of prevalence and risk factors of non-alcoholic fatty liver disease in patients with type 2 diabetes mellitus[J]. Chongqing Med, 2020, 49(14): 2284-2288, 2294. DOI: 10.3969/j.issn.1671-8348.2020.14.009.徐静, 卜宁, 焦杨, 等. 2型糖尿病患者合并非酒精性脂肪性肝病的患病率及危险因素分析[J]. 重庆医学, 2020, 49(14): 2284-2288, 2294. DOI: 10.3969/j.issn.1671-8348.2020.14.009. [13] ALBERTI KG, ZIMMET PZ. Definition, diagnosis and classification of diabetes mellituss and its complications. Part 1: Diagnosis and classiffication of diabetes mellitus. Provisional report of a WHO consultation[J]. Diabet Med, 1998, 15(7): 539-553. DOI: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [14] National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, Chinese Medical Association, Fatty Liver Expert Committee, Chinese Medical Doctor Association. Guidelines of prevention and treatment for nonalcoholic fatty liver disease: A 2018 update[J]. J Clin Hepatol, 2018, 34(5): 947-957. DOI: 10.3969/j.issn.1001-5256.2018.05.007中华医学会肝病学分会脂肪肝和酒精性肝病学组, 中国医师协会脂肪性肝病专家委员会. 非酒精性脂肪性肝病防治指南(2018年更新版)[J]. 临床肝胆病杂志, 2018, 34(5): 947-957. DOI: 10.3969/j.issn.1001-5256.2018.05.007. [15] MASCITELLI L, PEZZETTA F. Diagnosis of non-alcoholic fatty liver disease (NAFLD)[J]. JAMA, 2016, 290(12): 1577-1578. DOI: 10.1007/s00125-016-3944-1. [16] PAN JJ, FALLON MB. Gender and racial differences in nonalcoholic fatty liver disease[J]. World J Hepatol, 2014, 6(5): 274-283. DOI: 10.4254/wjh.v6.i5.274. [17] DAY CP, JAMES OF. Steatohepatitis: A tale of two "hits"?[J]. Gastroenterology, 1998, 114(4): 842-845. DOI: 10.1016/s0016-5085(98)70599-2. [18] LIU JQ, ZHANG ZJ, WANG W, et al. Risk factors for non-alcoholic fatty liver disease combined with type 2 diabetes mellitus in adolescents[J]. World Chin J Dig, 2015, 23(11): 1812-1817. DOI: 10.11569/wcjd.v23.i11.1812.刘建强, 张志坚, 王雯, 等. 青少年非酒精性脂肪肝合并2型糖尿病的危险因素[J]. 世界华人消化杂志, 2015, 23(11): 1812-1817. DOI: 10.11569/wcjd.v23.i11.1812. [19] MENG LW, WANG LC, CUI Q. Relationship between ferritin and homocysteine and non-alcoholic fatty liver disease in type 2 diabetes mellitus[J]. Guide China Med, 2020, 18(17): 137-138.孟令伟, 王丽春, 崔琦. 2型糖尿病患者铁蛋白及同型半胱氨酸与非酒精性脂肪肝的关系[J]. 中国医药指南, 2020, 18(17): 137-138. [20] LUBOS E, LOSCALZO J, HANDY DE. Homocysteine and glutathione peroxidase-1[J]. Antioxid Redox Signal, 2007, 9(11): 1923-1940. DOI: 10.1089/ars.2007.1771. [21] SCHLIEFSTEINER C, HIRSCHMUGL B, KOPP S, et al. Maternal Gestational Diabetes Mellitus increases placental and foetal lipoprotein-associated Phospholipase A2 which might exert protective functions against oxidative stress[J]. Sci Rep, 2017, 7(1): 12628. DOI: 10.1038/s41598-017-13051-6. [22] ZHENG HL, LI F, DING W, et al. Association between neutrophil-lymphocyte ratio and type 2 diabetes with nonalcoholic fatty liver disease[J]. Anhui Med J, 2020, 41(5): 562-566. DOI: 10.3969/j.issn.1000-0399.2020.05.019.郑海兰, 李凡, 丁维, 等. 中性粒细胞/淋巴细胞比值与2型糖尿病合并非酒精性脂肪肝的相关性分析[J]. 安徽医学, 2020, 41(5): 562-566. DOI: 10.3969/j.issn.1000-0399.2020.05.019. -



 PDF下载 ( 2111 KB)
PDF下载 ( 2111 KB)

 下载:
下载:


