肝硬化食管静脉曲张急诊套扎术后再出血的影响因素
DOI: 10.3969/j.issn.1001-5256.2022.08.016
Risk factors for rebleeding after emergency esophageal variceal ligation in patients with liver cirrhosis
-
摘要:
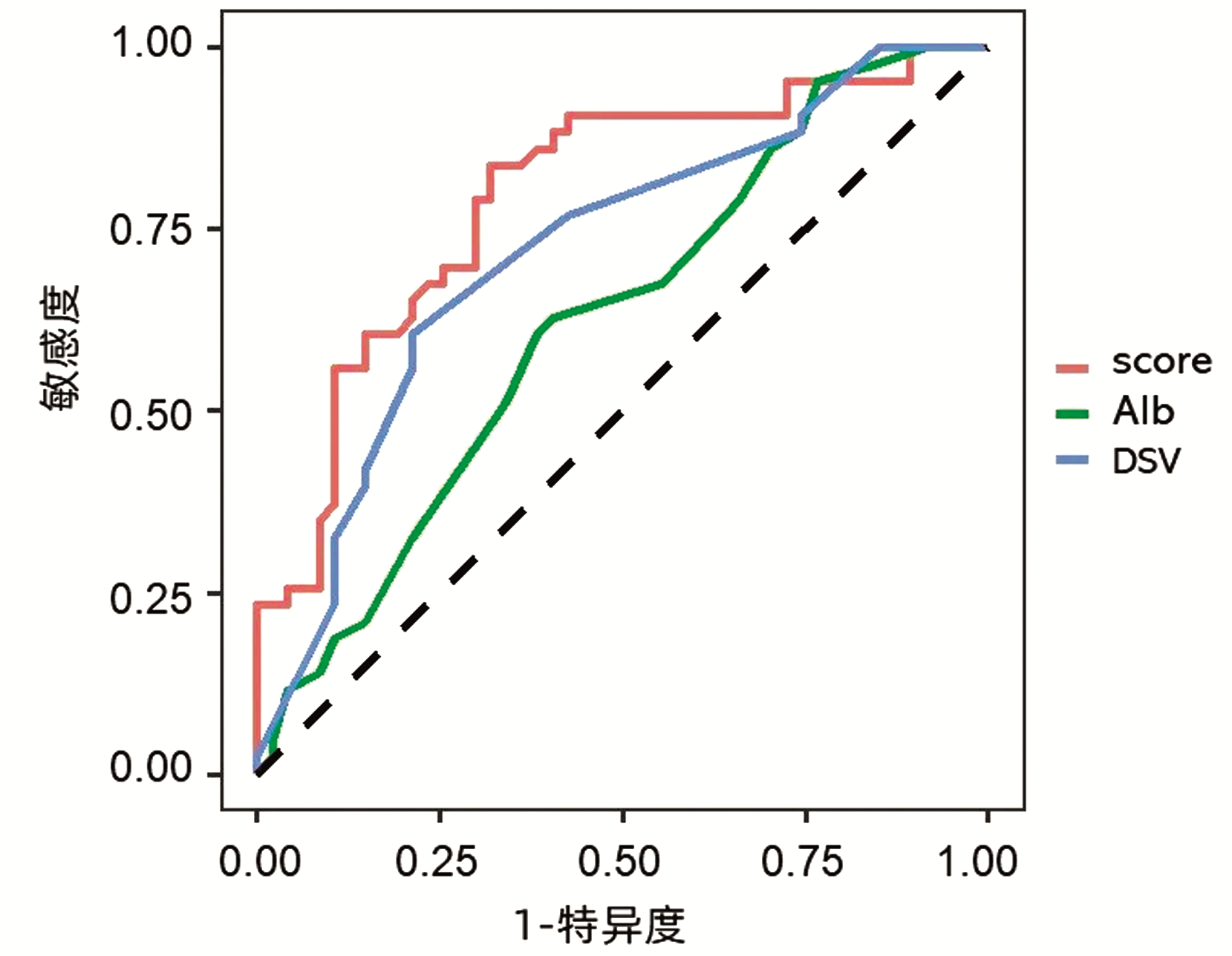
目的 探讨影响肝硬化食管静脉曲张急诊套扎术后再出血的危险因素。 方法 回顾性分析2016年1月—2019年12月解放军总医院第五医学中心290例行急诊食管静脉套扎术治疗的肝硬化患者的临床和实验室资料,根据患者随访1年时有无再出血,分为再出血组和未出血组各145例。符合正态分布的计量资料两组间比较采用t检验,不符合正态分布的计量资料两组间比较采用Wilcoxn秩和检验,计数资料两组间比较采用χ2检验,以筛选出的有统计学意义的因素为自变量进行多因素logistic回归分析,筛选出急诊食管静脉套扎术后再出血的独立相关因素,通过绘制受试者工作特征曲线,获得预测再出血概率的指标并建立模型。 结果 单因素分析显示两组间血小板计数(PLT)(t=-1.888,P=0.047)、Child-Pugh评分(χ2=5.975,P=0.049)、白蛋白(Alb)水平(t=-2.229,P=0.029)、脾静脉直径(DSV)(t=3.808,P=0.001)比较,差异均有统计学意义。多因素logistic回归分析结果显示,Child-Pugh评分[比值比(OR)=0.280,95%CI: 0.108~0.729,P=0.009]、DSV(OR=1.549,95%CI: 1.197~2.005, P=0.001)和Alb(OR=0.832, 95%CI: 0.729~0.949,P=0.006)是食管静脉套扎术后再出血的影响因素。3个因素联合建立预测模型的受试者工作特征曲线下面积0.796,敏感度为83.7%,特异度为74.5%,界值为-0.086。 结论 Child-Pugh评分、Alb水平、DSV为急诊食管静脉套扎术后再出血的独立相关因素,三者联合预测再出血的敏感度和特异度最高。 Abstract:Objective To investigate the risk factors for rebleeding after emergency esophageal variceal ligation (EVL) in patients with liver cirrhosis. Methods A retrospective analysis was performed for the clinical and laboratory data of 290 patients with liver cirrhosis who underwent emergency EVL in The Fifth Medical Center of Chinese PLA General Hospital from January 2016 to December 2019, and according to the presence or absence of rebleeding within 1-year follow-up, they were divided into rebleeding group and non-rebleeding group. The t-test was used for comparison of normally distributed continuous data between two groups, and the Wilcoxon rank sum test was used for comparison of non-normally distributed continuous data between two groups; the chi-square test was used for comparison of categorical data between two groups. A multivariate logistic regression analysis was performed with the statistically significant factors as independent variables to screen out the independent risk factors for rebleeding after emergency EVL, and the receiver operating characteristic (ROC) curve was plotted to obtain the indices for predicting the probability of rebleeding and establish a predictive model. Results The univariate analysis showed that there were significant differences between the two groups in platelet count (t=-1.888, P=0.047), Child-Pugh score (χ2=5.975, P=0.049), albumin level (t=-2.229, P=0.029), and splenic vein diameter (t=3.808, P=0.001). The multivariate logistic regression analysis showed that Child-Pugh score (odds ratio [OR]=0.280, 95% confidence interval [CI]: 0.108-0.729, P=0.009), splenic vein diameter (OR=1.549, 95%CI: 1.197-2.005, P=0.001) and albumin level (OR=0.832, 95%CI: 0.729-0.949, P=0.006) were independent influencing factors for rebleeding after EVL. The predictive model based on these three factors had an area under the ROC curve of 0.796, with a sensitivity of 83.7% and a specificity of 74.5% at the cut-off value of -0.086. Conclusion Child-Pugh score, albumin level, and splenic vein diameter are independent risk factors for rebleeding after emergency EVL, and the combination of the three indices has the highest sensitivity and specificity in predicting rebleeding. -
Key words:
- Liver Cirrhosis /
- Esophageal and Gastric Varices /
- Hemorrhage /
- Secondary Prevention /
- Risk Factors
-
表 1 再出血组和未出血组患者一般资料比较
Table 1. Comparison of general data between rebleeding group and non bleeding group
项目 再出血组(n=145) 未出血组(n=145) 统计值 P值 性别[例(%)] χ2=2.382 0.115 男 83(57.2) 88(60.7) 女 62(42.8) 57(39.3) 年龄(岁) 54.3±10.8 52.6±10.3 t=0.734 0.486 病因[例(%)] χ2=1.791 0.145 肝炎肝硬化 82(56.6) 78(53.8) 酒精性肝硬化 29(20.0) 30(20.7) 胆汁淤积性肝硬化 15(10.3) 18(12.4) 自身免疫性肝硬化 9 (6.2) 11(7.6) 其他原因肝硬化 10(6.9) 8(5.5) 曲张静脉程度(例) χ2=7.648 0.132 轻/中/重 24/46/75 28/39/78 表 2 急诊食管套扎术后再出血的单因素分析
Table 2. Single factor analysis of rebleeding after emergency esophageal ligation
项目 未出血组(n=145) 再出血组(n=145) 统计值 P值 Child-Pugh分级[例(%)] χ2=5.975 0.049 A级
B级
C级40(27.6)
67(46.2)
38(26.2)30(20.7)
101(69.6)
14(9.7)WBC(×1012/L) 5.18±3.79 5.04±3.15 t=-0.188 0.852 Hb(g/L) 79.26±21.07 80.91±22.96 t=0.356 0.723 PLT(×109/L) 98.83±92.12 66.63±34.74 t=-1.888 0.047 ALT(U/L) 33.06±32.73 73.40±25.24 t=1.086 0.280 AST(U/L) 38(26~74) 38(24~59) Z=-0.727 0.467 GGT(U/L) 52(22~149) 34(20~108) Z=-1.293 0.196 ALP(U/L) 144.20±148.48 105.44±61.00 t=-1.596 0.114 Alb(g/L) 30.57±7.06 27.72±4.98 t=-2.229 0.029 TBil(μmol/L) 18.50(14.10~43.70) 19(15.10~30.80) Z=-0.12 0.990 GLU(mmol/L) 8.70±6.03 8.48±4.79 t=-0.191 0.849 ChE(mmol/L) 2 673.00±1 194.99 2 706.88±1 134.84 t=0.138 0.891 UN(mmol/L) 8.17±5.97 7.46±3.36 t=-0.689 0.492 Cr(μmol/L) 75.11±51.02 69.26±15.60 t=-0.721 0.473 PT(s) 14.36±1.90 14.46±2.35 t=0.215 0.830 PTA(%) 61.11±13.48 62.08±16.05 t=0.312 0.756 INR 1.26±0.17 1.26±0.21 t=0.078 0.938 脾脏长度(mm) 161.36±25.80 165.81±25.50 t=0.823 0.413 DSV(mm) 10.57±2.05 12.25±2.14 t=3.808 0.001 DPV(mm) 12.95±2.05 13.70±3.70 t=1.201 0.233 表 3 影响急诊食管套扎术后再次出血的logistic多因素分析
Table 3. Effect of independent variables on rebleeding after emergency esophageal ligation
变量 B值 标准误 Wald值 OR(95%CI) P值 PLT 0.997(0.987~1.008) 0.595 Alb -0.183 0.070 7.914 0.832(0.729~0.949) 0.006 DSV 0.437 0.142 10.578 1.549(1.197~2.005) 0.001 Child-Pugh分级 -1.272 0.810 10.310 0.280(0.108~0.729) 0.009 -
[1] KRAJA B, MONE I, AKSHIJA I, et al. Predictors of esophageal varices and first variceal bleeding in liver cirrhosis patients[J]. World J Gastroenterol, 2017, 23(26): 4806-4814. DOI: 10.3748/wjg.v23.i26.4806. [2] BARI K, GARCIA-TSAO G. Treatment of portal hypertension[J]. World J Gatroenterol, 2012, 18(11): 1166-75. DOI: 10.3748/wjg.v18.i11.1166. [3] Chinese Society of Hepatology, Chinese Medical Association. Chinese guidelines on the management of liver cirrhosis[J]. J Clin Hepatol, 2019, 35(11): 2408-2425. DOI: 10.3969/j.issn.1001-5256.2019.11.006.中华医学会肝病学分会. 肝硬化诊治指南[J]. 临床肝胆病杂志, 2019, 35(11): 2408-2425. DOI: 10.3969/j.issn.1001-5256.2019.11.006. [4] Chinese Society of Hepatology, Chinese Medical Association, Chinese Society of Gastroenterology, Chinese Medical Association, Chinese Society of Endoscopy, Chinese Medical Association. Guidelines for the diagnosis and treatment of esophageal and gastric variceal bleeding in cirrhotic portal hypertension[J]. J Clin Hepatol, 2016, 32(2): 203-219. DOI: 10.3969/j.issn.1001-5256.2016.02.002.中华医学会肝病学分会, 中华医学会消化病学分会, 中华医学会内镜学分会. 肝硬化门静脉高压食管胃静脉曲张出血的防治指南[J]. 临床肝胆病杂志, 2016, 32(2): 203-219. DOI: 10.3969/j.issn.1001-5256.2016.02.002. [5] Chinese Society of Spleen and Portal Hypertension Surgery, Chinese Society of Surgery, Chinese Medical Association. Expert consensus on diagnosis and treatment of esophagogastric variceal bleeding in cirrhotic portal hypertension (2019 edition)[J]. Chin J Surg, 2019, 57(12): 885-892. DOI: 10.3760/cma.j.issn.0529-5815.2019.12.002.中华医学会外科学分会脾及门静脉高压外科学组. 肝硬化门静脉高压症食管、胃底静脉曲张破裂出血诊治专家共识(2019版)[J]. 中华外科杂志, 2019, 57(12): 885-892. DOI: 10.3760/cma.j.issn.0529-5815.2019.12.002. [6] LO GH. Endoscopic treatments for portal hypertension[J]. Hepatol Int, 2018, 12(Suppl 1): 91-101. DOI: 10.1007/s12072-017-9828-8. [7] ZHANG YY, CHEN GD, WANG ZF, et al. Clinical characteristics and endoscopic findings in patients with cirrhotic upper gastrointestinal variceal bleeding[J]. Chin J General Surg, 2018, 33(2): 134-137. DOI: 10.3760/cma.j.issn.1007-631X.2018.02.010.张媛媛, 陈国栋, 王智峰, 等. 肝硬化患者静脉曲张出血的临床和内镜特点分析[J]. 中华普通外科杂志, 2018, 33(2): 134-137. DOI: 10.3760/cma.j.issn.1007-631X.2018.02.010. [8] CHEN SY. Problems and countermeasures of endoscopic treatment of esophageal and gastric varices in cirrhotic portal hypertension[J]. Chin J Dig, 2019, 39(6): 373-375. DOI: 10.3760/cma.j.issn.0254-1432.2019.06.005.陈世耀. 肝硬化门静脉高压食管胃静脉曲张内镜治疗的问题与对策[J]. 中华消化杂志, 2019, 39(6): 373-375. DOI: 10.3760/cma.j.issn.0254-1432.2019.06.005. [9] de FRANCHIS R, Baveno Ⅵ Faculty. Expanding consensus in portal hypertension: Report of the Baveno Ⅵ Consensus Workshop: Stratifying risk and individualizing care for portal hypertension[J]. J Hepatol, 2015, 63(3): 743-752. DOI: 10.1016/j.jhep.2015.05.022. [10] ZHAO Q, HE SX, LIU YP, et al. Clinical study of endoscopic ligation, sclerotherapy and tissue glue embolization in the treatment of esophageal and gastric varicose vein bleeding[J]. J Clin Exp Med, 2021, 20(3): 279-282. DOI: 10.3969/j.issn.1671-4695.2021.03.016.赵倩, 和水祥, 刘亚萍, 等. 内镜下套扎、硬化剂及组织胶栓塞联合治疗食管胃底静脉曲张出血的临床研究[J]. 临床和实验医学杂志, 2021, 20(3): 279-282. DOI: 10.3969/j.issn.1671-4695.2021.03.016. [11] DENG SM, ZHANG JX, QI Y, et al. Application of endoscopic ligation in esophageal varices and study on high risk factors of postoperative rebleeding[J]. Clin J Med Offic, 2021, 49(6): 718-720. DOI: 10.16680/j.1671-3826.2021.06.43.邓水苗, 张嘉星, 齐晔, 等. 内镜下套扎术在食管静脉曲张中应用及其术后再出血高危因素研究[J]. 临床军医杂志, 2021, 49(6): 718-720. DOI: 10.16680/j.1671-3826.2021.06.43. [12] LI BM, ZHU X, SHU X, et al. Endoscopic variceal ligation plus sclerotherapy for esophageal variceal bleeding[J]. Chin J Dig Endosc, 2013, 30(2): 67-70. DOI: 10.3760/cma.j.issn.1007-5232.2013.02.003.李弼民, 朱萱, 舒徐, 等. 肝硬化食管静脉曲张破裂出血序贯治疗的临床应用价值[J]. 中华消化内镜杂志, 2013, 30(2): 67-70. DOI: 10.3760/cma.j.issn.1007-5232.2013.02.003. [13] CHEN J, ZENG XQ, MA LL, et al. Randomized controlled trial comparing endoscopic ligation with or without sclerotherapy for secondary prophylaxis of variceal bleeding[J]. Eur J Gastroenterol Hepatol, 2016, 28(1): 95-100. DOI: 10.1097/MEG.0000000000000499. [14] VUACHET D, CERVONI JP, VUITTON L, et al. Improved survival of cirrhotic patients with variceal bleeding over the decade 2000-2010[J]. Clin Res Hepatol Gastroenterol, 2015, 39(1): 59-67. DOI: 10.1016/j.clinre.2014.06.018. [15] CHEN XL, CHEN TW, ZHANG XM, et al. Platelet count combined with right liver volume and spleen volume measured by magnetic resonance imaging for identifying cirrhosis and esophageal varices[J]. World J Gastroenterol, 2015, 21(35): 10184-10191. DOI: 10.3748/wjg.v21.i35.10184. [16] ZHANG Y, DING HG. Risk factors for early rebleeding after endoscopic therapy for esophageal varices in cirrhotic patients[J]. J Clin Hepatol, 2021, 37(9): 2087-2091. DOI: 10.3969/j.issn.1001-5256.2021.09.017.张妍, 丁惠国. 肝硬化食管静脉曲张内镜治疗术后早期再出血的危险因素分析[J]. 临床肝胆病杂志, 2021, 37(9): 2087-2091. DOI: 10.3969/j.issn.1001-5256.2021.09.017. [17] TRIANTOS C, KALAFATELI M. Endoscopic treatment of esophageal varices in patients with liver cirrhosis[J]. World J Gastroenterol, 2014, 20(36): 13015-13026. DOI: 10.3748/wjg.v20.i36.13015. [18] MOSTAFA EF, MOHAMMAD AN. Incidence and predictors of rebleeding after band ligation of oesophageal varices[J]. Arab J Gastroenterol, 2014, 15(3-4): 135-141. DOI: 10.1016/j.ajg.2014.10.002. [19] JIN Y, WANG X, ZHANG LJ, et al. Risk factors for early rebleeding after esophageal variceal ligation in patients with liver cirrhosis[J]. J Clin Hepatol, 2017, 33 (11): 2147-2151. DOI: 10.3969/j.issn.1001-5256.2017.11.019.金燕, 王雪, 张玲娟, 等. 肝硬化患者食管静脉曲张套扎术后早期再出血的危险因素分析[J]. 临床肝胆病杂志, 2017, 33(11): 2147-2151. DOI: 10.3969/j.issn.1001-5256.2017.11.019. [20] ZHANG S, YU JH, XU GL. Advances in hemodynamics of portal hypertension[J]. J Hepatobiliary Surg, 2013, 21(3): 230-232. DOI: 10.3969/j.issn.1006-4761.2013.03.025.张硕, 余继海, 许戈良. 门静脉高压症血流动力学研究进展[J]. 肝胆外科杂志, 2013, 21(3): 230-232. DOI: 10.3969/j.issn.1006-4761.2013.03.025. [21] LI YF, LIU LJ, CHENG X, et al. The risk factors of esophageal variceal bleeding in patients with liver cirrhosis[J]. Pract J Clin Med, 2019, 16(1): 41-44. DOI: 10.3969/j.issn.1672-6170.2019.01.014.李艳芳, 刘灵军, 程星, 等. 肝硬化食管静脉曲张破裂出血危险因素分析[J]. 实用医院临床杂志, 2019, 16(1): 41-44. DOI: 10.3969/j.issn.1672-6170.2019.01.014. [22] YANG HR. Value of color Doppler ultrasound in the diagnosis of portal hypertension liver cirrhosis merged with esophageal variceal bleeding[J]. J Hainan Med Univ, 2016, 22(5): 496-498. DOI: 10.13210/j.cnki.jhmu.20151203.007.杨海荣. 彩色多普勒超声在肝硬化门脉高压食管静脉曲张破裂出血中的价值[J]. 海南医学院学报, 2016, 22(5): 496-498. DOI: 10.13210/j.cnki.jhmu.20151203.007. -



 PDF下载 ( 2091 KB)
PDF下载 ( 2091 KB)

 下载:
下载:


