磁共振IDEAL-IQ技术对急性胰腺炎患者脂肪与铁沉积的诊断效能分析
DOI: 10.3969/j.issn.1001-5256.2022.10.022
Efficacy of magnetic resonance IDEAL-IQ technique in diagnosis of fat and iron deposition in acute pancreatitis
-
摘要:
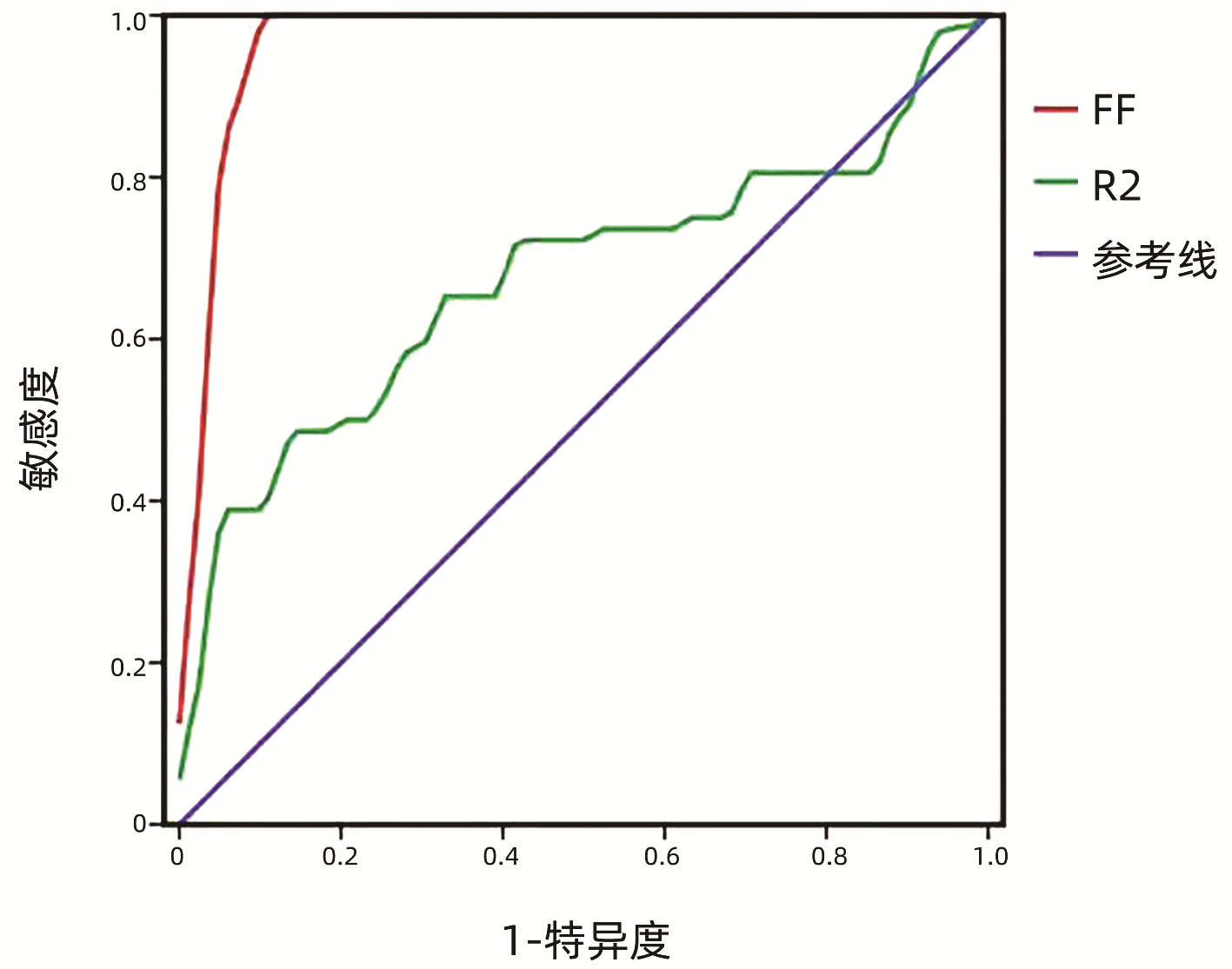
目的 利用IDEAL-IQ技术定量参数脂肪分量(FF)和弛豫率(R2*)对急性胰腺炎(AP)患者胰腺内脂肪沉积和铁沉积进行量化评估,评价其诊断AP的效能。 方法 纳入2020年10月—2021年10月于内蒙古科技大学包头医学院第一附属医院诊治的AP患者72例为AP组,以同期82例健康体检者为对照组。两组研究对象应用GE 3.0T MRI行腹部IDEAL-IQ序列检查,并在MR后处理工作站测量胰腺FF及R2*值。符合正态性分布的计量资料两组间比较采用t检验;不符合正态分布的计量资料两组间比较采用非参数Mann-Whitney U检验。差异有统计学意义的参数进行受试者工作特征曲线分析。以曲线下面积作为评价参数诊断效能的指标。 结果 病例组中FF值显著高于对照组(Z=-10.01,P<0.001),AP组中R2*值高于对照组,差异有统计学意义(Z=-3.73,P<0.001);而轻度与中重度AP间FF和R2*值的差异均无统计学意义(P值均>0.05);FF值和R2*值诊断AP的敏感度分别为100%、48.6%,特异度分别为90.2%、86.6%。 结论 磁共振IDEAL-IQ技术定量参数FF值诊断AP的灵敏度和特异度均较高,是诊断AP的特异性指标,具有很好的临床应用前景。 Abstract:Objective To perform quantitative evaluation of fat and iron deposition in the pancreas of patients with acute pancreatitis (AP) based on the IDEAL-IQ quantitative parameters fat fraction (FF) and relaxation rate (R2*), and to investigate the efficacy of this technique in the diagnosis of AP. Methods A total of 72 patients with AP who were diagnosed and treated in The First Affiliated Hospital of Baotou Medical College, Inner Mongolia University of Science and Technology from October 2020 to October 2021, were enrolled as case group, and 82 healthy controls who underwent physical examination during the same period of time were enrolled as control group. The abdominal IDEAL-IQ sequence test was performed for both groups using GE 3.0T magnetic resonance instrument, and FF and R2* values were measured on post-processing workstation. The t-test was used for comparison of normally distributed continuous data between groups, and the Mann-Whitney U test was used for comparison of non-normally distributed continuous data between groups. A receiver operating characteristic (ROC) curve analysis was performed for the parameters with statistical significance, and area under the ROC curve (AUC) was used to evaluate the diagnostic efficacy of parameters. Results Compared with the control group, the case group had significantly higher FF value (Z=-10.01, P < 0.001) and R2* value (Z=-3.73, P < 0.001), while there were no significant differences in FF and R2* values between mild AP and moderate-to-severe AP (P > 0.05). FF value had a sensitivity of 100% and a specificity of 90.2% in the diagnosis of AP, while R2* value had a sensitivity of 48.6% and a specificity of 86.6% in the diagnosis of AP. Conclusion The quantitative parameter FF value of magnetic resonance IDEAL-IQ technique has relatively high sensitivity and specificity in the diagnosis of AP, and it is a specific index for the diagnosis of AP and holds promise for clinical application. -
Key words:
- Pancreatitis /
- IDEAL-IQ /
- Fat Deposition /
- Iron Deposition
-
表 1 MRSI评分标准
Table 1. MRSI scoring system
MRI表现 评分 胰腺炎症评分 未见明显异常 0 局灶性或弥漫性胰腺增大 1 腺体内信号异常伴胰周脂肪炎性改变 2 单处的、无明确边界的积液或蜂窝组织炎块 3 2处或2处以上无明确边界的积液或积气 4 胰腺坏死评分1) 无坏死 0 <30% 2 30%~50% 4 >50% 6 注:MRSI=胰腺炎症评分+坏死评分;1)胰腺坏死的判断标准,T1WI呈低信号,T2WI呈低信号或高信号,增强扫描动脉期、静脉期图像均未见明显强化。 表 2 腹部MRI平扫及增强扫描主要参数
Table 2. Main parameters of abdominal MRI plain scan and enhanced scan
项目 扫描序列 TR(ms) TE(ms) FOV(cm) 层厚(mm) 翻转角 MRI平扫 T1WI轴位 快速干扰相梯度回波序列 4.2 1.1/2.2 40×32 5 15° T2WI轴位 单次激发快速自旋回波序列 7500 76.1 40×40 7 110° T2WI抑脂 快速恢复自旋回波饱和脂肪抑制序列 9000 76.1 40×40 7 110° T2WI冠位 单次激发快速自旋回波序列 2211 76.1 42×42 6 90° MRI增强 肝脏快速容积成像序列 3.5 1.3 40×32 5 15° 注:TR,重复时间;TE,回波时间;FOV,视野。所有受试者在屏气状态下行IDEAL-IQ序列扫描,扫描参数为TR 6.6 ms,TE 0.9~4.8 ms,激励次数0.50,FOV 44 cm×44 cm,层厚8 mm,相位数160,翻转角3°,扫描时间18 s。 表 3 病例组与对照组FF及R2*值的比较
Table 3. Comparison of FF and R2* between the case and control group
参数 AP组(n=72) 对照组(n=82) Z值 P值 FF(%) 9.23(7.51~12.33) 3.02(2.00~3.85) -10.01 <0.001 R2*(Hz) 37.05(25.33~53.56) 28.18(23.85~35.53) -3.73 <0.001 表 4 轻度与中重度AP患者胰腺FF及R2*值的比较
Table 4. Comparison of pancreatic FF and R2* values between mild group and moderately severe to severe group of AP patients
参数 轻度(n=50) 中重度(n=22) Z值 P值 FF(%) 9.80(7.44~12.75) 8.30(7.88~10.32) -1.032 0.299 R2*(Hz) 39.27(27.44~53.62) 33.22(23.96~54.97) -0.274 0.741 -
[1] LANKISCH PG, APTE M, BANKS PA. Acute pancreatitis[J]. Lancet, 2015, 386(9988): 85-96. DOI: 10.1016/S0140-6736(14)60649-8. [2] Chinese Society for Emergency Medicine; Beijing-Tianjin-Hebei Alliance of Emergency Treatment and First Aid; Emergency Medicine Branch, Beijing Medical Association, et al. Expert consensus on emergency diagnosis and treatment of acute pancreatits[J]. J Clin Hepatol, 2021, 37(5): 1034-1041. DOI: 10.3969/j.issn.1001-5256.2021.05.012.中华医学会急诊分会, 京津冀急诊急救联盟, 北京医学会急诊分会, 等. 急性胰腺炎急诊诊断及治疗专家共识[J]. 临床肝胆病杂志, 2021, 37(5): 1034-1041. DOI: 10.3969/j.issn.1001-5256.2021.05.012. [3] QUICLET C, DITTBERNER N, GÄSSLER A, et al. Pancreatic adipocytes mediate hypersecretion of insulin in diabetes-susceptible mice[J]. Metabolism, 2019, 97: 9-17. DOI: 10.1016/j.metabol.2019.05.005. [4] YAMAZAKI H, TSUBOYA T, KATANUMA A, et al. Lack of independent association between fatty pancreas and incidence of type 2 diabetes: 5-year Japanese cohort study[J]. Diabetes Care, 2016, 39(10): 1677-1683. DOI: 10.2337/dc16-0074. [5] WONG VW, WONG GL, YEUNG DK, et al. Fatty pancreas, insulin resistance, and β-cell function: a population study using fat-water magnetic resonance imaging[J]. Am J Gastroenterol, 2014, 109(4): 589-597. DOI: 10.1038/ajg.2014.1. [6] ALEMPIJEVIC T, DRAGASEVIC S, ZEC S, et al. Non-alcoholic fatty pancreas disease[J]. Postgrad Med J, 2017, 93(1098): 226-230. DOI: 10.1136/postgradmedj-2016-134546. [7] ACHARYA C, CLINE RA, JALIGAMA D, et al. Fibrosis reduces severity of acute-on-chronic pancreatitis in humans[J]. Gastroenterology, 2013, 145(2): 466-475. DOI: 10.1053/j.gastro.2013.05.012. [8] REEDER SB, PINEDA AR, WEN Z, et al. Iterative decomposition of water and fat with echo asymmetry and least-squares estimation (IDEAL): application with fast spin-echo imaging[J]. Magn Reson Med, 2005, 54(3): 636-644. DOI: 10.1002/mrm.20624. [9] XIONG XQ, LIN QT, SITU DK, et al. Application of new magnetic resonance water-fat separation technology IDEAL-IQ[J]. J Jinan Univ (Natural Science and Medicine Edition), 2020, 41(5): 427-433. DOI: 10.11778/j.jdxb.2020.05.007.熊晓晴, 林绮婷, 司徒定坤, 等. 磁共振水脂分离新技术IDEAL-IQ的应用[J]. 暨南大学学报(自然科学与医学版), 2020, 41(5): 427-433. DOI: 10.11778/j.jdxb.2020.05.007. [10] SERAI SD, DILLMAN JR, TROUT AT. Proton density fat fraction measurements at 1.5- and 3-T hepatic MR imaging: Same-day agreement among readers and across two imager manufacturers[J]. Radiology, 2017, 284(1): 244-254. DOI: 10.1148/radiol.2017161786. [11] WILDMAN-TOBRINER B, MIDDLETON MM, MOYLAN CA, et al. Association between magnetic resonance imaging-proton density fat fraction and liver histology features in patients with nonalcoholic fatty liver disease or nonalcoholic steatohepatitis[J]. Gastroenterology, 2018, 155(5): 1428-1435. DOI: 10.1053/j.gastro.2018.07.018. [12] BANKS PA, BOLLEN TL, DERVENIS C, et al. Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus[J]. Gut, 2013, 62(1): 102-111. DOI: 10.1136/gutjnl-2012-302779. [13] TANG W, ZHANG XM, XIAO B, et al. Magnetic resonance imaging versus Acute Physiology And Chronic Healthy Evaluation Ⅱ score in predicting the severity of acute pancreatitis[J]. Eur J Radiol, 2011, 80(3): 637-642. DOI: 10.1016/j.ejrad.2010.08.020. [14] NIU CY, WU FX. Research status of fatty pancreas[J]. World J Chin Dig, 2018, 26(21): 1280-1288. DOI: 10.11569/wcjd.v26.i21.1280牛春燕, 吴方雄. 脂肪胰的研究现状[J]. 世界华人消化杂志, 2018, 26(21): 1280-1288. DOI: 10.11569/wcjd.v26.i21.1280. [15] ZENG XP, HU LH, LI ZS. Research progress of fatty pancreas[J]. Chin J Pancreatol, 2016, 16(1): 68-72. DOI: 10.3760/cma.J.issn.1674-1935.2016.01.022.曾祥鹏, 胡良皞, 李兆申. 脂肪胰的研究进展[J]. 中华胰腺病杂志, 2016, 16(1): 68-72. DOI: 10.3760/cma.J.issn.1674-1935.2016.01.022. [16] SMITS MM, VAN GEENEN EJ. The clinical significance of pancreatic steatosis[J]. Nat Rev Gastroenterol Hepatol, 2011, 8(3): 169-177. DOI: 10.1038/nrgastro.2011.4. [17] NAVINA S, ACHARYA C, DELANY JP, et al. Lipotoxicity causes multisystem organ failure and exacerbates acute pancreatitis in obesity[J]. Sci Transl Med, 2011, 3(107): 107ra110. DOI: 10.1126/scitranslmed.3002573. [18] ACHARYA C, NAVINA S, SINGH VP. Role of pancreatic fat in the outcomes of pancreatitis[J]. Pancreatology, 2014, 14(5): 403-408. DOI: 10.1016/j.pan.2014.06.004. [19] KANG GH, CRUITE I, SHIEHMORTEZA M, et al. Reproducibility of MRI-determined proton density fat fraction across two different MR scanner platforms[J]. J Magn Reson Imaging, 2011, 34(4): 928-934. DOI: 10.1002/jmri.22701. [20] HUANG MY, CHENG JL, LYU XT, et al. IDEAL-IQ and MRS in quantitative assessment of liver fat content[J]. Radiol Pract, 2017, 32(5): 447-450. DOI: 10.13609/j.cnki.1000-0313.2017.05.004.黄梦月, 程敬亮, 吕晓婷, 等. IDEAL-IQ与MRS定量测量肝脏脂肪含量的可行性及相关性[J]. 放射学实践, 2017, 32(5): 447-450. DOI: 10.13609/j.cnki.1000-0313.2017.05.004. [21] LIU ML, HUANG XH, XU HX, et al. Potential role of IDEAL-IQ sequence for quantitative assessment of fat and iron deposition in pancreas with acute pancreatitis[J]. Radiol Pract, 2018, 33(12): 1266-1271. DOI: 10.13609/j.cnki.1000-0313.2018.12.008.刘梦苓, 黄小华, 徐红霞, 等. 磁共振IDEAL-IQ序列对急性胰腺炎状态下胰腺脂肪沉积和铁沉积的评估[J]. 放射学实践, 2018, 33(12): 1266-1271. DOI: 10.13609/j.cnki.1000-0313.2018.12.008. [22] GUO RM, TANG WJ, ZHU YQ, et al. Diagnostic value of MRI IDEAL-IQ sequence to hepatic steatosis and hepatic iron-overloaded[J]. J Sun Yat-Sen Univ (Medical Sciences), 2015, 36(5): 689-692. DOI: 10.13471/j.cnki.j.sun.yat-sen.univ(med.sci).2015.0111.郭若汨, 唐文杰, 朱叶青, 等. 磁共振IDEAL-IQ序列对肝脏脂肪变性和铁过载的诊断价值[J]. 中山大学学报(医学科学版), 2015, 36(5): 689-692. DOI: 10.13471/j.cnki.j.sun.yat-sen.univ(med.sci).2015.0111. [23] MORAN RA, GARCÍA-RAYADO G, DE LA IGLESIA-GARCÍA D, et al. Influence of age, body mass index and comorbidity on major outcomes in acute pancreatitis, a prospective nation-wide multicentre study[J]. United European Gastroenterol J, 2018, 6(10): 1508-1518. DOI: 10.1177/2050640618798155. [24] SZENTESI A, PÁRNICZKY A, VINCZE Á, et al. Multiple hits in acute pancreatitis: components of metabolic syndrome synergize each other's deteriorating effects[J]. Front Physiol, 2019, 10: 1202. DOI: 10.3389/fphys.2019.01202. [25] ZHANG ZC, LIN QS, HUANG YC, et al. Application of high field MR IDEAL-IQ in acute pancreatitis[J]. J Clin Radiol, 2018, 37(12): 2006-2009. DOI: 10.13437/j.cnki.jcr.2018.12.014.张志诚, 林钱森, 黄永础, 等. 高场磁共振IDEAL-IQ技术在急性胰腺炎中的应用价值研究[J]. 临床放射学杂志, 2018, 37(12): 2006-2009. DOI: 10.13437/j.cnki.jcr.2018.12.014. -



 PDF下载 ( 2190 KB)
PDF下载 ( 2190 KB)


 下载:
下载: