吲哚菁绿荧光显影在困难胆囊腹腔镜胆囊切除术中的应用价值
DOI: 10.3969/j.issn.1001-5256.2022.11.019
Application value of indocyanine green fluorescence imaging in laparoscopic cholecystectomy of difficult gallbladder
-
摘要:
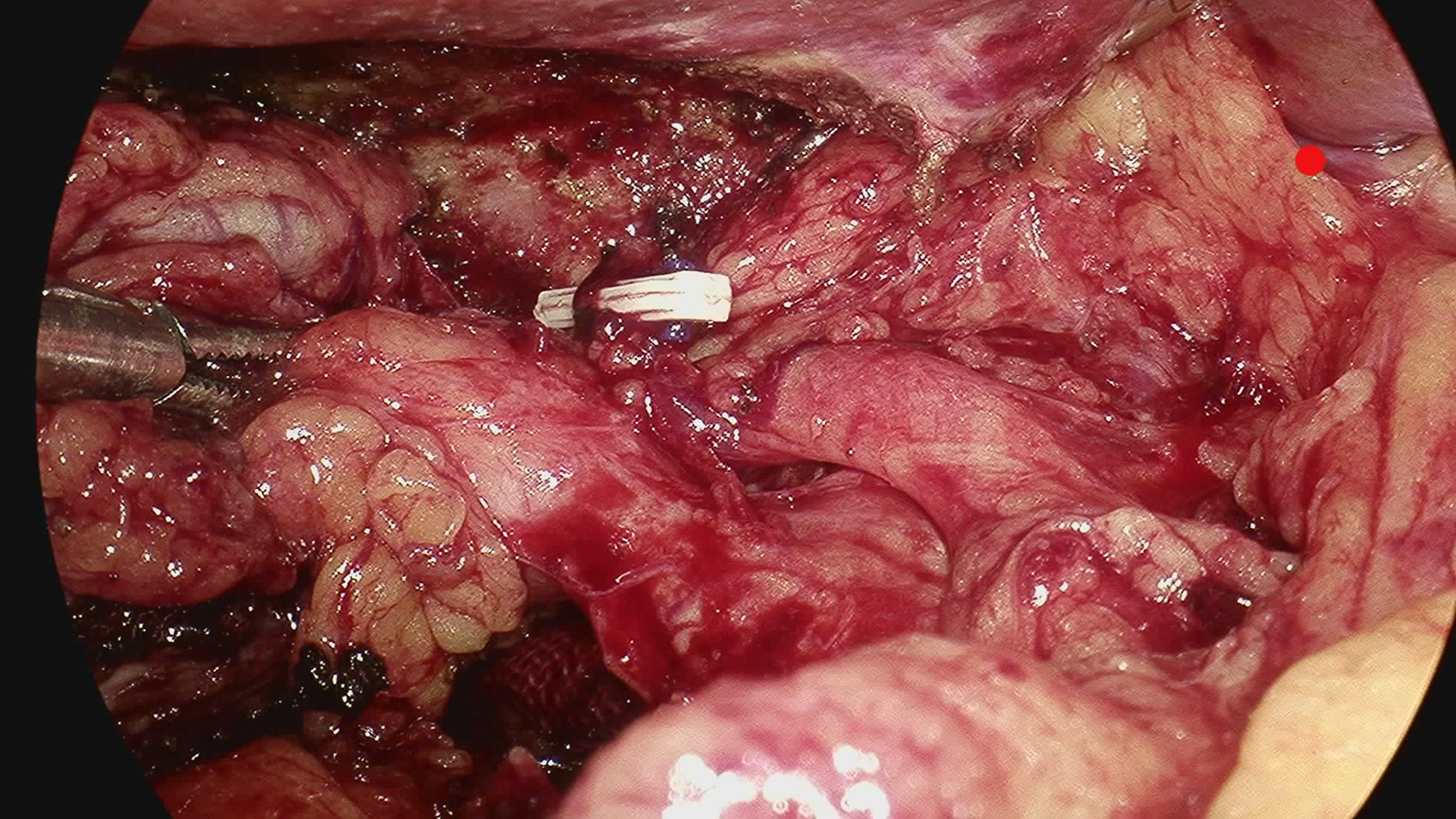
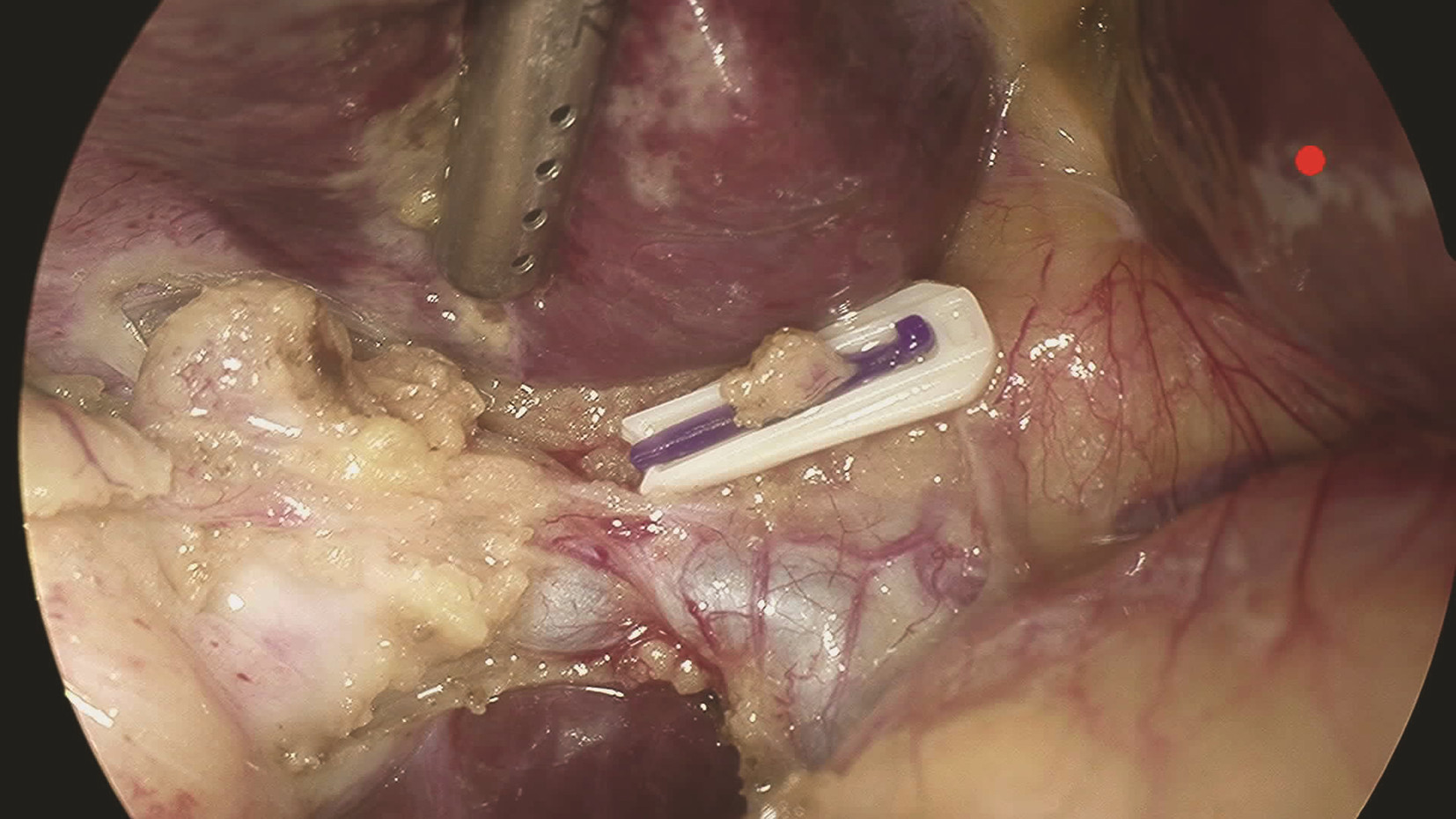
目的 探讨吲哚菁绿(ICG)荧光显影在困难胆囊腹腔镜胆囊切除术(LC)中的应用价值。 方法 回顾性分析安徽医科大学第一附属医院2021年10月—12月行LC的患者临床资料,根据术中是否使用ICG荧光显影和是否为困难胆囊分为4组:A组为使用ICG荧光显影普通胆囊,B组为使用ICG荧光显影困难胆囊,C组为未使用ICG荧光显影普通胆囊,D组为未使用ICG荧光显影困难胆囊。比较各组手术时间、术中出血、住院时间、住院费用和术后并发症间的差异。正态分布的计量资料2组间比较采用t检验。计数资料2组间比较用χ2检验或Fisher确切概率法。 结果 A组与C组相比手术时间、术中出血、住院时间、住院费用和术中并发症,差异均无统计学意义(P值均>0.05)。B组手术时间和术中出血分别为(75.41±12.96)min和(18.27±6.97)mL,D组分别为(106.78±19.21)min和(23.99±8.43)mL,两组相比差异均有统计学意义(P值均<0.05);B组住院时间、住院费用和术后并发症与D组相比,差异均无统计学意义(P值均>0.05)。 结论 普通胆囊患者LC术中使用ICG荧光显影优势不明显;但在困难胆囊中,ICG荧光显影有利于胆道显露,可以缩短手术时间,减少术中出血。ZHANG Chao -
关键词:
- 胆囊切除术, 腹腔镜 /
- 吲哚花青绿 /
- 治疗结果
Abstract:Objective To investigate the clinical utility of indocyanine green (ICG) fluorescence imaging in difficult laparoscopic cholecystectomy (LC). Methods The clinical data of LC patients from October 2021 to December 2021 in the First Affiliated Hospital of Anhui Medical University were retrospectively analyzed. Based on whether ICG fluorescence imaging was used and whether gallbladder difficulties were detected, the patients were divided into four groups: ICG common gallbladder (Group A), ICG difficult gallbladder (Group B), common gallbladder (Group C), and difficult gallbladder (Group D). The operative time, intraoperative bleeding, length of hospital stay, hospitalization cost and postoperative complications were compared. Comparison of normally distributed continuous data between groups was performed by t test. Comparison of categorical data between groups was performed using the chi-square test or Fisher's exact probability method. Results The operative time, intraoperative bleeding, length of hospital stay, hospitalization cost and intraoperative complications in group A were comparable to those in Group C (all P > 0.05). The operative time and intraoperative bleeding were (75.41±12.96) min and (18.27±6.97) mL in group B, vs (106.78±19.21) min and (23.99±8.43) mL in group D, respectively, and the differences were statistically significant (all P < 0.05), while the length of hospitalization, hospitalization cost and postoperative complications in group B were comparable to those in group D (all P > 0.05). Conclusion The benefits of ICG fluorescence imaging during LC in patients with the common gallbladder are not obvious. However, in difficult gallbladder cases, ICG fluorescence imaging can improve biliary tract exposure and reduce operation time and intraoperative bleeding. -
Key words:
- Cholecystectomy, Laparoscopic /
- Indocyanine Green /
- Treatment Outcome
-
表 1 患者一般资料比较
Table 1. Comparison of general data of patients
组别 例数 性别(例) 年龄(岁) 合并症
(例)男 女 A组 49 18 31 55.29±12.66 13 B组 44 19 25 48.59±14.88 10 C组 45 10 35 52.98±12.76 8 D组 37 16 21 50.95±13.62 10 表 2 A、C组患者手术相关指标比较
Table 2. Comparison of surgical indicators in group A and C
组别 例数 手术时间(min) 住院时间(d) 术中出血(mL) 住院费用(元) A组 49 47.16±9.79 2.51±1.00 9.63±2.60 10 163.70±1 040.61 C组 45 49.24±9.45 2.58±1.37 9.49±2.90 9 901.79±1 044.43 t值 1.047 0.274 0.253 1.218 P值 0.298 0.785 0.801 0.226 表 3 B、D组患者手术相关指标比较
Table 3. Comparison of surgical indicators in group B and D
组别 例数 手术时间(min) 住院时间(d) 术中出血(mL) 住院费用(元) 三孔法/四孔法(例) B组 44 75.41±12.96 2.82±1.24 18.27±6.97 10 124.12±915.56 30/14 D组 37 106.78±19.21 3.27±1.73 23.99±8.43 10 578.99±1 404.03 15/22 统计值 t=8.729 t=1.366 t=3.300 t=1.691 χ2=6.219 P值 <0.001 0.176 0.001 0.096 0.013 -
[1] NI ZP, ZHANG XH, LIU YS. Discussion on the application value of indocyanine green fluorescence staining in laparoscopic cholecystectomy[J]. J Abdom Surg, 2020, 33(3): 212-217. DOI: 10.3969/j.issn.1003-5591.2020.03.011.倪忠鹏, 张昕辉, 刘养岁. 吲哚菁绿荧光染色技术在腹腔镜胆囊切除术中的价值分析[J]. 腹部外科, 2020, 33(3): 212-217. DOI: 10.3969/j.issn.1003-5591.2020.03.011. [2] LIU XL, LI HY, BAO Q, et al. MRCP study on the correlation between gallbladder stones and different types of gallbladder duct variation[J]. Chin J CT MRI, 2019, 17(10): 75-78. DOI: 10.3969/j.issn.1672-5131.2019.10.025.刘新亮, 李洪义, 包权, 等. 胆囊管变异不同类型与胆囊结石相关性的MRCP研究[J]. 中国CT和MRI杂志, 2019, 17(10): 75-78. DOI: 10.3969/j.issn.1672-5131.2019.10.025. [3] YAMASHITA M, KUROKI T, HAMADA T, et al. Evaluation of preoperative magnetic resonance cholangiopancreatography in acute cholecystitis to predict technical difficulties in laparoscopic cholecystectomy[J]. Acta Med Okayama, 2021, 75(6): 685-689. DOI: 10.18926/AMO/62807. [4] OMIYA K, HIRAMATSU K, SHIBATA Y, et al Preoperative magnetic resonance cholangiopancreatography for detecting difficult laparoscopic cholecystectomy in acute cholecystitis[J]. Diagnostics (Basel), 2021, 11(3): 383. DOI: 10.3390/diagnostics11030383. [5] XU XL, MENG FK, ZHENG Y, et al. Application of indocyanine green excretion test and liver stiffness measurement before surgery of hepatocellular carcinoma[J]. Chin Hepatol, 2020, 25(3): 264-266, 281. DOI: 10.3969/j.issn.1008-1704.2020.03.011.徐晓鸾, 孟繁坤, 郑颖, 等. ICG清除试验及肝脏弹性值在肝癌术前的应用研究[J]. 肝脏, 2020, 25(3): 264-266, 281. DOI: 10.3969/j.issn.1008-1704.2020.03.011. [6] WANG Z, YUE ZD, ZHAO HW, et al. Value of indocyanine green retention rate at 15 minutes in predicting the risk of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt in liver cancer patients with portal hypertension[J]. J Clin Hepatol, 2020, 36(9): 1994-1997. DOI: 10.3969/j.issn.1001-5256.2020.09.017.王重, 岳振东, 赵洪伟, 等. 吲哚菁绿15分钟滞留率对肝癌合并门静脉高压症患者经颈静脉肝内门体分流术后肝性脑病发生风险的预测价值[J]. 临床肝胆病杂志, 2020, 36(9): 1994-1997. DOI: 10.3969/j.issn.1001-5256.2020.09.017. [7] LIU S, YIN XM, LIU Y, et al. Safety and feasibility analysis of ICG fluorescence imaging laparoscopic anatomical right hepatectomy in the treatment of liver neoplasms[J]. Chin J Prac Surg, 2019, 39(9): 944-948. DOI: 10.19538/j.cjps.issn1005-2208.2019.09.15.刘胜, 尹新民, 刘毅, 等. ICG荧光显影引导腹腔镜解剖性右半肝切除治疗肝脏肿瘤安全性及可行性研究[J]. 中国实用外科杂志, 2019, 39(9): 944-948. DOI: 10.19538/j.cjps.issn1005-2208.2019.09.15. [8] XIA XG, ZHOU P, LU C, et al. Effect of ICG imaging guidance on laparoscopic surgery in patients with recurrent liver cancer[J]. Clin J Med Offic, 2021, 49(11): 1248-1249, 1252. DOI: 10.16680/j.1671-3826.2021.11.22.夏喜刚, 周鹏, 卢超, 等. ICG显像引导对复发性肝癌患者腹腔镜手术治疗效果影响[J]. 临床军医杂志, 2021, 49(11): 1248-1249, 1252. DOI: 10.16680/j.1671-3826.2021.11.22. [9] ZHANG W, ZHU W, YANG J, et al. Augmented reality navigation for stereoscopic laparoscopic anatomical hepatectomy of primary liver cancer: preliminary experience[J]. Front Oncol, 2021, 11: 663236. DOI: 10.3389/fonc.2021.663236. eCollection 2021. [10] ZHANG P, LUO H, ZHU W, et al. Real-time navigation for laparoscopic hepatectomy using image fusion of preoperative 3D surgical plan and intraoperative indocyanine green fluorescence imaging[J]. Surg Endosc, 2020, 34(8): 3449-3459. DOI: 10.1007/s00464-019-07121-1. [11] SHANG XG, ZHANG XM, YUE XJ, et al. An differential analysis of the effects of nanocarbon and ICG fluorescence on lymph node dissection and parathyroid protection during thyroid carcinoma surgery[J]. Lab Immun Clin Med, 2020, 27(3): 423-427, 431. DOI: 10.11748/bjmy.issn.1006-1703.2020.03.014.尚兴国, 张雪棉, 岳秀杰, 等. 纳米炭与吲哚箐绿荧光两种示踪法对甲状腺微小乳头状癌术中淋巴结清扫和甲状旁腺保护作用研究[J]. 标记免疫分析与临床, 2020, 27(3): 423-427, 431. DOI: 10.11748/bjmy.issn.1006-1703.2020.03.014. [12] CHEN QY, XIE JW, ZHONG Q, et al. Safety and efficacy of indocyanine green tracer-guided lymph node dissection during laparoscopic radical gastrectomy in patients with gastric cancer: a randomized clinical trial[J]. JAMA Surg, 2020, 155(4): 300-311. DOI: 10.1001/jamasurg.2019.6033. [13] MATSUMURA M, SEYAMA Y, ISHIDA H, et al. Indocyanine green fluorescence navigation for hepatocellular carcinoma with bile duct tumor thrombus: a case report[J]. Surg Case Rep, 2021, 7(1): 18. DOI: 10.1186/s40792-020-01101-7. [14] CALABRO KA, HARMON CM, VALI K. Fluorescent cholangiography in laparoscopic cholecystectomy and the use in pediatric patients[J]. J Laparoendosc Adv Surg Tech A, 2020, 30(5): 586-589. DOI: 10.1089/lap.2019.0204. [15] LIM SH, TAN HTA, SHELAT VG. Comparison of indocyanine green dye fluorescent cholangiography with intra-operative cholangiography in laparoscopic cholecystectomy: a meta-analysis[J]. Surg Endosc, 2021, 35(4): 1511-1520. DOI: 10.1007/s00464-020-08164-5. [16] WANG C, WU SD, LYU C, et al. Optimal preoperative timing of indocyanine green administration for laparoscopic cholecystectomy under fluorescence navigation[J]. Chin J Hepatobiliary Surg, 2020, 26(9): 695-698. DOI: 10.3760/cma.j.cn113884-20200113-00029.汪聪, 吴硕东, 吕超, 等. 荧光导航腹腔镜胆囊切除患者吲哚菁绿最佳术前注射时机分析[J]. 中华肝胆外科杂志, 2020, 26(9): 695-698. DOI: 10.3760/cma.j.cn113884-20200113-00029. [17] WANG XN, WU SD, DENG TL, et al. Application of indolyanine green fluorescent cholangiography in laparoscopic cholecystectomy[J]. J Laparo Surg, 2021, 26(7): 550-554. DOI: 10.13499/j.cnki.fqjwkzz.2021.07.550.王潇宁, 吴硕东, 邓天麟, 等. 吲哚菁绿荧光胆道造影在腹腔镜胆囊切除术中的应用[J]. 腹腔镜外科杂志, 2021, 26(7): 550-554. DOI: 10.13499/j.cnki.fqjwkzz.2021.07.550. [18] BRODERICK RC, LEE AM, CHEVERIE JN, et al. Fluorescent cholangiography significantly improves patient outcomes for laparoscopic cholecystectomy[J]. Surg Endosc, 2021, 35(10): 5729-5739. DOI: 10.1007/s00464-020-08045-x. [19] ESPOSITO C, ALBERTI D, SETTIMI A, et al. Indocyanine green (ICG) fluorescent cholangiography during laparoscopic cholecystectomy using RUBINATM technology: preliminary experience in two pediatric surgery centers[J]. Surg Endosc, 2021, 35(11): 6366-6373. DOI: 10.1007/s00464-021-08596-7. [20] THORNBLADE LW, MELSTROM KA, ZHUMKHAWALA A, et al. Fluorescence guidance in digestive surgery[J]. Chin J Dig Surg, 2021, 20(2): 149-154. DOI: 10.3760/cma.j.cn115610-20201126-00740.LUCAS WILLIAN THORNBLADE, KURT ALLAN MELSTROM, ALI ZHUMKHAWALA, 等. 荧光显像技术在消化外科中的应用进展[J]. 中华消化外科杂志, 2021, 20(2): 149-154. DOI: 10.3760/cma.j.cn115610-20201126-00740. [21] BLESZYNSKI MS, DEGIROLAMO KM, MENEGHETTI AT, et al. Fluorescent cholangiography in laparoscopic cholecystectomy: an updated canadian experience[J]. Surg Innov, 2020, 27(1): 38-43. DOI: 10.1177/1553350619885792. [22] LAI EC, CHUNG DT, LO ST, et al. The role of indocyanine green cholangiography in minimally invasive surgery[J]. Minerva Surg, 2021, 76(3): 229-234. DOI: 10.23736/S2724-5691.21.08721-6. [23] QUARESIMA S, BALLA A, PALMIERI L, et al. Routine near infra-red indocyanine green fluorescent cholangiography versus intraoperative cholangiography during laparoscopic cholecystectomy: a case-matched comparison[J]. Surg Endosc, 2020, 34(5): 1959-1967. DOI: 10.1007/s00464-019-06970-0. [24] QIU F, ZHU RF, WU JJ. Application of low concentration of indocyanine green fluorescence imaging technique in laparoscopic cholecystectomy[J]. J Hepatobiliary Surg, 2020, 28(4): 285-287. DOI: 10.3969/j.issn.1006-4761.2020.04.014.邱烽, 朱任飞, 吴建军. 低浓度ICG在腹腔镜胆囊切除术中的应用体会[J]. 肝胆外科杂志, 2020, 28(4): 285-287. DOI: 10.3969/j.issn.1006-4761.2020.04.014. [25] KOONG JK, NG GH, RAMAYAH K, et al. Early identification of the critical view of safety in laparoscopic cholecystectomy using indocyanine green fluorescence cholangiography: A randomised controlled study[J]. Asian J Surg, 2021, 44(3): 537-543. DOI: 10.1016/j.asjsur.2020.11.002. [26] IACUZZO C, BRESSAN L, TROIAN M, et al. The added value of intraoperative near-infrared fluorescence imaging in elective laparoscopic cholecystectomy[J]. Surg Innov, 2021, 15533506211052744. DOI: 10.1177/15533506211052744.[Online ahead of print] -



 PDF下载 ( 2744 KB)
PDF下载 ( 2744 KB)

 下载:
下载: