慢性乙型肝炎患者停用核苷(酸)类似物后循环血清中HBV pgRNA、HBcrAg表达水平与复发的相关性分析
DOI: 10.3969/j.issn.1001-5256.2023.01.009
Expression levels of HBV pregenomic RNA and hepatitis B core-related antigen in circulating serum and their association with recurrence in chronic hepatitis B patients after withdrawal from nucleos(t)ide analogues
-
摘要:
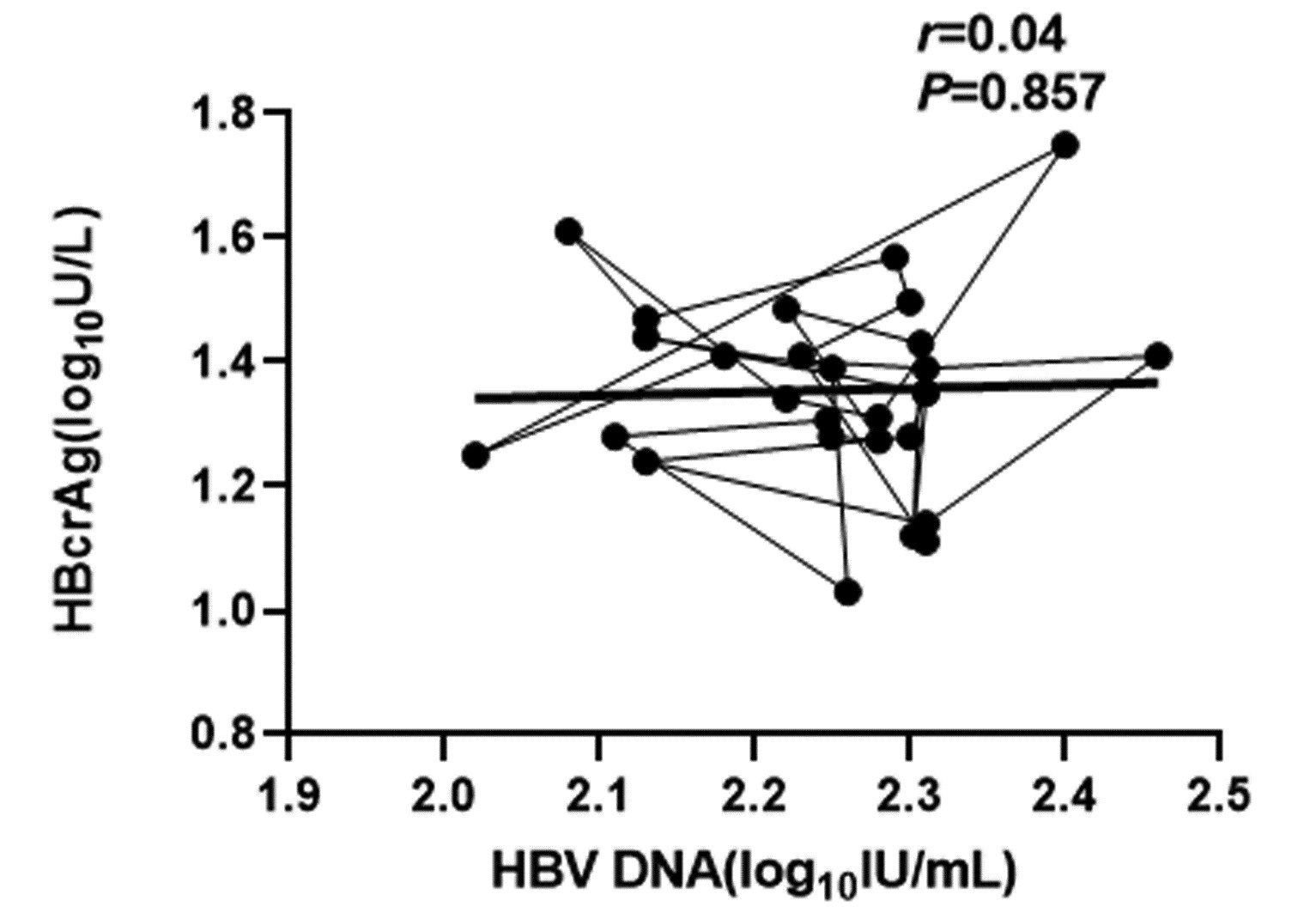
目的 检测慢性乙型肝炎(CHB)患者停用核苷(酸)类似物(NUC)后循环血清中HBV前基因组RNA(pgRNA)以及乙型肝炎核心相关抗原(HBcrAg)的表达水平,分析停药后CHB患者循环血中不同时段HBV pgRNA、HBcrAg水平与复发之间的相关性。 方法 选取2019年12月—2022年7月川北医学院附属医院门诊就诊者中抗HBV治疗至少5年到达完全应答并满足2017年版欧洲肝病学会指南停药标准的CHB患者108例,根据停药时间分为停药后4、12、24周组;根据复发情况分为复发组与未复发组。运用实时荧光定量PCR法检测CHB患者循环血清中HBV pgRNA水平,运用ELISA检测研究对象静脉血中HBcrAg的表达水平,采用实时荧光定量PCR法高精度检测HBV DNA载量。计量资料两组间比较采用t检验;多组间比较采用单因素方差分析,进一步两两比较采用LSD-t检验。采用Pearson相关检验分析循环血中各指标间的相关性。 结果 CHB患者停药后在随访4~12周时复发率17.1%,24周后累积复发率达到29.3%,其中单独HBV DNA复阳者各占64.3%、60.0%,HBeAg单独复阳者各占28.6%、20.0%,HBV DNA、HBeAg同时复阳者各占7.1%、20.0%。停药24周时,CHB患者循环血清中HBV pgRNA、HBcrAg、HBV DNA表达水平较停药时及停药后4周时明显高表达,不同时段比较差异具有统计学意义(P值均<0.05)。复发组循环血清中HBV pgRNA、HBcrAg、HBV DNA水平较未复发组显著高表达(t值分别2.549、8.654、27.429,P值均<0.05);对复发组进一步分析发现,在12~24周时复发组患者循环血清中HBV pgRNA、HBcrAg与HBV DNA水平较4~12周时高表达(P值均<0.05)。复发组停药时循环血清中HBV pgRNA、HBcrAg的表达水平较未复发组停药时显著高表达(t值分别为18.561、6.152,P值均<0.001)。相关性分析显示,CHB患者停药后复发组循环血清中HBV pgRNA、HBcrAg与HBV DNA呈正相关(r值分别为0.82、0.66,P值均<0.001);未复发组循环血清中HBV pgRNA、HBcrAg与HBV DNA均无相关性(r值分别为0.14、0.04,P值均>0.05)。 结论 停药时复发组HBV pgRNA、HBcrAg水平较未复发组高表达,提示未复发组在停药时的HBV pgRNA、HBcrAg水平可能作为CHB患者可安全停药的参考临界值指标,HBV pgRNA、HBcrAg水平检测可能是未来抗HBV治疗终点选择的潜在参考指标之一。 -
关键词:
- 慢性乙型肝炎 /
- HBV前基因组RNA /
- 乙型肝炎核心相关抗原 /
- 复发
Abstract:Objective To investigate the expression levels of HBV pregenomic RNA (pgRNA) and hepatitis B core-related antigen (HBcrAg) in circulating serum of chronic hepatitis B (CHB) patients after withdrawal from nucleos(t)ide analogues (NUC), as well as the correlation of HBV pgRNA and HBcrAg levels in circulating blood in different periods of time with recurrence in CHB patients after drug withdrawal. Methods Among the patients who attended the outpatient service of Affiliated Hospital of North Sichuan Medical College from December 2019 to July 2022, a total of 108 CHB patients who received anti-HBV therapy for at least 5 years and met the criteria for drug withdrawal in 2017 EASL Guidelines were enrolled. According to the time of drug withdrawal, the patients were divided into 4-, 12-, and 24-week groups after drug withdrawal, and according to the presence or absence of recurrence, they were divided into recurrence group and non-recurrence group. Quantitative real-time PCR was used to measure the level of HBV pgRNA in circulating serum of CHB patients; ELISA was used to measure the expression level of HBcrAg in peripheral venous blood; quantitative real-time PCR was used to measure HBV DNA load with high accuracy. The t-test was used for comparison of continuous data between two groups. A one-way analysis of variance was used for comparison of continuous data between multiple groups, and the least significant difference t-test was used for further comparison between two groups. The Pearson correlation test was used to investigate the correlation between the indices in circulating blood. Results For the CHB patients after drug withdrawal, the recurrence rate was 17.1% at 4-12 weeks, cumulative recurrence rate reached 29.3% after 24 weeks of follow-up, the patients with positive HBV DNA alone accounted for 64.3% and 60.0%, respectively, those with positive HBeAg alone accounted for 28.5% and 20.0%, respectively, and those with positive HBV DNA and HBeAg accounted for 7.1% and 20.0%, respectively. The expression levels of HBV pgRNA, HBcrAg, and HBV DNA in circulating serum of CHB patients at 24 weeks after drug withdrawal were significantly higher than those at the time of drug withdrawal and at 4 weeks after drug withdrawal, and there was a significant difference between groups at different time points (all P < 0.05). Compared with the non-recurrence group, the recurrence group had significantly higher expression levels of HBV pgRNA, HBcrAg, and HBV DNA in circulating serum (t=2.549, 8.654, and 27.429, all P < 0.05), and further analysis of the recurrence group showed that the levels of HBV pgRNA, HBcrAg, and HBV DNA in circulating serum at 12-24 weeks were significantly higher than those at 4-12 weeks (all P < 0.05). At the time of drug withdrawal, the recurrence group had significantly higher expression levels of HBV pgRNA and HBcrAg in circulating serum than the non-recurrence group (t=18.561 and 6.152, both P < 0.001). The Pearson correlation analysis showed that in the recurrence group after drug withdrawal, HBV pgRNA and HBcrAg were positively correlated with HBV DNA in circulating serum (r=0.82 and 0.66, both P < 0.001), while no such correlation was observed in the non-recurrence group (r=0.14 and 0.04, both P > 0.05). Conclusion The recurrence group had significantly higher expression levels of HBV pgRNA and HBcrAg than the non-recurrence group at the time of drug withdrawal, suggesting that the levels of HBV pgRNA and HBcrAg in the CHB patients of the non-recurrence group at the time of drug withdrawal may be used as the reference thresholds for safe drug withdrawal in CHB patients, and measurement of HBV pgRNA and HBcrAg may be one of the potential reference indicators for the selection of anti-HBV treatment endpoints in the future. -
Key words:
- Hepatitis B, Chronic /
- HBV Pregenomic RNA /
- Hepatitis B Core Related Antigen /
- Recurrence
-
表 1 CHB患者停药后随访24周内病毒学复发人数及累积复发率
Table 1. The number of viral recurrences and cumulative recurrence rate of CHB patients within 24 weeks of follow-up after drug withdrawal
组别 复发率(%) 停药4周 0 停药12周 17.1(14/82) HBV DNA复阳 64.3(9/14) HBeAg复阳 28.6(4/14) HBV DNA、HBeAg同时复阳 7.1(1/14) 停药24周 14.7(10/68) HBV DNA复阳 60.0(6/10) HBeAg复阳 20.0(2/10) HBV DNA、HBeAg同时复阳 20.0(2/10) 表 2 CHB患者停药后各时段循环血清中HBV pgRNA、HBcrAg、HBV DNA表达水平比较
Table 2. Comparison of HBV pgRNA, HBcrAg and HBV DNA expression levels in circulating serum of CHB patients at different periods after drug withdrawal
组别 例数 HBV pgRNA (log10拷贝/mL) HBcrAg (log10 U/L) HBV DNA (log10 IU/mL) 停药时 82 1.36±0.12 1.31±0.16 1.30±0.18 停药4周 82 1.37±0.10 1.31±0.17 1.61±0.20 停药12周 82 1.39±0.12 1.40±0.13 2.38±0.26 停药24周 68 1.42±0.141)2) 1.51±0.161)2) 2.50±0.351)2) F值 10.276 14.359 21.473 P值 0.022 0.013 < 0.001 注:与停药时相比,1)P<0.05;与停药4周相比,2)P<0.05。 表 3 CHB患者停药后复发组与未复发组循环血清中HBV pgRNA、HBcrAg、HBV DNA、HBsAg水平比较
Table 3. Comparison of HBV pgRNA, HBcrAg, HBV DNA and HBsAg levels in circulating serum between relapse group and non relapse group of CHB patients after drug withdrawal
组别 例数 HBV pgRNA (log10拷贝/mL) HBcrAg (log10 U/L) HBV DNA (log10 IU/mL) 复发组 24 1.49±0.15 2.02±0.11 3.74±0.39 未复发组 58 1.39±0.13 1.35±0.17 2.24±0.15 t值 2.549 8.654 25.680 P值 0.015 < 0.001 < 0.001 表 4 停药时复发组与未复发组CHB患者循环血清中HBV pgRNA、HBcrAg表达水平比较
Table 4. Comparison of HBV pgRNA, HBcrAg expression levels in circulating serum of CHB patients in relapse and non relapse groups at the time of drug withdrawal
组别 例数 HBV pgRNA (log10拷贝/mL) HBcrAg (log10 U/L) 复发组 24 1.42±0.11 1.55±0.20 未复发组 58 1.34±0.07 1.21±0.11 t值 18.561 6.152 P值 < 0.001 < 0.001 -
[1] TANG L, COVERT E, WILSON E, et al. Chronic hepatitis B infection: a review[J]. JAMA, 2018, 319(17): 1802-1813. DOI: 10.1001/jama.2018.3795. [2] BAI L, ZHANG X, KOZLOWSKI M, et al. Extracellular hepatitis B virus RNAs are heterogeneous in length and circulate as capsid-antibody complexes in addition to virions in chronic hepatitis B patients[J]. J Virol, 2018, 92(24): e00798-18. DOI: 10.1128/JVI.00798-18. [3] NING X, LUCKENBAUGH L, LIU K, et al. Common and distinct capsid and surface protein requirements for secretion of complete and genome-free hepatitis B virions[J]. J Virol, 2018, 92(14): e00272-18. DOI: 10.1128/JVI.00272-18. [4] LU L, ZHANG HY, YUENG YH, et al. Intracellular levels of hepatitis B virus DNA and pregenomic RNA in peripheral blood mononuclear cells of chronically infected patients[J]. J Viral Hepat, 2009, 16(2): 104-112. DOI: 10.1111/j.1365-2893.2008.01054.x. [5] LARSSON SB, MALMSTRÖM S, HANNOUN C, et al. Mechanisms downstream of reverse transcription reduce serum levels of HBV DNA but not of HBsAg in chronic hepatitis B virus infection[J]. Virol J, 2015, 12: 213. DOI: 10.1186/s12985-015-0447-5. [6] TANG H. The development history of new biomarkers for hepatitis B virus infection[J]. J Clin Hepatol, 2019, 35(10): 2137-2139. DOI: 10.3969/j.issn.1001-5256.2019.10.001.唐红. HBV感染"新型"生物标志物的"前世今生"[J]. 临床肝胆病杂志, 2019, 35(10): 2137-2139. DOI: 10.3969/j.issn.1001-5256.2019.10.001. [7] WANG XR, HU XJ, WANG XR, et al. Correlation between the expressions of HBV pgRNA and HBV-LP in serum and the degree of liver fibrosis in patients with chronic HBV infection[J]. Int J Virol, 2021, 28(2): 149-153. DOI: 10.3760/cma.j.issn.1673-4092.2021.02.014.王鲜茹, 胡新俊, 王雪茹, 等. 慢性HBV感染者血清HBV pgRNA、HBV-LP表达与肝脏纤维化程度的相关性研究[J]. 国际病毒学杂志, 2021, 28(2): 149-153. DOI: 10.3760/cma.j.issn.1673-4092.2021.02.014. [8] 陈来印, 齐聪幸, 安伟娜, 等. HBeAg阳性CHB患者恩替卡韦治疗中HBcrAg水平变化及其对疗效预测价值[J/CD]. 中国肝脏病杂志(电子版), 2022, 14(2): 50-56. DOI: 10.3969/j.issn.1674-7380.2022.02.008.CHEN LY, QI CX, AN WN, et al. Levels and predictive value of HBcrAg in CHB patients with HBeAg positive in treatment with entecavir[J/CD]. Chin J Liver Dis (Electronic Version), 2022, 14(2): 50-56. DOI: 10.3969/j.issn.1674-7380.2022.02.008. [9] European Association for the Study of the Liver. EASL 2017 Clinical Practice Guidelines on the management of hepatitis B virus infection[J]. J Hepatol, 2017, 67(2): 370-398. DOI: 10.1016/j.jhep.2017.03.021. [10] LIU RX, PAN XC, GENG J. Clinical value of serum HBV RNA[J]. J Clin Hepatol, 2017, 33(11): 2196-2199. DOI: 10.3969/j.issn.1001-5256.2017.11.032.刘瑞霞, 潘修成, 耿建. 血清HBV RNA检测的临床价值[J]. 临床肝胆病杂志, 2017, 33(11): 2196-2199. DOI: 10.3969/j.issn.1001-5256.2017.11.032. [11] NASSAL M. HBV cccDNA: viral persistence reservoir and key obstacle for a cure of chronic hepatitis B[J]. Gut, 2015, 64(12): 1972-1984. DOI: 10.1136/gutjnl-2015-309809. [12] CHEN EQ, FENG S, WANG ML, et al. Serum hepatitis B core-related antigen is a satisfactory surrogate marker of intrahepatic covalently closed circular DNA in chronic hepatitis B[J]. Sci Rep, 2017, 7(1): 173. DOI: 10.1038/s41598-017-00111-0. [13] WANG J, SHEN T, HUANG X, et al. Serum hepatitis B virus RNA is encapsidated pregenome RNA that may be associated with persistence of viral infection and rebound[J]. J Hepatol, 2016, 65(4): 700-710. DOI: 10.1016/j.jhep.2016.05.029. [14] LING XZ, WANG RM, SU MH, et al. Clinical significance of dynamic monitoring of serum HBV pgRNA in CHB patients treated with Nas[J]. Chin J Pract Intern Med, 2022, 42(5): 404-408. DOI: 10.19538/j.nk2022050112.零小樟, 王荣明, 苏明华, 等. 慢性乙型肝炎患者核苷酸类似物治疗中动态监测血清乙型肝炎病毒前基因组RNA的临床意义[J]. 中国实用内科杂志, 2022, 42(5): 404-408. DOI: 10.19538/j.nk2022050112. [15] HÖNER ZU SIEDERDISSEN C, RINKER F, MAASOUMY B, et al. Viral and host responses after stopping long-term nucleos(t)ide analogue therapy in HBeAg-negative chronic hepatitis B[J]. J Infect Dis, 2016, 214(10): 1492-1497. DOI: 10.1093/infdis/jiw412. [16] ZIMMER CL, RINKER F, HÖNER ZU SIEDERDISSEN C, et al. Increased NK cell function after cessation of long-term nucleos(t)ide analogue treatment in chronic hepatitis B is associated with liver damage and HBsAg loss[J]. J Infect Dis, 2018, 217(10): 1656-1666. DOI: 10.1093/infdis/jiy097. [17] LIAO H, LIU Y, LI X, et al. Monitoring of serum HBV RNA, HBcrAg, HBsAg and anti-HBc levels in patients during long-term nucleoside/nucleotide analogue therapy[J]. Antivir Ther, 2019, 24(2): 105-115. DOI: 10.3851/IMP3280. [18] BUTLER EK, GERSCH J, MCNAMARA A, et al. Hepatitis B virus serum DNA and RNA levels in nucleos(t)ide analog-treated or untreated patients during chronic and acute infection[J]. Hepatology, 2018, 68(6): 2106-2117. DOI: 10.1002/hep.30082. -



 PDF下载 ( 2010 KB)
PDF下载 ( 2010 KB)


 下载:
下载: