第三代头孢菌素治疗社区获得性自发性细菌性腹膜炎效果预测模型的临床价值
DOI: 10.12449/JCH240214
Clinical application value of a predictive model for the efficacy of third-generation cephalosporin in treatment of community-acquired spontaneous bacterial peritonitis
-
摘要:
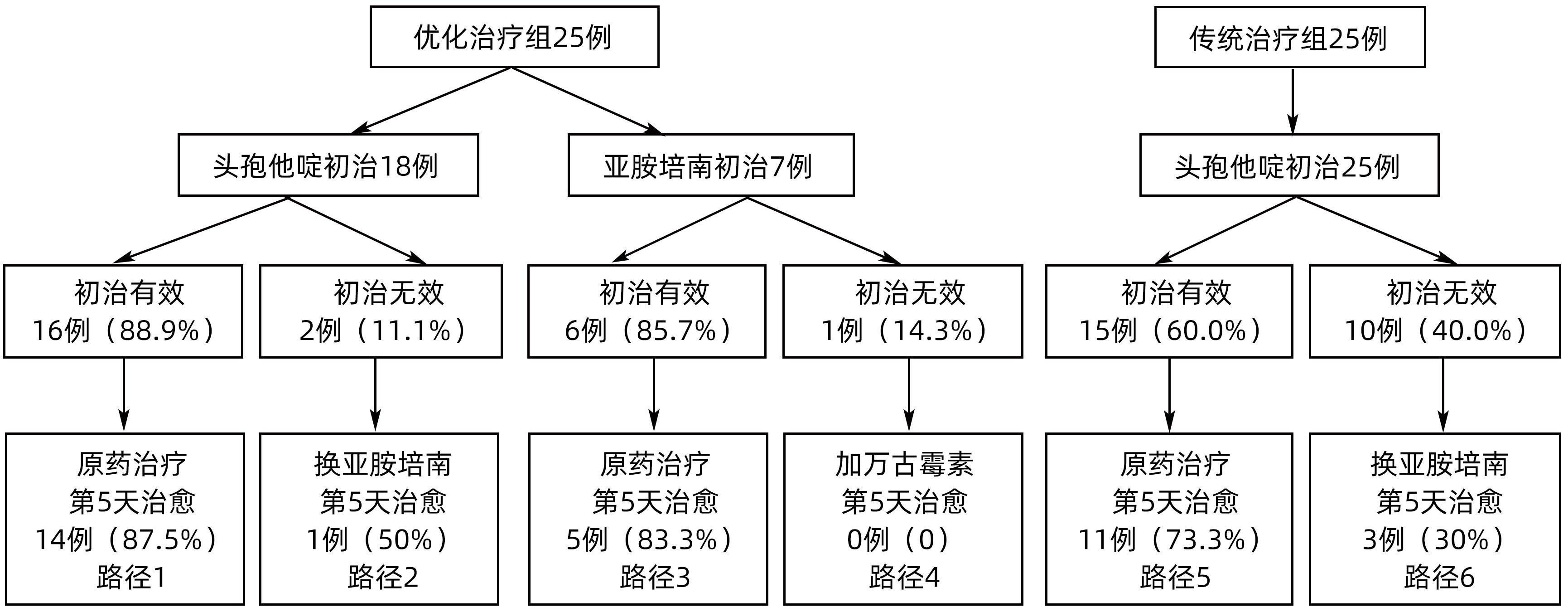
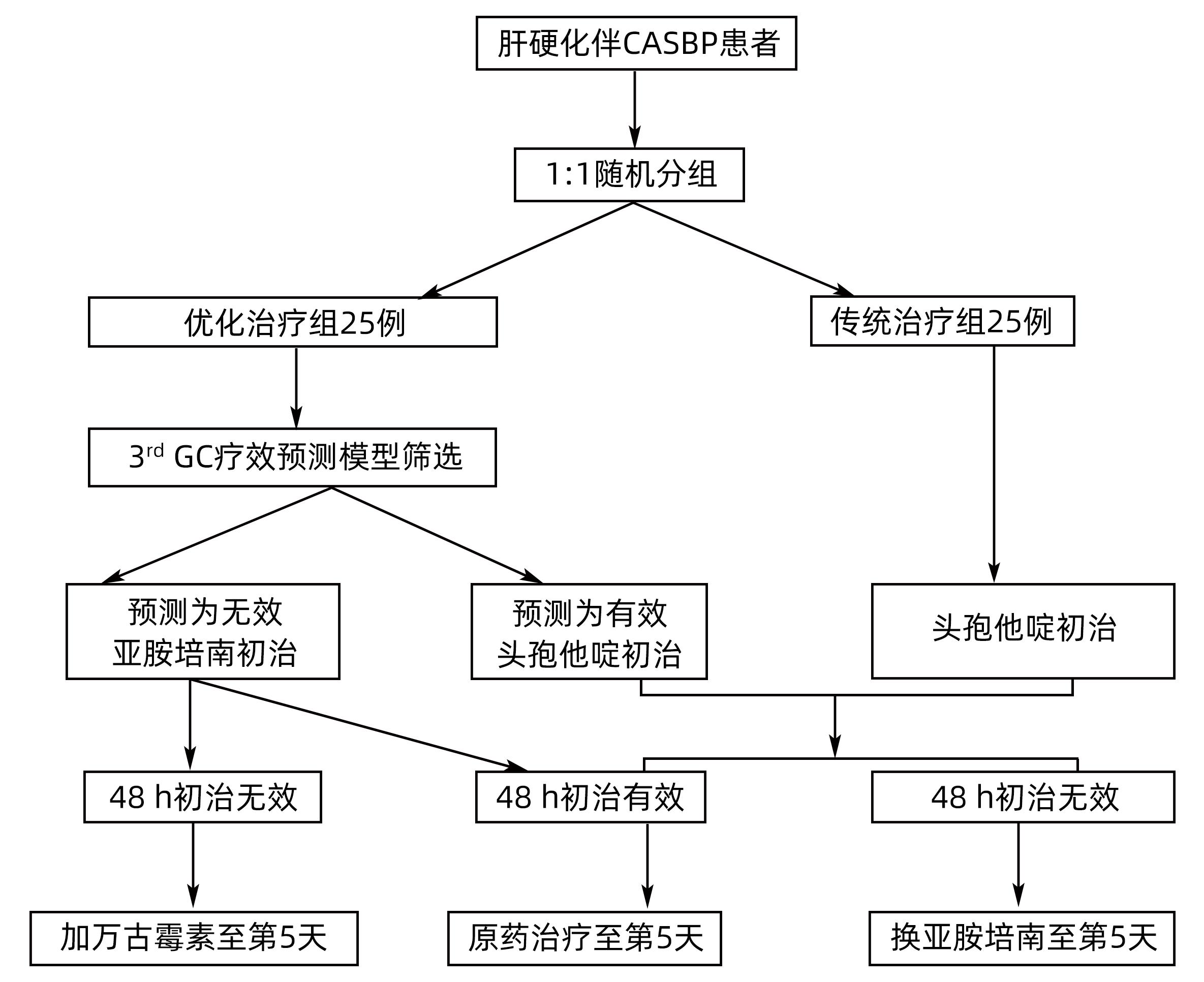
目的 探讨第三代头孢菌素(3rd GC)治疗社区获得性自发性细菌性腹膜炎(CASBP)效果预测模型的临床应用价值。 方法 前瞻性选取2021年1月—2022年6月南昌市第九医院新入院的肝硬化伴CASBP患者50例,随机分为优化治疗组(n=25)与传统治疗组(n=25),前者基于效果预测模型采用头孢他啶或亚胺培南初治,后者均采用头孢他啶初治,此后依据初治效果调整抗生素,比较两组的初治有效率、第5天治愈率及30天病死率。计量资料两组间比较采用成组t检验或Mann-Whitney U检验。计数资料两组间比较采用χ2检验或Fisher精确概率法。 结果 所有患者均完成研究。优化治疗组初治有效率明显高于传统治疗组(88.0% vs 60.0%,χ2=5.094,P=0.024),两组第5天治愈率相当(80.0% vs 56.6%,χ2=3.309,P=0.069)。均使用头孢他定初治的患者中,优化治疗组初治有效率亦明显高于传统治疗组(88.9% vs 60.0%,χ2=4.341,P=0.037),两组第5天治愈率相当(83.3% vs 56.0%,χ2=2.425,P=0.119)。两组患者的30天病死率分别为8.0%和20.0%,差异无统计学意义(χ2=0.664,P=0.415)。所有入组患者初治有效与第5天治愈关联明显(OR=9.643,95%CI:2.292~40.564),第5天治愈与患者30天死亡关联明显(OR=0.138,95%CI:0.023~0.813)。 结论 该疗效预测模型有助于临床医生筛选3rd GC治疗的优势患者,提高3rd GC经验性治疗CASBP的初治疗效。 Abstract:Objective To investigate the clinical application value of a predictive model for the efficacy of third-generation cephalosporin in the treatment of community-acquired spontaneous bacterial peritonitis (CASBP). Methods This prospective study was conducted among 50 patients with liver cirrhosis and CASBP who were admitted to The Ninth Hospital of Nanchang from January 2021 to June 2022, and the patients were randomly divided into optimized treatment group and traditional treatment group, with 25 patients in each group. The patients in the optimized treatment group received ceftazidime or imipenem for initial treatment based on the above predictive model, and those in the traditional treatment group received ceftazidime for initial treatment, with the subsequent use of antibiotics adjusted based on the efficacy of initial treatment. The two groups were compared in terms of the response rate of initial treatment, cure rate on day 5, and 30-day mortality rate. The independent-samples t test or the Mann-Whitney U test was used for comparison of continuous data between two groups, and the chi-square test or the Fisher’s exact test was used for comparison of categorical data between two groups. Results All patients completed the study. The optimized treatment group had a significantly higher response rate of initial treatment than the traditional treatment group (88.0% vs 60.0%, χ2=5.094, P=0.024), while there was no significant difference in the cure rate on day 5 between the two groups (80.0% vs 56.6%, χ2=3.309, P=0.069). As for the patients who received ceftazidime for initial treatment, the optimized treatment group had a significantly higher response rate of initial treatment than the traditional treatment group (88.9% vs 60.0%, χ2=4.341, P=0.037), while there was no significant difference in the cure rate on day 5 between the two groups (83.3% vs 56.0%, χ2=2.425, P=0.119). There was no significant difference in 30-day mortality rate between the two groups (8.0% vs 20.0%, χ2=0.664, P=0.415). For all patients, there was a significant association between response of initial treatment and cure on day 5 (odds ratio [OR]=9.643, 95% confidence interval [CI]: 2.292 — 40.564) and between cure on day 5 and 30-day mortality (OR=0.138, 95%CI: 0.023 — 0.813). Conclusion This predictive model for efficacy helps clinicians to identify the patients who can benefit from third-generation cephalosporin treatment and improve the efficacy of third-generation cephalosporin in the initial empirical treatment of CASBP. -
Key words:
- Liver Cirrhosis /
- Peritonitis /
- Community-Acquired Infections /
- Cephalosporins /
- Treatment Outcome
-
表 1 两组患者基线情况比较
Table 1. Comparison of baseline between two groups of patients
指标 传统治疗组(n=25) 优化治疗组(n=25) 统计值 P值 男性[例(%)] 17(68.0) 22(88.0) χ2=2.914 0.088 年龄(岁) 50.2±9.8 55.3±11.9 t=-1.625 0.111 肝硬化病因[例(%)] 0.220 HBV 17(68.0) 15(60.0) 酒精 4(16.0) 4(16.0) HCV 1(4.0) 0(0.0) HBV+酒精 3(12.0) 1(4.0) HBV+HCV 0(0.0) 1(4.0) 隐源性 0(0.0) 4(16.0) 2型糖尿病[例(%)] 4(16.0) 1(4.0) χ2=0.889 0.346 脾切除术[例(%)] 1(4.0) 4(16.0) χ2=0.889 0.346 广谱抗生素暴露[例(%)] 9(36.0) 8(32.0) χ2=0.089 0.765 SBP首次发病[例(%)] 18(72.0) 20(80.0) χ2=0.439 0.508 腹痛[例(%)] 7(28.0) 9(36.0) χ2=0.368 0.544 腹部压痛[例(%)] 16(64.0) 14(56.0) χ2=0.333 0.564 腹部反跳痛[例(%)] 15(60.0) 14(56.0) χ2=0.082 0.774 腹水量[例(%)] χ2=0.082 0.470 少量 0(0.0) 2(8.0) 中大量 25(100.0) 23(92.0) 体温(℃) 36.6(36.4~37.9) 36.6(36.4~38.0) Z=-0.234 0.815 白细胞(×109/L) 4.7(3.7~7.6) 4.9(3.2~9.3) Z=-0.116 0.907 血小板(×1012/L) 72.0(41.5~94.5) 80.0(47.0~108.5) Z=-0.951 0.342 凝血酶原时间(s) 15.5(13.4~20.3) 15.3(14.4~18.3) Z=-0.301 0.763 国际标准化比值 1.4(1.2~1.8) 1.3(1.2~1.5) Z=-1.068 0.286 谷丙转氨酶(U/L) 24.5(17.3~57.9) 26.0(14.7~35.3) Z=-0.990 0.322 谷草转氨酶(U/L) 34.8(28.8~89.0) 38.6(24.7~85.2) Z=-0.252 0.801 总胆红素(μmol/L) 37.8(17.7~69.3) 31.8(20.7~58.4) Z=-0.602 0.547 白蛋白(g/L) 29.5(23.7~33.7) 31.4(24.8~34.1) Z=-0.466 0.641 血肌酐(μmol/L) 71.2(66.1~106.2) 70.1(62.9~96.4) Z=-0.961 0.337 尿素氮(mmol/L) 5.2(4.5~7.1) 4.7(4.1~6.5) Z=-1.029 0.304 腹水白细胞(×109/L) 0.857(0.596~1.637) 1.034(0.713~2.345) Z=-1.145 0.252 腹水PMN(×109/L) 0.616(0.361~1.216) 0.700(0.518~1.417) Z=-1.009 0.313 MELD评分 9.3(6.7~18.6) 9.3(6.3~13.4) Z=-0.660 0.509 Child-Pugh评分 10(8~11) 9(8~11) Z=-1.243 0.214 -
[1] Chinese Society of Hepatology, Chinese Medical Association. Guidelines on the management of ascites and complications in cirrhosis[J]. J Clin Hepatol, 2017, 33( 10): 1847- 1863. DOI: 10.3969/j.issn.1001-5256.2017.10.003.中华医学会肝病学分会. 肝硬化腹水及相关并发症的诊疗指南[J]. 临床肝胆病杂志, 2017, 33( 10): 1847- 1863. DOI: 10.3969/j.issn.1001-5256.2017.10.003. [2] BIGGINS SW, ANGELI P, GARCIA-TSAO G, et al. Diagnosis, evaluation, and management of ascites, spontaneous bacterial peritonitis and hepatorenal syndrome: 2021 practice guidance by the American association for the study of liver diseases[J]. Hepatology, 2021, 74( 2): 1014- 1048. DOI: 10.1002/hep.31884. [3] ZHU LC, WU W, ZOU B, et al. Efficacy predictors of third-generation cephalosporins in treating spontaneous bacterial peritonitis[J]. Medicine(Baltimore), 2022, 101( 40): e30164. DOI: 10.1097/MD.0000000000030164. [4] ZHU LC, WU W, ZOU B, et al. Establishment of a model for predicting the efficacy of third-generation cephalosporin in treatment of community-acquired spontaneous bacterial peritonitis[J]. J Clin Hepatol, 2022, 38( 11): 2499- 2504. DOI: 10.3969/j.issn.1001-5256.2022.11.012.朱龙川, 吴蔚, 邹波, 等. 第三代头孢菌素治疗社区获得性自发性细菌性腹膜炎的疗效预测模型[J]. 临床肝胆病杂志, 2022, 38( 11): 2499- 2504. DOI: 10.3969/j.issn.1001-5256.2022.11.012. [5] AITHAL GP, PALANIYAPPAN N, CHINA L, et al. Guidelines on the management of ascites in cirrhosis[J]. Gut, 2021, 70( 1): 9- 29. DOI: 10.1136/gutjnl-2020-321790. [6] JINDAL A, KUMAR M, BHADORIA AS, et al. A randomized open label study of‘imipenem vs. cefepime’ in spontaneous bacterial peritonitis[J]. Liver Int, 2016, 36( 5): 677- 687. DOI: 10.1111/liv.12985. [7] PUGH RN, MURRAY-LYON IM, DAWSON JL, et al. Transection of the oesophagus for bleeding oesophageal varices[J]. Br J Surg, 1973, 60( 8): 646- 649. DOI: 10.1002/bjs.1800600817. [8] KAMATH PS, WIESNER RH, MALINCHOC M, et al. A model to predict survival in patients with end-stage liver disease[J]. Hepatology, 2001, 33( 2): 464- 470. DOI: 10.1053/jhep.2001.22172. [9] JIN PH. Medical statistical methods[M]. 2nd ed. Shanghai: Fudan University Press, 2003: 469- 471.金丕焕. 医用统计方法[M]. 第2版. 上海: 复旦大学出版社, 2003: 469- 471. [10] FIORE M, GENTILE I, MARAOLO AE, et al. Are third-generation cephalosporins still the empirical antibiotic treatment of community-acquired spontaneous bacterial peritonitis? A systematic review and meta-analysis[J]. Eur J Gastroenterol Hepatol, 2018, 30( 3): 329- 336. DOI: 10.1097/MEG.0000000000001057. [11] LIN QT, ZHU HD. Establishment of the model for predicting the initial therapeutic effect of hospital-acquired methicillin-resistant staphylococcus aureus pneumonia[J]. Chin J Crit Care Med, 2022, 42( 5): 393- 400. DOI: 10.3969/j.issn.1002-1949.2022.05.004.林清婷, 朱华栋. 建立医院获得性耐甲氧西林金黄色葡萄球菌肺炎的初始治疗效果预测模型的研究[J]. 中国急救医学, 2022, 42( 5): 393- 400. DOI: 10.3969/j.issn.1002-1949.2022.05.004. [12] LI C, SU HB, LIU XY, et al. Clinical outcome of patients with acute-on-chronic liver failure and bacterial infection after 72 hours of anti-infective therapy[J]. J Clin Hepatol, 2019, 35( 1): 147- 152. DOI: 10.3969/j.issn.1001-5256.2019.01.028.李晨, 苏海滨, 刘晓燕, 等. 慢加急性肝衰竭合并细菌感染患者抗感染治疗72小时的效果及影响因素[J]. 临床肝胆病杂志, 2019, 35( 1): 147- 152. DOI: 10.3969/j.issn.1001-5256.2019.01.028. [13] LEE CH, KANG HJ, YU SY, et al. Initial treatment response and short-term mortality of spontaneous bacterial peritonitis in cirrhotic patients with hepatocellular carcinoma[J]. Sci Rep, 2023, 13( 1): 6067. DOI: 10.1038/s41598-023-32006-8. [14] PIANO S, FASOLATO S, SALINAS F, et al. The empirical antibiotic treatment of nosocomial spontaneous bacterial peritonitis: Results of a randomized, controlled clinical trial[J]. Hepatology, 2016, 63( 4): 1299- 1309. DOI: 10.1002/hep.27941. [15] YIM HJ, KIM TH, SUH SJ, et al. Response-guided therapy with cefotaxime, ceftriaxone, or ciprofloxacin for spontaneous bacterial peritonitis: A randomized trial: A validation study of 2021 AASLD practice guidance for SBP[J]. Am J Gastroenterol, 2023, 118( 4): 654- 663. DOI: 10.14309/ajg.0000000000002126. [16] SAFFO S, TO UK, SANTOIEMMA PP, et al. Changes in ascitic fluid polymorphonuclear cell count after antibiotics are associated with mortality in spontaneous bacterial peritonitis[J]. Clin Gastroenterol Hepatol, 2022, 20( 5): e1201- e1204. DOI: 10.1016/j.cgh.2021.07.019. [17] SARWAR S, TARIQUE S, WARIS U, et al. Cephalosporin resistance in community acquired spontaneous bacterial peritonitis[J]. Pak J Med Sci, 2019, 35( 1): 4- 9. DOI: 10.12669/pjms.35.1.17. [18] SANGLODKAR U, JAIN M, VENKATARAMAN J. Predictors of immediate and short-term mortality in spontaneous bacterial peritonitis[J]. Indian J Gastroenterol, 2020, 39( 4): 331- 337. DOI: 10.1007/s12664-020-01040-z. -



 PDF下载 ( 922 KB)
PDF下载 ( 922 KB)

 下载:
下载: