熊去氧胆酸治疗1个月后的碱性磷酸酶水平和基线红细胞分布宽度对原发性胆汁性胆管炎治疗应答的预测价值
DOI: 10.12449/JCH240310
Value of alkaline phosphatase level after ursodeoxycholic acid treatment for one month and baseline red blood cell distribution width in predicting the treatment response of primary biliary cholangitis
-
摘要:
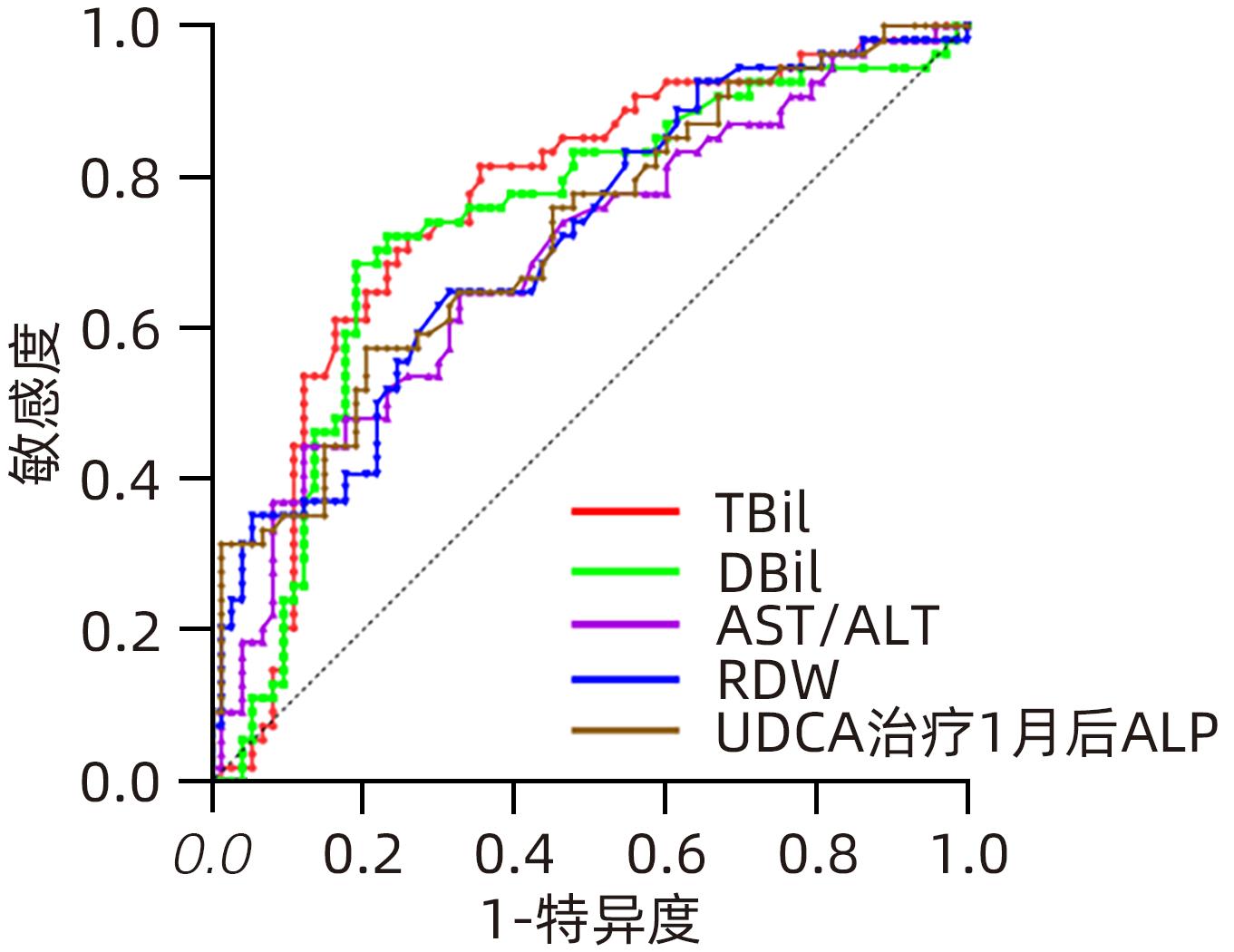
目的 研究基线红细胞分布宽度(RDW)和熊去氧胆酸(UDCA)治疗1个月后的ALP水平预测原发性胆汁性胆管炎(PBC)患者对UDCA治疗的应答情况。 方法 回顾性分析2015年1月—2022年7月于江苏大学附属第三人民医院肝病中心确诊的127例PBC患者资料,收集基线指标、治疗1个月后以及1年后随访数据。根据巴黎-Ⅰ标准将患者分为应答良好组和应答欠佳组,分析2组患者临床及实验室特征,以及与UDCA应答之间的相关性,利用Logistic回归法分析与UDCA治疗应答相关的独立危险因素。利用ROC曲线下面积(AUC)确定相关指标的最佳临界值,根据界值将患者再次分组,分析两组间基线指标、应答情况的差异。符合正态分布的计量资料两组间比较采用成组t检验;非正态分布的计量资料两组间比较采用Mann-Whitney U检验。计数资料组间比较则采用χ2检验。 结果 UDCA应答欠佳组患者基线TBil、AST/ALT、ALP、RDW、RDW-CV以及UDCA治疗1个月后的ALP水平明显高于应答良好组(Z值分别为-4.792、-3.697、-2.399、-4.102、-3.220、-4.236,P值均<0.05);应答欠佳组患者基线Alb、Hb、淋巴细胞数、红细胞比容及BMI水平明显低于应答良好组(Z值分别为-3.592、-3.603、-2.602、-3.829、-2.432,P值均<0.05);应答欠佳组患者基线前白蛋白、白球比、载脂蛋白A、游离三碘甲状腺原氨酸水平明显低于应答良好组(t值分别为4.530、3.402、3.485、3.639,P值均<0.001)。应答良好组患者存在肝硬化、合并胆囊结石胆囊炎以及贫血占比较低,两组间差异均有统计学意义(χ2值分别为20.815、3.892、12.283,P值均<0.05)。与UDCA应答相关的独立危险因素为基线RDW(OR=1.157,95%CI:1.028~1.301,P=0.015)及治疗1个月后的ALP水平(OR=1.012,95%CI:1.005~1.020,P=0.002),其AUC分别为0.713、0.720。基线RDW≥正常值上限且UDCA治疗1个月后ALP≥2.2倍正常值上限组患者UDCA应答率更低(42.6% vs 8.2%,χ2=20.813,P<0.001)。 结论 基线RDW≥正常值上限同时UDCA治疗1个月后ALP≥2.2倍正常值上限的患者对UDCA的生化应答率更低。 Abstract:Objective To investigate the value of baseline red cell distribution width (RDW) and alkaline phosphatase (ALP) level after ursodeoxycholic acid (UDCA) treatment for one month in predicting the response to UDCA treatment in patients with primary biliary cholangitis (PBC). Methods A retrospective analysis was performed for the data of 127 patients with PBC who were diagnosed in Department of Hepatology, The Third People’s Hospital of Jiangsu University, from January 2015 to July 2022, with data collected at baseline, after one month of treatment, and after one year of follow-up. Based on the Paris-I criteria, the patients were divided into good response group and poor response group, and the two groups were analyzed in terms of clinical and laboratory features and their association with response to UDCA. The Logistic regression method was used to investigate the independent risk factors for response to UDCA treatment. The area under the ROC curve (AUC) was used to determine the optimal cut-off values of related indicators; the patients were divided into two groups based on such values, and the two groups were compared in terms of baseline indicators and response. The independent-samples t test was used for comparison of normally distributed continuous data between two groups, and the Mann-Whitney U test was used for comparison of non-normally distributed continuous data between two groups; the chi-square test was used for comparison of categorical data between two groups. Results Compared with the good response group, the poor response group had significantly higher levels of total bilirubin, aspartate aminotransferase/alanine aminotransferase, ALP, RDW, and RDW-CV at baseline and a significantly higher level of ALP after one month of UDCA treatment (Z=-4.792, -3.697, -2.399, -4.102, -3.220, and -4.236, all P<0.05). Compared with the good response group, the poor response group had significantly lower levels of albumin, hemoglobin, lymphocytes, hematocrit, and body mass index at baseline (Z=-3.592, -3.603, -2.602, -3.829, -2.432, all P<0.05), as well as significantly lower levels of prealbumin, albumin/globulin ratio, apolipoprotein A, and free triiodothyronine at baseline (t=4.530, 3.402, 3.485, and 3.639, all P<0.001). Compared with the poor response group, the good response group had a significantly lower proportion of patients with liver cirrhosis, gallstones/cholecystitis, or anemia (χ2=20.815, 3.892, and 12.283, all P<0.05). Baseline RDW (odds ratio [OR]=1.157, 95% confidence interval [CI]: 1.028 — 1.301, P=0.015) and ALP level after one month of treatment (OR=1.012, 95%CI: 1.005 — 1.020, P=0.002) were independent risk factors for response to UDCA, with an AUC of 0.713 and 0.720, respectively. The patients with baseline RDW≥upper limit of normal (ULN) and ALP≥2.2×ULN after one month of UDCA treatment had a lower UDCA response rate (42.6% vs 8.2%, χ2=20.813, P<0.001). Conclusion Patients with baseline RDW≥ULN and ALP≥2.2×ULN after one month of UDCA treatment tend to have a low biochemical response rate to UDCA. -
Key words:
- Primary Biliary Cholangitis /
- Ursodeoxycholic Acid /
- Risk Factors /
- Biochemical Response
-
表 1 PBC患者基线特征
Table 1. Baseline characteristics of PBC patients
指标 数值 性别 [例(%)] 男 17(13.4) 女 110(86.6) 年龄(岁) 57±9 BMI(kg/m2) 22.3(20.7~24.2) TBil(μmol/L) 20.2(13.7~38.5) DBil(μmol/L) 9.4(5.5~23.7) Alb(g/L) 39.8(34.5~43.8) A/G 1.10±0.34 PA(mg/L) 161.7±68.9 ALT(U/L) 86(50~121) AST(U/L) 91(55~134) AST/ALT 1.01(0.76~1.37) ALP(U/L) 304(165~487) GGT(U/L) 301(144~534) a-HBDH(U/L) 147±33 TC(mmol/L) 4.82(3.73~5.97) TG(mmol/L) 1.26(0.88~1.80) HDL(mmol/L) 1.57±0.72 APOA(g/L) 1.38±0.48 Hb(g/L) 121(106~130) Neu(×109/L) 2.57(2.02~3.45) Lym(×109/L) 1.29(0.95~1.64) PCV(%) 0.36(0.32~0.39) RDW(fL) 46.4(43.7~49.6) RDW-CV(%) 14.0(12.9~15.5) MPV(fL) 11.75±1.54 P-LCR(%) 38.9±11.4 ANA 127(56~302) T3(nmol/L) 4.22±0.83 注:A/G,白球比;PA,前白蛋白;a-HBDH,a-羟丁酸脱氢酶;APOA,载脂蛋白A;Neu,中性细胞数;Lym,淋巴细胞数;PCV,红细胞比容;RDW-CV,红细胞分布宽度变异系数;MPV,平均血小板体积;P-LCR,大型血小板比率;ANA,抗核抗体;T3,游离三碘甲状腺原氨酸。 表 2 UDCA应答良好组与UDCA应答欠佳组的临床特征比较
Table 2. Comparative analysis of the clinical characteristics of the good UDCA response group and the poor UDCA response group
组别 例数 脂肪肝[例(%)] 肝硬化[例(%)] 胆囊结石胆囊炎[例(%)] 贫血[例(%)] SS-A/Ro52KD阳性[例(%)] CENP-B着丝点抗体阳性[例(%)] 应答良好组 73 9(12.3) 27(37.0) 10(13.7) 16(21.9) 14(19.2) 16(21.9) 应答欠佳组 54 6(11.1) 42(77.8) 15(27.8) 28(51.9) 14(25.9) 13(24.1) χ2值 0.044 20.815 3.892 12.283 0.822 0.082 P值 0.834 P<0.001 P<0.05 P<0.001 0.364 0.775 表 3 UDCA应答良好组与UDCA应答欠佳组的实验室指标比较
Table 3. Comparative analysis of the laboratory test indices of the good UDCA response group and the poor UDCA response group
指标 UDCA应答良好组(n=73) UDCA应答欠佳组(n=54) 统计值 P值 年龄(岁) 56±9 57±9 t=-0.281 0.780 BMI(kg/m2) 22.6(21.4~24.8) 21.9(20.1~23.3) Z=-2.432 0.015 TBil(μmol/L) 15.4(11.6~22.9) 32.6(19.8~54.4) Z=-4.972 <0.001 DBil(μmol/L) 6.8(4.6~10.4) 15.9(8.7~31.5) Z=-4.480 <0.001 Alb(g/L) 41.2(37.7~44.3) 37.4(29.0~41.3) Z=-3.592 <0.001 A/G 1.19±0.31 0.99±0.35 t=3.402 <0.001 PA(mg/L) 183.9±61.6 131.8±67.3 t=4.530 <0.001 ALT(U/L) 88(54~144) 76(42~114) Z=-1.600 0.110 AST(U/L) 81(52~141) 103(70~125) Z=-0.744 0.457 AST/ALT 0.92(0.71~1.23) 1.26(0.92~1.63) Z=-3.697 <0.001 ALP(U/L) 265(162~452) 377(197~717) Z=-2.399 0.016 GGT(U/L) 286(145~472) 410(130~566) Z=-0.744 0.457 a-HBDH(U/L) 143±28 152±38 t=-1.435 0.154 TC(mmol/L) 4.79(3.90~5.88) 5.07(3.56~6.61) Z=-0.268 0.789 TG(mmol/L) 1.19(0.89~1.81) 1.29(0.88~1.68) Z=-0.263 0.792 HDL(mmol/L) 1.68±0.69 1.44±0.75 t=1.860 0.065 APOA(g/L) 1.50±0.43 1.21±0.49 t=3.485 <0.001 Hb(g/L) 123(114~133) 110(94~128) Z=-3.603 <0.001 Neu(109/L) 2.48(1.91~3.30) 2.70(2.09~3.80) Z=-1.680 0.093 Lym(109/L) 1.36(1.02~1.87) 1.13(0.90~1.51) Z=-2.602 0.009 PCV(%) 0.37(0.35~0.40) 0.33(0.30~0.37) Z=-3.829 <0.001 RDW(fL) 45.0(43.0~47.9) 48.2(44.9~53.7) Z=-4.102 <0.001 RDW-CV(%) 13.6(12.7~14.8) 14.7(13.4~16.4) Z=-3.220 <0.001 MPV(fL) 11.56±1.45 12.01±1.63 t=-1.333 0.185 P-LCR(%) 37.4±11.1 40.9±11.7 t=-1.702 0.091 ANA 129(53~310) 112(58~270) Z=-0.159 0.874 T3(nmol/L) 4.44±0.83 3.92±0.75 t=3.639 <0.001 1月后ALP(U/L) 150(107~220) 253(164~423) Z=-4.236 <0.001 表 4 PBC患者UDCA应答欠佳的影响因素分析
Table 4. Analysis of factors associated with poor UDCA response in patients with PBC
指标 OR 95%CI P值 BMI(kg/m2) 0.841 0.676~1.046 0.119 TBil(μmol/L) 1.020 0.982~1.058 0.310 DBil(μmol/L) 0.959 0.913~1.006 0.086 Alb(g/L) 1.004 0.860~1.172 0.964 A/G 2.046 0.207~20.243 0.540 PA(mg/L) 0.992 0.980~1.004 0.207 AST/ALT 2.107 0.922~4.811 0.077 ALP(U/L) 0.998 0.994~1.002 0.279 APOA(g/L) 0.402 0.062~2.617 0.340 Hb(g/L) 1.046 0.963~1.135 0.287 Lym(109/L) 1.120 0.497~2.523 0.785 RDW(fL) 1.157 1.028~1.301 0.015 RDW-CV(%) 1.106 0.962~1.272 0.158 T3(nmol/L) 0.835 0.374~1.861 0.659 1个月后ALP(U/L) 1.012 1.005~1.020 0.002 表 5 相关指标预测UDCA治疗1年后应答欠佳的AUC值
Table 5. PBC patient-related indicators predict AUC for poor response after 1 year of UDCA therapy
指标 AUC 95%CI P值 TBil 0.759 0.672~0.854 <0.001 DBil 0.733 0.641~0.825 <0.001 AST/ALT 0.692 0.599~0.786 <0.001 基线ALP 0.625 0.525~0.725 0.016 RDW 0.713 0.623~0.803 <0.001 RDW-CV 0.667 0.572~0.763 0.001 UDCA治疗1个月后ALP 0.720 0.631~0.810 <0.001 -
[1] GULAMHUSEIN AF, HIRSCHFIELD GM. Primary biliary cholangitis: pathogenesis and therapeutic opportunities[J]. Nat Rev Gastroenterol Hepatol, 2020, 17( 2): 93- 110. DOI: 10.1038/s41575-019-0226-7. [2] FLOREANI A, GABBIA D, de MARTIN S. Obeticholic acid for primary biliary cholangitis[J]. Biomedicines, 2022, 10( 10). DOI: 10.3390/biomedicines10102464. [3] YOU H, MA X, EFE C, et al. APASL clinical practice guidance: the diagnosis and management of patients with primary biliary cholangitis[J]. Hepatol Int, 2022, 16( 1): 1- 23. DOI: 10.1007/s12072-021-10276-6. [4] HARMS MH, LAMMERS WJ, THORBURN D, et al. Major hepatic complications in ursodeoxycholic acid-treated patients with primary biliary cholangitis: Risk factors and time trends in incidence and outcome[J]. Am J Gastroenterol, 2018, 113( 2): 254- 264. DOI: 10.1038/ajg.2017.440. [5] European Association for the Study of the Liver. EASL Clinical Practice Guidelines: The diagnosis and management of patients with primary biliary cholangitis[J]. J Hepatol, 2017, 67( 1): 145- 172. DOI: 10.1016/j.jhep.2017.03.022. [6] NEVENS F, ANDREONE P, MAZZELLA G, et al. A placebo-controlled trial of obeticholic acid in primary biliary cholangitis[J]. N Engl J Med, 2016, 375( 7): 631- 643. DOI: 10.1056/NEJMoa1509840. [7] TANAKA A. Current understanding of primary biliary cholangitis[J]. Clin Mol Hepatol, 2021, 27( 1): 1- 21. DOI: 10.3350/cmh.2020.0028. [8] BRUNET E, HERNÁNDEZ L, MIQUEL M, et al. Analysis of predictive response scores to treatment with ursodeoxycholic acid in patients with primary biliary cholangitis[J]. Med Clin(Barc), 2019, 152( 10): 377- 383. DOI: 10.1016/j.medcli.2018.08.002. [9] TERZIROLI BERETTA-PICCOLI B, MIELI-VERGANI G, VERGANI D, et al. The challenges of primary biliary cholangitis: What is new and what needs to be done[J]. J Autoimmun, 2019, 105: 102328. DOI: 10.1016/j.jaut.2019.102328. [10] ALOMARI M, COVUT F, MOMANI L AL, et al. Evaluation of the United Kingdom-primary biliary cholangitis and global primary biliary cholangitis group prognostic models for primary biliary cholangitis patients treated with ursodeoxycholic acid in the U.S. population[J]. JGH Open, 2020, 4( 2): 132- 139. DOI: 10.1002/jgh3.12223. [11] SCHATTENBERG JM, PARES A, KOWDLEY KV, et al. A randomized placebo-controlled trial of elafibranor in patients with primary biliary cholangitis and incomplete response to UDCA[J]. J Hepatol, 2021, 74( 6): 1344- 1354. DOI: 10.1016/j.jhep.2021.01.013. [12] ASLAM H, OZA F, AHMED K, et al. The role of red cell distribution width as a prognostic marker in chronic liver disease: A literature review[J]. Int J Mol Sci, 2023, 24( 4): 3487. DOI: 10.3390/ijms24043487. [13] LOU Y, WANG M, MAO W. Clinical usefulness of measuring red blood cell distribution width in patients with hepatitis B[J]. PLoS One, 2012, 7( 5): e37644. DOI: 10.1371/journal.pone.0037644. [14] YANG CY, MA X, TSUNEYAMA K, et al. IL-12/Th1 and IL-23/Th17 biliary microenvironment in primary biliary cirrhosis: implications for therapy[J]. Hepatology, 2014, 59( 5): 1944- 1953. DOI: 10.1002/hep.26979. [15] WANG H, XU H, WANG X, et al. Red blood cell distribution width to platelet ratio is related to histologic severity of primary biliary cirrhosis[J]. Medicine(Baltimore), 2016, 95( 11): e3114. DOI: 10.1097/MD.0000000000003114. [16] OWOICHO O, TAPELA K, OLWAL CO, et al. Red blood cell distribution width as a prognostic biomarker for viral infections: prospects and challenges[J]. Biomark Med, 2022, 16( 1): 41- 50. DOI: 10.2217/bmm-2021-0364. [17] CORTEZ-PINTO H, LIBERAL R, LOPES S, et al. Predictors for incomplete response to ursodeoxycholic acid in primary biliary cholangitis. Data from a national registry of liver disease[J]. United European Gastroenterol J, 2021, 9( 6): 699- 706. DOI: 10.1002/ueg2.12095. [18] ANGULO P, LINDOR KD, THERNEAU TM, et al. Utilization of the Mayo risk score in patients with primary biliary cirrhosis receiving ursodeoxycholic acid[J]. Liver, 1999, 19( 2): 115- 121. DOI: 10.1111/j.1478-3231.1999.tb00020.x. [19] PARÉS A, CABALLERÍA L, RODÉS J. Excellent long-term survival in patients with primary biliary cirrhosis and biochemical response to ursodeoxycholic acid[J]. Gastroenterology, 2006, 130( 3): 715- 720. DOI: 10.1053/j.gastro.2005.12.029. [20] JORGENSEN RA, DICKSON ER, HOFMANN AF, et al. Characterisation of patients with a complete biochemical response to ursodeoxycholic acid[J]. Gut, 1995, 36( 6): 935- 938. DOI: 10.1136/gut.36.6.935. [21] CARBONE M, NARDI A, FLACK S, et al. Pretreatment prediction of response to ursodeoxycholic acid in primary biliary cholangitis: development and validation of the UDCA Response Score[J]. Lancet Gastroenterol Hepatol, 2018, 3( 9): 626- 634. DOI: 10.1016/S2468-1253(18)30163-8. [22] ZHANG LN, SHI TY, SHI XH, et al. Early biochemical response to ursodeoxycholic acid and long-term prognosis of primary biliary cirrhosis: results of a 14-year cohort study[J]. Hepatology, 2013, 58( 1): 264- 272. DOI: 10.1002/hep.26322. [23] MURILLO PEREZ CF, IOANNOU S, HASSANALLY I, et al. Optimizing therapy in primary biliary cholangitis: Alkaline phosphatase at six months identifies one-year non-responders and predicts survival[J]. Liver Int, 2023, 43( 7): 1497- 1506. DOI: 10.1111/liv.15592. [24] YANG C, GUO G, LI B, et al. Prediction and evaluation of high-risk patients with primary biliary cholangitis receiving ursodeoxycholic acid therapy: an early criterion[J]. Hepatol Int, 2023, 17( 1): 237- 248. DOI: 10.1007/s12072-022-10431-7. [25] HUANG LX, WANG ZL, JIN R, et al. Incomplete response to ursodeoxycholic acid in primary biliary cholangitis: criteria, epidemiology, and possible mechanisms[J]. Expert Rev Gastroenterol Hepatol, 2022, 16( 11-12): 1065- 1078. DOI: 10.1080/17474124.2022.2153672. -



 PDF下载 ( 675 KB)
PDF下载 ( 675 KB)

 下载:
下载:


