肝豆状核变性发病机制、临床表型-基因型关系及药物治疗研究进展
DOI: 10.3969/j.issn.1001-5256.2023.06.037
Research advances in the pathogenesis, phenotype-genotype relationship, and pharmacotherapy of hepatolenticular degeneration
-
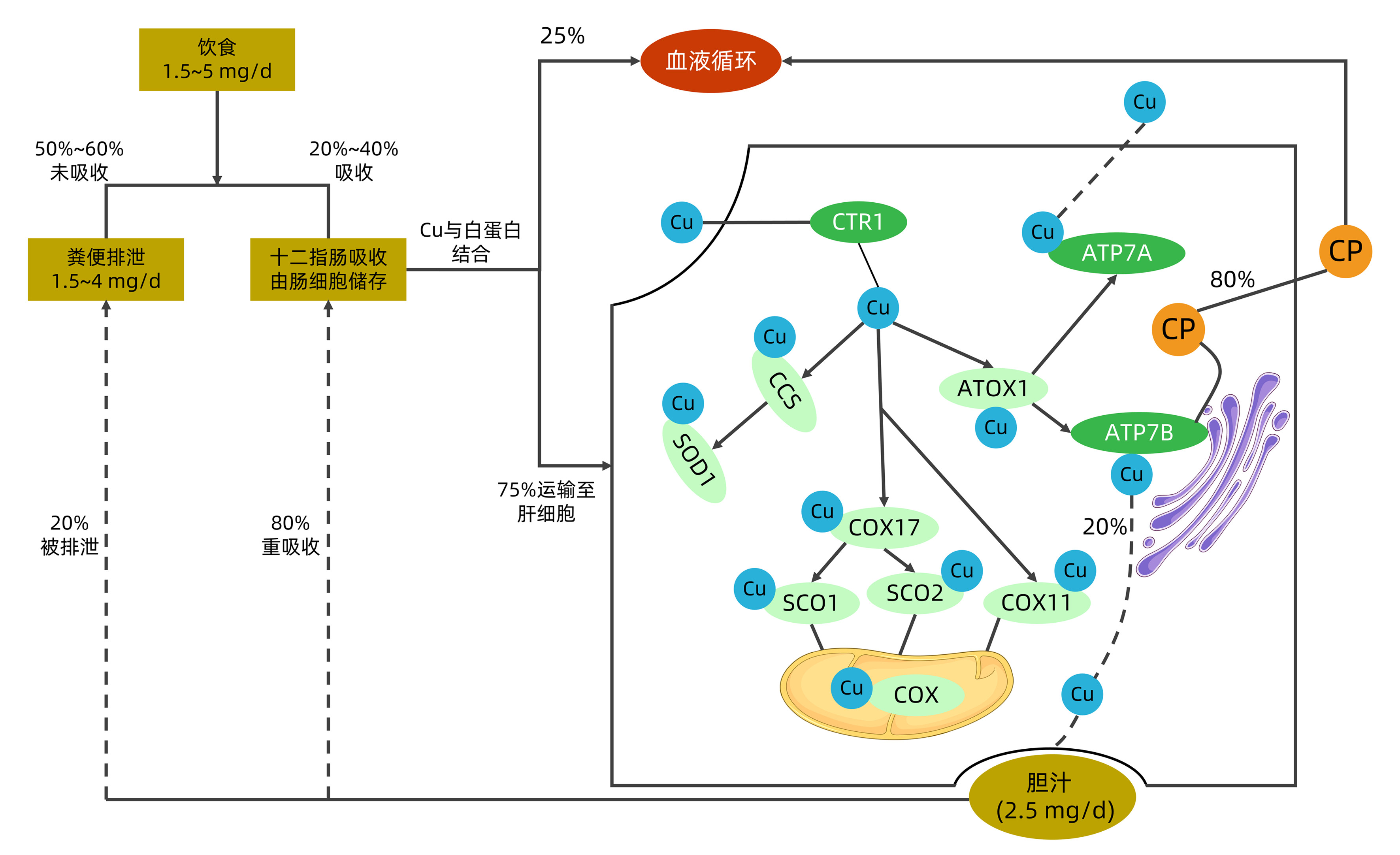
摘要: 肝豆状核变性又称Wilson病(WD),WD中铜与铜蓝蛋白结合受损,导致游离铜主要在肝脏、大脑和其他器官中沉积。WD的患病率为1/30 000。在临床上,大多数WD患者都是年轻人,其特征是锥体外系症状、肝硬化、角膜K-F环、血清低铜蓝蛋白水平(<50 mg/L)和24 h高尿铜排泄(>100 mg/L)。目前WD主要的治疗措施为药物治疗。在一些终末期肝病或急性肝衰竭的病例中,肝移植是提高生存率的一种选择。本综述结合国内外对WD发病机制、临床表型与基因型的关系及药物治疗进展的研究作出了概述。Abstract: In hepatolenticular degeneration, also known as Wilson's disease (WD), the binding of copper to ceruloplasmin is impaired, resulting in the deposition of free copper mainly in the liver, brain, and other organs. The prevalence rate of WD was 1/30 000. In clinical practice, most WD patients are young adults and are characterized by extrapyramidal symptoms, liver cirrhosis, Kayser-Fleischer ring of the cornea, low serum ceruloplasmin level (< 50 mg/L), and high 24-hour urinary copper excretion (> 100 mg/L). At present, pharmacotherapy is the main treatment method for WD, and in some cases of end-stage liver disease or acute liver failure, liver transplantation is an option to improve survival rate. This article reviews the research advances in the pathogenesis of hepatolenticular degeneration, phenotype-genotype relationship, and pharmacotherapy in China and globally.
-
Key words:
- Hepatolenticular Degeneration /
- Genotype /
- Drug Therapy
-
表 1 ATP7B基因突变类型与临床表型关系
Table 1. Relationship between ATP7B gene mutation type and clinical phenotype
作者(年份) 样本量(例) 主要突变类型 研究结局 Das等(2022)[16] ≥80 纯合p.His1069Gln
p.Arg778Leup.Arg778Leu患者发病年龄早,CP水平低,大多表现为肝脏症状;p.His1069Gln患者主要表现为迟发性神经系统症状 张天鹤等(2022)[17] 70 p.Arg778Leu p.Arg778Leu突变患者表现出较低的CP水平及肝脏症状 周霄颖等(2020)[18] 55 p.Arg778Leu p.Arg778Leu突变发病年龄早,肝脏损害较重 Zhang等(2022)[20] 1 366 p.Arg778Leu、p.Pro992Leu、p.Ala874Val p.Arg778Leu、p.Pro992Leu发病年龄早,p.Ala874Val发病年龄较晚并与构音障碍有关 Nagral等(2022)[21] 58 p.Cys271Ter 未发现基因变异与临床表现关联 刘攀等(2022)[22] 75 p.Arg778Leu、p.Ala874Val、p.Pro992Leu 基因型-表型无明显相关性 表 2 WD与其他Cu代谢指标异常遗传性疾病的鉴别
Table 2. Differential diagnosis of WD and other genetic diseases with abnormal copper metabolism indexes
疾病类型 病因 实验室特征 临床特征 Menkes综合征[23] ATP7A基因突变 血清Cu、CP及肝Cu减少 严重的神经退行性病变、毛发异常、癫痫发作、体温过低、结缔组织紊乱 MEDNIK综合征[24] AP1S1基因突变 血清Cu减少,血清CP减少和肝Cu升高 智力迟钝,肠病,耳聋,神经病变,皮肤表现(鱼鳞病和角化皮病) 遗传性铜蓝蛋白缺乏症 CP基因突变 血清CP无法检测或明显降低,血清Cu、尿Cu及肝Cu水平正常 神经系统疾病、糖尿病和贫血,这些都与全身铁的过度积累有关 Huppke-Brendel综合征[6] 编码乙酰辅酶A转运体1的SLC33A1基因突变 血清Cu和CP水平低 先天性白内障、听力丧失和严重发育迟缓,也可见明显的小脑发育不全和骨髓鞘减少 WD ATP7B基因突变 血清Cu和CP降低,尿Cu排泄增加,肝Cu水平增加 肝脏疾病、神经系统疾病和精神表现、角膜K-F环 -
[1] CHENG YL. Hepato-lenticular degeneration: (Pseudosclerosis, progressive lenticular degeneration and torsionspasm): Review of literature and repoet of two cases[J]. Chin Med J, 1932, 46(4): 347-369. [2] CHANG IJ, HAHN SH. The genetics of Wilson disease[J]. Handb Clin Neurol, 2017, 142: 19-34. DOI: 10.1016/B978-0-444-63625-6.00003-3. [3] JI L, ZHANG Y, KONG L, et al. Clinical features of Wilson's disease: An analysis of 83 cases[J]. J Clin Hepatol, 2022, 38(8): 1843-1846. DOI: 10.3969/j.issn.1001-5256.2022.08.023.纪雷, 张莹, 孔丽, 等. 83例肝豆状核变性患者的临床特征分析[J]. 临床肝胆病杂志, 2022, 38(8): 1843-1846. DOI: 10.3969/j.issn.1001-5256.2022.08.023. [4] XIE JJ, WU ZY. Wilson's disease in China[J]. Neurosci Bull, 2017, 33(3): 323-330. DOI: 10.1007/s12264-017-0107-4. [5] WEITZMAN E, PAPPO O, WEISS P, et al. Late onset fulminant Wilson's disease: a case report and review of the literature[J]. World J Gastroenterol, 2014, 20(46): 17656-17660. DOI: 10.3748/wjg.v20.i46.17656. [6] CZŁONKOWSKA A, LITWIN T, DUSEK P, et al. Wilson disease[J]. Nat Rev Dis Primers, 2018, 4(1): 21. DOI: 10.1038/s41572-018-0018-3. [7] BULL PC, THOMAS GR, ROMMENS JM, et al. The Wilson disease gene is a putative copper transporting P-type ATPase similar to the Menkes gene[J]. Nat Genet, 1993, 5(4): 327-337. DOI: 10.1038/ng1293-327. [8] BREWER GJ, ASKARI F, DICK RB, et al. Treatment of Wilson's disease with tetrathiomolybdate: V. Control of free copper by tetrathiomolybdate and a comparison with trientine[J]. Transl Res, 2009, 154(2): 70-77. DOI: 10.1016/j.trsl.2009.05.002. [9] ZISCHKA H, EINER C. Mitochondrial copper homeostasis and its derailment in Wilson disease[J]. Int J Biochem Cell Biol, 2018, 102: 71-75. DOI: 10.1016/j.biocel.2018.07.001. [10] LALIOTI V, MURUAIS G, TSUCHIYA Y, et al. Molecular mechanisms of copper homeostasis[J]. Front Biosci (Landmark Ed), 2009, 14(13): 4878-4903. DOI: 10.2741/3575. [11] BALDARI S, DI ROCCO G, TOIETTA G. Current biomedical use of copper chelation therapy[J]. Int J Mol Sci, 2020, 21(3): 1069. DOI: 10.3390/ijms21031069. [12] CHEN C, SHEN B, XIAO JJ, et al. Currently clinical views on genetics of Wilson's disease[J]. Chin Med J (Engl), 2015, 128(13): 1826-1830. DOI: 10.4103/0366-6999.159361. [13] LUTSENKO S, PETRUKHIN K, COOPER MJ, et al. N-terminal domains of human copper-transporting adenosine triphosphatases (the Wilson's and Menkes disease proteins) bind copper selectively in vivo and in vitro with stoichiometry of one copper per metal-binding repeat[J]. J Biol Chem, 1997, 272(30): 18939-18944. DOI: 10.1074/jbc.272.30.18939. [14] European Association for Study of Liver. EASL clinical practice guidelines: Wilson's disease[J]. J Hepatol, 2012, 56(3): 671-685. DOI: 10.1016/j.jhep.2011.11.007. [15] HUSTER D, KÜHNE A, BHATTACHARJEE A, et al. Diverse functional properties of Wilson disease ATP7B variants[J]. Gastroenterology, 2012, 142(4): 947-956. e5. DOI: 10.1053/j.gastro.2011.12.048. [16] DAS S, MOHAMMED A, MANDAL T, et al. Polarized trafficking and copper transport activity of ATP7B: A mutational approach to establish genotype-phenotype correlation in Wilson disease[J]. Hum Mutat, 2022, 43(10): 1408-1429. DOI: 10.1002/humu.24428. [17] ZHANG TH, MAO ZQ. Clinical characteristics and gene analysis of hepatolenticular degeneration in children: A report of 70 cases[J]. Chin J Pract Pediatr, 2022, 2(37): 135-139. DOI: 10.19538/j.ek2022020614.张天鹤, 毛志芹. 儿童肝豆状核变性的临床特点及基因分析(附70例报告)[J]. 中国实用儿科杂志, 2022, 2(37): 135-139. DOI: 10.19538/j.ek2022020614. [18] ZHOU XY, YIN HX, WANG CL, et al. Phenotype and genotype analysis of 55 children patients with Wilson's disease[J]. Chin J Hepatol, 2020, 28(7): 603-607. DOI: 10.3760/cma.j.cn501113-20190423-00143.周霄颖, 尹瀚浚, 王春莉, 等. 55例肝豆状核变性患儿表型与基因型分析[J]. 中华肝脏病杂志, 2020, 28(7): 603-607. DOI: 10.3760/cma.j.cn501113-20190423-00143. [19] USTA J, WEHBEH A, RIDA K, et al. Phenotype-genotype correlation in Wilson disease in a large Lebanese family: association of c. 2299insC with hepatic and of p. Ala1003Thr with neurologic phenotype[J]. PLoS One, 2014, 9(11): e109727. DOI: 10.1371/journal.pone.0109727. [20] ZHANG S, YANG W, LI X, et al. Clinical and genetic characterization of a large cohort of patients with Wilson's disease in China[J]. Transl Neurodegener, 2022, 11(1): 13. DOI: 10.1186/s40035-022-00287-0. [21] NAGRAL A, MALLAKMIR S, GARG N, et al. Genomic variations in ATP7B gene in indian patients with Wilson disease[J]. Indian J Pediatr, 2023, 90(3): 240-248. DOI: 10.1007/s12098-022-04250-9. [22] LIU P, CHE FY, SHU C, et al. Analysis of clinical phenotypes and ATP7B gene variants in 75 children patients with Wilson's disease[J]. Chin J Med Genetics, 2022, 39(4): 357-361. DOI: 10.3760/cma.j.cn511374-20201231-00926.刘攀, 车凤玉, 舒畅, 等. 75例肝型肝豆状核变性患儿的临床表型及ATP7B基因变异分析[J]. 中华医学遗传学杂志, 2022, 39(4): 357-361. DOI: 10.3760/cma.j.cn511374-20201231-00926. [23] TÜMER Z, MØLLER LB. Menkes disease[J]. Eur J Hum Genet, 2010, 18(5): 511-518. DOI: 10.1038/ejhg.2009.187. [24] ALSAIF HS, AL-OWAIN M, BARRIOS-LLERENA ME, et al. Homozygous loss-of-function mutations in AP1B1, encoding Beta-1 subunit of adaptor-related protein complex 1, cause MEDNIK-like syndrome[J]. Am J Hum Genet, 2019, 105(5): 1016-1022. DOI: 10.1016/j.ajhg.2019.09.020. [25] KASZTELAN-SZCZERBINSKA B, CICHOZ-LACH H. Wilson's disease: An update on the diagnostic workup and management[J]. J Clin Med, 2021, 10(21): 5097. DOI: 10.3390/jcm10215097. [26] LUCENA-VALERA A, PEREZ-PALACIOS D, MUÑOZ-HERNANDEZ R, et al. Wilson's disease: Revisiting an old friend[J]. World J Hepatol, 2021, 13(6): 634-649. DOI: 10.4254/wjh.v13.i6.634. [27] EMRE PARLAR Y, YASEMIN BALABAN H, YAVUZ MALKAN U, et al. A rare case of DIC in a patient with Wilson's disease: D-penicillamine[J]. Hepatol Forum, 2022, 3(2): 61-63. DOI: 10.14744/hf.2022.2022.0001. [28] BREWER GJ. Neurologically presenting Wilson's disease: epidemiology, pathophysiology and treatment[J]. CNS Drugs, 2005, 19(3): 185-192. DOI: 10.2165/00023210-200519030-00001. [29] SEETHARAMAN J, SARMA MS. Chelation therapy in liver diseases of childhood: Current status and response[J]. World J Hepatol, 2021, 13(11): 1552-1567. DOI: 10.4254/wjh.v13.i11.1552. [30] ALA A, ALIU E, SCHILSKY ML. Prospective pilot study of a single daily dosage of trientine for the treatment of Wilson disease[J]. Dig Dis Sci, 2015, 60(5): 1433-1439. DOI: 10.1007/s10620-014-3495-6. [31] WEISS KH, THURIK F, GOTTHARDT DN, et al. Efficacy and safety of oral chelators in treatment of patients with Wilson disease[J]. Clin Gastroenterol Hepatol, 2013, 11(8): 1028-1035. e1-2. DOI: 10.1016/j.cgh.2013.03.012. [32] WEISS KH, KRUSE C, MANOLAKI N, et al. Multicentre, retrospective study to assess long-term outcomes of chelator based treatment with trientine in Wilson disease patients withdrawn from therapy with D-penicillamine[J]. Eur J Gastroenterol Hepatol, 2022, 34(9): 940-947. DOI: 10.1097/MEG.0000000000002387. [33] SHRIBMAN S, MARJOT T, SHARIF A, et al. Investigation and management of Wilson's disease: a practical guide from the British Association for the Study of the Liver[J]. Lancet Gastroenterol Hepatol, 2022, 7(6): 560-575. DOI: 10.1016/S2468-1253(22)00004-8. [34] DONG Y, WU ZY. Challenges and suggestions for precise diagnosis and treatment of Wilson's disease[J]. World J Pediatr, 2021, 17(6): 561-565. DOI: 10.1007/s12519-021-00475-4. [35] AVAN A, CZŁONKOWSKA A, GASKIN S, et al. The role of zinc in the treatment of Wilson's disease[J]. Int J Mol Sci, 2022, 23(16): 9316. DOI: 10.3390/ijms23169316. [36] MUNK DE, LUND LAURSEN T, TEICHER KIRK F, et al. Effect of oral zinc regimens on human hepatic copper content: a randomized intervention study[J]. Sci Rep, 2022, 12(1): 14714. DOI: 10.1038/s41598-022-18872-8. [37] CHEN JC, CHUANG CH, WANG JD, et al. Combination therapy using chelating agent and zinc for Wilson's disease[J]. J Med Biol Eng, 2015, 35(6): 697-708. DOI: 10.1007/s40846-015-0087-7. [38] LI WJ, CHEN C, YOU ZF, et al. Current drug managements of Wilson's disease: From West to East[J]. Curr Neuropharmacol, 2016, 14(4): 322-325. DOI: 10.2174/1570159x14666151130222427. [39] WEISS KH, ASKARI FK, CZLONKOWSKA A, et al. Bis-choline tetrathiomolybdate in patients with Wilson's disease: an open-label, multicentre, phase 2 study[J]. Lancet Gastroenterol Hepatol, 2017, 2(12): 869-876. DOI: 10.1016/S2468-1253(17)30293-5. [40] LICHTMANNEGGER J, LEITZINGER C, WIMMER R, et al. Methanobactin reverses acute liver failure in a rat model of Wilson disease[J]. J Clin Invest, 2016, 126(7): 2721-2735. DOI: 10.1172/JCI85226. -



 PDF下载 ( 2259 KB)
PDF下载 ( 2259 KB)

 下载:
下载:


