血脂指标对乙型肝炎相关慢加急性肝衰竭前期进展的预测价值
DOI: 10.3969/j.issn.1001-5256.2023.07.009
Value of blood lipid parameters in predicting the progression of HBV-related acute-on-chronic pre-liver failure
-
摘要:
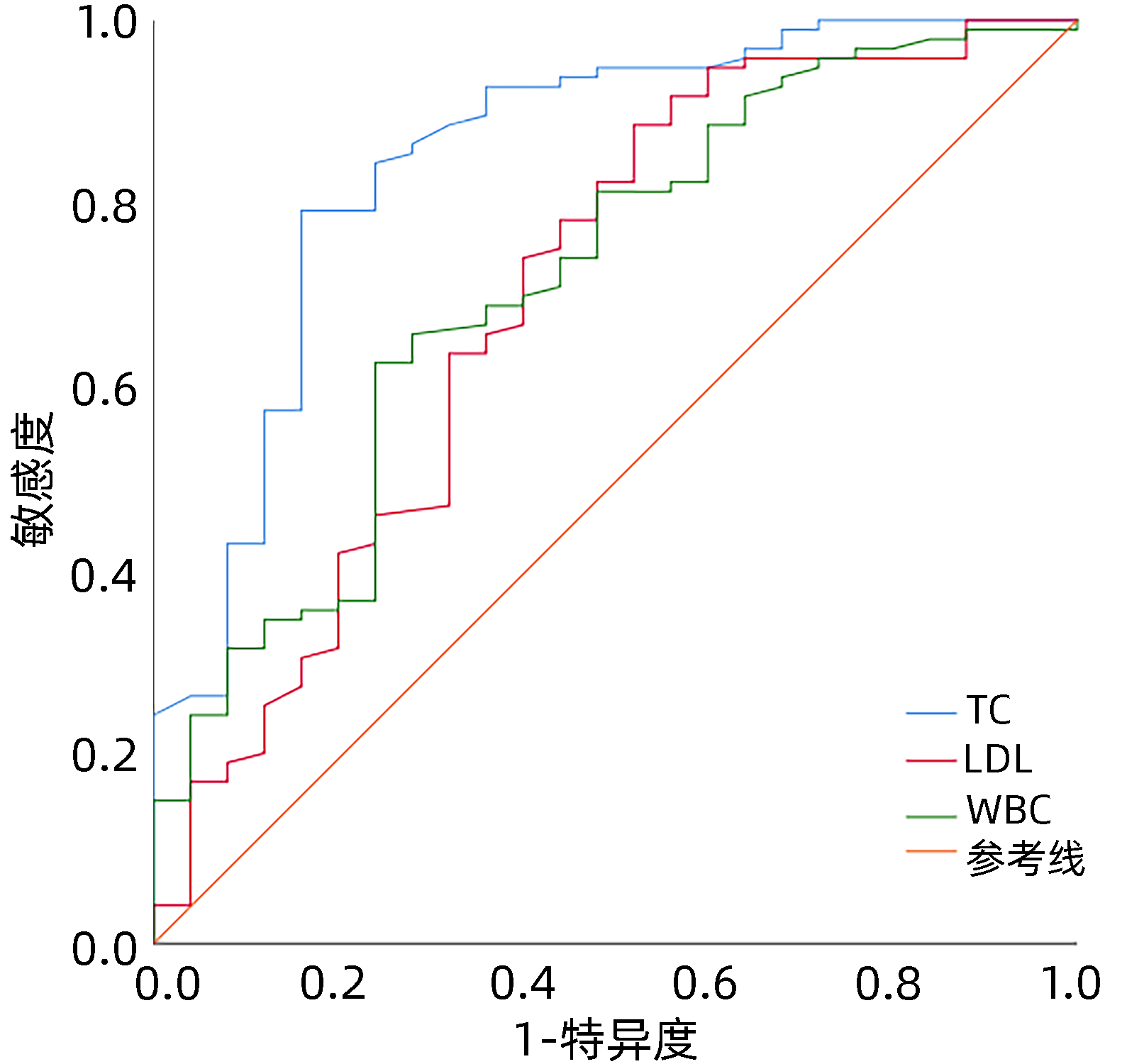
目的 分析血脂指标在慢加急性肝衰竭前期(pre-ACLF)和慢加急性肝衰竭(ACLF)组间的差异,并探讨患者进展的危险因素。 方法 回顾性分析西部战区总医院2012年1月—2020年12月ACLF组(n=118)和pre-ACLF组(n=44)患者的基线年龄、白蛋白、肌酐、血常规、血脂等指标。计量资料服从正态分布的两组间比较采用成组t检验;计量资料不服从正态分布的两组间比较采用Mann-Whitney U检验。计数资料两组间比较采用χ2检验。通过Logistic二元回归进行多因素分析,筛选独立预测因素。使用受试者工作特征曲线(ROC曲线)比较指标的敏感度和特异度,通过约登指数计算临界值。 结果 比较两组间年龄、肌酐、白蛋白、TBil、INR、ALT、AST、TG、TC、HDL、LDL、WBC和中性粒细胞计数水平的差异,发现ACLF组患者的TC[2.02(1.56~2.37) mmol/L vs 3.01(2.57~3.66) mmol/L,Z=5.411,P<0.001]、HDL[0.40(0.25~0.49) mmol/L vs 0.62(0.47~0.75) mmol/L, Z=4.781, P<0.001]、LDL [1.52(1.22~1.84) mmol/L vs 1.93(1.49~2.36) mmol/L, Z=3.146, P=0.002] 水平显著低于pre-ACLF组,ACLF组患者的TBil[352.13(284.32~ 451.19) μmol/L vs 135.80(112.80~154.68) μmol/L, Z=-9.775, P<0.001]、INR[1.96(1.71~2.51)vs 1.39(1.33~1.44), Z=-9.776, P<0.001]、WBC[6.74(5.07~9.19)×109/L vs 5.04(4.13~7.09)×109/L, Z=-3.985, P<0.001]、中性粒细胞水平[4.67(3.40~7.06)×109/L vs 3.30(2.72~5.01)×109/L, Z=-3.676, P<0.001]显著高于pre-ACLF组,两组间年龄、肌酐、白蛋白、ALT、AST和TG水平无显著差异(P值均>0.05)。进一步通过Logistic回归分析发现TC(OR=0.003, 95%CI:0.000~0.068)、LDL(OR=61.901, 95%CI:3.354~1 142.558)、WBC(OR=3.175, 95%CI:1.097~9.185)具有独立预测价值(P值均<0.05),ROC结果显示TC的AUC为0.852,LDL敏感度为0.887,TC特异度为0.840。 结论 血脂指标在pre-ACLF进展到ACLF过程中下降,提示临床医师需要关注pre-ACLF阶段脂质的变化,并及时调整营养方案。 Abstract:Objective To investigate the difference in blood lipid parameters between acute-on-chronic pre-liver failure (pre-ACLF) and acute-on-chronic liver failure (ACLF) and the risk factors for disease progression. Methods A retrospective analysis was performed for the related data of 118 patients with ACLF (ACLF group) and 44 patients with pre-ACLF (pre-ACLF group) who were treated in The General Hospital of Western Theater Command from January 2012 to December 2020, including baseline age, albumin, creatinine, routine blood test results, and blood lipids. The independent samples t-test was used for comparison between normally distributed continuous data; and the Mann-Whitney U test was used for comparison between non-normally distributed continuous data; the chi-square test was used for comparison of categorical data between groups. A binary logistic regression analysis was used for multivariate analysis to identify independent predictive factors. The receiver operating characteristic (ROC) curve was used to compare the sensitivity and specificity of related indicators, and Youden index was used to calculate cut-off values. Results Compared with the pre-ACLF group, the ACLF group had significantly lower levels of total cholesterol (TC)[2.02(1.56-2.37) mmol/L vs 3.01(2.57-3.66) mmol/L, Z=5.411, P < 0.001], high-density lipoprotein [0.40(0.25-0.49) mmol/L vs 0.62(0.47-0.75) mmol/L, Z=4.781, P < 0.001], and low-density lipoprotein (LDL) [1.52(1.22-1.84) mmol/L vs 1.93(1.49-2.36) mmol/L, Z=3.146, P=0.002] and significantly higher levels of total bilirubin [352.13(284.32-451.19) μmol/L vs 135.80(112.80-154.68) μmol/L, Z=-9.775, P < 0.001], international normalized ratio [1.96(1.71-2.51) vs 1.39(1.33-1.44), Z=-9.776, P < 0.001], white blood cell count (WBC) [6.74(5.07-9.19)×109/L vs 5.04(4.13-7.09)×109/L, Z=-3.985, P < 0.001], and neutrophils [4.67(3.40-7.06)×109/L vs 3.30(2.72-5.01)×109/L, Z=-3.676, P < 0.001], while there were no significant differences between the two groups in age, creatinine, albumin, alanine aminotransferase, aspartate aminotransferase, and triglyceride (all P > 0.05). The logistic regression analysis showed that TC (odds ratio [OR]=0.003, 95% confidence interval [CI]: 0.000-0.068, P < 0.05), LDL (OR=61.901, 95%CI: 3.354-1142.558, P < 0.05), and WBC (OR=3.175, 95%CI: 1.097-9.185, P < 0.05) had an independent predictive value, and the ROC analysis showed that the area under the ROC curve of TC was 0.852, the sensitivity of LDL was 0.887, and TC had the best specificity of TC was 0.840. Conclusion There are reductions in blood lipid parameters in the progression from pre-ACLF to ACLF, suggesting that clinicians should pay attention to the changes in lipids in the pre-ACLF stage and adjust the nutritional regimen in a timely manner. -
Key words:
- Acute-On-Chronic Liver Failure /
- Cholesterol /
- Lipoproteins, LDL
-
表 1 pre-ACLF组和ACLF组患者基线数据比较
Table 1. Comparison of baseline data of patients in the pre-ACLF and ACLF groups
指标 pre-ACLF组(n=44) ACLF组(n=118) Z值 P值 年龄(岁) 48.50(36.75~53.75) 46.00(39.75~53.00) 0.228 0.820 肌酐(μmol/L) 72.00(59.00~86.25) 73.50(63.00~87.25) -0.717 0.473 白蛋白(g/L) 34.16(28.83~37.83) 31.60(29.28~34.92) 1.423 0.155 ALT(U/L) 292.70(64.13~1 025.48) 519.55(141.78~1 208.38) -1.514 0.130 AST(U/L) 266.70(103.68~730.83) 373.70(163.95~1 047.90) -1.703 0.089 TC(mmol/L) 3.01(2.57~3.66) 2.02(1.56~2.37) 5.411 <0.001 TG(mmol/L) 1.25(0.88~1.59) 1.10(0.72~1.42) 1.615 0.106 HDL(mmol/L) 0.62(0.47~0.75) 0.40(0.25~0.49) 4.781 <0.001 LDL(mmol/L) 1.93(1.49~2.36) 1.52(1.22~1.84) 3.146 0.002 WBC(×109/L) 5.04(4.13~7.09) 6.74(5.07~9.19) -3.985 <0.001 中性粒细胞计数(×109/L) 3.30(2.72~5.01) 4.67(3.40~7.06) -3.676 <0.001 TBil(μmol/L) 135.80(112.80~154.68) 352.13(284.32~451.19) -9.775 <0.001 INR 1.39(1.33~1.44) 1.96(1.71~2.51) -9.776 <0.001 表 2 pre-ACLF组和ACLF相关指标的Logistic回归结果
Table 2. Results of logistic regression of correlation indicators between pre-ACLF and ACLF groups
变量 单因素分析 多因素分析 OR 95%CI P值 OR 95%CI P值 TC(mmol/L) 0.114 0.046~0.284 <0.001 0.003 0.000~0.068 <0.001 HDL(mmol/L) 0.010 0.001~0.088 <0.001 27.200 0.220~3 360.146 0.179 LDL(mmol/L) 0.198 0.079~0.495 0.001 61.901 3.354~1 142.558 0.006 WBC(×109/L) 1.387 1.163~1.654 <0.001 3.175 1.097~9.185 0.033 中性粒细胞计数(×109/L) 1.399 1.143~1.714 0.001 0.407 0.130~1.276 0.123 白蛋白(g/L) 0.939 0.880~1.002 0.059 肌酐(μmol/L) 1.002 0.997~1.008 0.403 表 3 TC、LDL和WBC的预测效能
Table 3. Predictive performances of TC, LDL, and WBC
参数 P值 AUC 临界值 敏感度 特异度 95%CI TC <0.001 0.852 2.455 mmol/L 0.794 0.840 0.760~0.944 LDL 0.002 0.701 2.060 mmol/L 0.887 0.480 0.574~0.828 WBC 0.001 0.718 5.885×109/L 0.629 0.760 0.604~0.832 -
[1] ARTRU F, MCPHAIL M, TRIANTAFYLLOU E, et al. Lipids in liver failure syndromes: A focus on eicosanoids, specialized pro-resolving lipid mediators and lysophospholipids[J]. Front Immunol, 2022, 13: 867261. DOI: 10.3389/fimmu.2022.867261. [2] LEUTI A, FAZIO D, FAVA M, et al. Bioactive lipids, inflammation and chronic diseases[J]. Adv Drug Deliv Rev, 2020, 159: 133-169. DOI: 10.1016/j.addr.2020.06.028. [3] HASSE JM. Nutrition and liver disease: complex connections[J]. Nutr Clin Pract, 2013, 28(1): 12-14. DOI: 10.1177/0884533612473156. [4] LÓPEZ-VICARIO C, CHECA A, URDANGARIN A, et al. Targeted lipidomics reveals extensive changes in circulating lipid mediators in patients with acutely decompensated cirrhosis[J]. J Hepatol, 2020, 73(4): 817-828. DOI: 10.1016/j.jhep.2020.03.046. [5] WANG XF, WU WY, QIU GK. et al. Plasma lipidomics identifies novel biomarkers in patients with hepatitis B virus-related acute-on-chronic liver failure[J]. Metabolomics, 2017, 13(76). DOI: 10.1007/s11306-017-1215-x. [6] Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, Chinese Medical Association; Severe Liver Disease and Artificial Liver Group, Chinese Society of Hepatology, Chinese Medical Association. Guideline for diagnosis and treatment of liver failure(2018)[J]. J Clin Hepatol, 2019, 35(1): 38-44. DOI: 10.3969/j.issn.1001-5256.2019.01.007.中华医学会感染病学分会肝衰竭与人工肝学组, 中华医学会肝病学分会重型肝病与人工肝学组. 肝衰竭诊治指南(2018年版)[J]. 临床肝胆病杂志, 2019, 35(1): 38-44. DOI: 10.3969/j.issn.1001-5256.2019.01.007. [7] MENG QH, HOU W, YU HW, et al. Resting energy expenditure and substrate metabolism in patients with acute-on-chronic hepatitis B liver failure[J]. J Clin Gastroenterol, 2011, 45(5): 456-461. DOI: 10.1097/MCG.0b013e31820f7f02. [8] European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis[J]. J Hepatol, 2018, 69(2): 406-460. DOI: 10.1016/j.jhep.2018.03.024. [9] WYMANN MP, SCHNEITER R. Lipid signalling in disease[J]. Nat Rev Mol Cell Biol, 2008, 9(2): 162-176. DOI: 10.1038/nrm2335. [10] GUAN M, TU Y, TANG SH. Classification and research progress of acute-on-chronic liver failure[J]. Chin J Clin Gastroenterol, 2021, 33(6): 450-453. DOI: 10.3870/lcxh.j.issn.1005-541X.2021.06.17.官敏, 涂颖, 汤善宏. 慢加急性肝衰竭分型及其研究进展[J]. 临床消化病杂志, 2021, 33(6): 450-453. DOI: 10.3870/lcxh.j.issn.1005-541X.2021.06.17. [11] YANG C, YANG SH, HU JH, et al. Effect of serum total cholesterol level on the prognosis of patients with liver failure[J]. Chin J Integr Tradit West Med Liver Dis, 2021, 31(11): 1053-1056. DOI: 10.3969/j.issn.1005-0264.2021.11.027.杨诚, 杨华升, 胡建华, 等. 血清总胆固醇水平对肝衰竭患者预后的影响[J]. 中西医结合肝病杂志, 2021, 31(11): 1053-1056. DOI: 10.3969/j.issn.1005-0264.2021.11.027. [12] ZHAO J, WANG JH, LI J, et al. Energy metabolism in patients with acute-on-chronic liver failure[J]. Guangdong Med J, 2015, 36(2): 203-207. DOI: 10.13820/j.cnki.gdyx.2015.02.014赵娟, 王金环, 李娟, 等. 慢加急性肝衰竭患者的能量代谢状况[J]. 广东医学, 2015, 36(2): 203-207. DOI: 10.13820/j.cnki.gdyx.2015.02.014 [13] ZHANG Z, PEREIRA SL, LUO M, et al. Evaluation of blood biomarkers associated with risk of malnutrition in older adults: a systematic review and meta-analysis[J]. Nutrients, 2017, 9(8): 829. DOI: 10.3390/nu9080829. [14] WU FP, LI YP, YANG Y, et al. Blood glucose and total cholesterol in the prognosis of patients with liver failure[J]. J Pract Hepatol, 2018, 21(3): 413-416. DOI: 10.3969/j.issn.1672-5069.2018.03.024.吴凤萍, 李亚萍, 杨颖, 等. 血糖和总胆固醇水平对肝衰竭患者预后的影响[J]. 实用肝脏病杂志, 2018, 21(3): 413-416. DOI: 10.3969/j.issn.1672-5069.2018.03.024. [15] DELGADO-COELLO B, BRIONES-ORTA MA, MACÍAS-SILVA M, et al. Cholesterol: recapitulation of its active role during liver regeneration[J]. Liver Int, 2011, 31(9): 1271-1284. DOI: 10.1111/j.1478-3231.2011.02542.x. [16] GREEN P, THEILLA M, SINGER P. Lipid metabolism in critical illness[J]. Curr Opin Clin Nutr Metab Care, 2016, 19(2): 111-115. DOI: 10.1097/MCO.0000000000000253. [17] XIAO C, GONG J, ZHU S, et al. Nomogram based on blood lipoprotein for estimation of mortality in patients with hepatitis B virus-related acute-on-chronic liver failure[J]. BMC Gastroenterol, 2020, 20(1): 188. DOI: 10.1186/s12876-020-01324-w. [18] KAWAMOTO M, MIZUGUCHI T, NAGAYAMA M, et al. Serum lipid and lipoprotein alterations represent recovery of liver function after hepatectomy[J]. Liver Int, 2006, 26(2): 203-210. DOI: 10.1111/j.1478-3231.2005.01217.x. [19] FESSLER MB, PARKS JS. Intracellular lipid flux and membrane microdomains as organizing principles in inflammatory cell signaling[J]. J Immunol, 2011, 187(4): 1529-1535. DOI: 10.4049/jimmunol.1100253. [20] TRIEB M, RAINER F, STADLBAUER V, et al. HDL-related biomarkers are robust predictors of survival in patients with chronic liver failure[J]. J Hepatol, 2020, 73(1): 113-120. DOI: 10.1016/j.jhep.2020.01.026. [21] XU Y, HUANG XP, CHEN L, et al. Value of high-density lipoprotein cholesterol in evaluating the severity and prognosis of hepatitis B virus-associated acute-on-chronic liver failure[J]. J Clin Hepatol, 2021, 37(7): 1632 -1635. DOI: 10.3969/j.issn.1001-5256.2021.07.030.徐英, 黄小平, 陈丽, 等. 高密度脂蛋白胆固醇对HBV相关慢加急性肝衰竭严重程度及预后的预测价值[J]. 临床肝胆病杂志, 2021, 37(7): 1632-1635. DOI: 10.3969/j.issn.1001-5256.2021.07.030. -



 PDF下载 ( 1875 KB)
PDF下载 ( 1875 KB)

 下载:
下载:


