铜代谢失调与细胞损伤及肝病的关系
DOI: 10.3969/j.issn.1001-5256.2023.09.032
利益冲突声明:本文不存在任何利益冲突。
作者贡献声明:高沿航负责课题设计;高沿航和柳涛进行查阅文献并起草论文;高沿航、柳涛、刘雅丽和张飞宇参与文章撰写及修改,校阅论文。
-
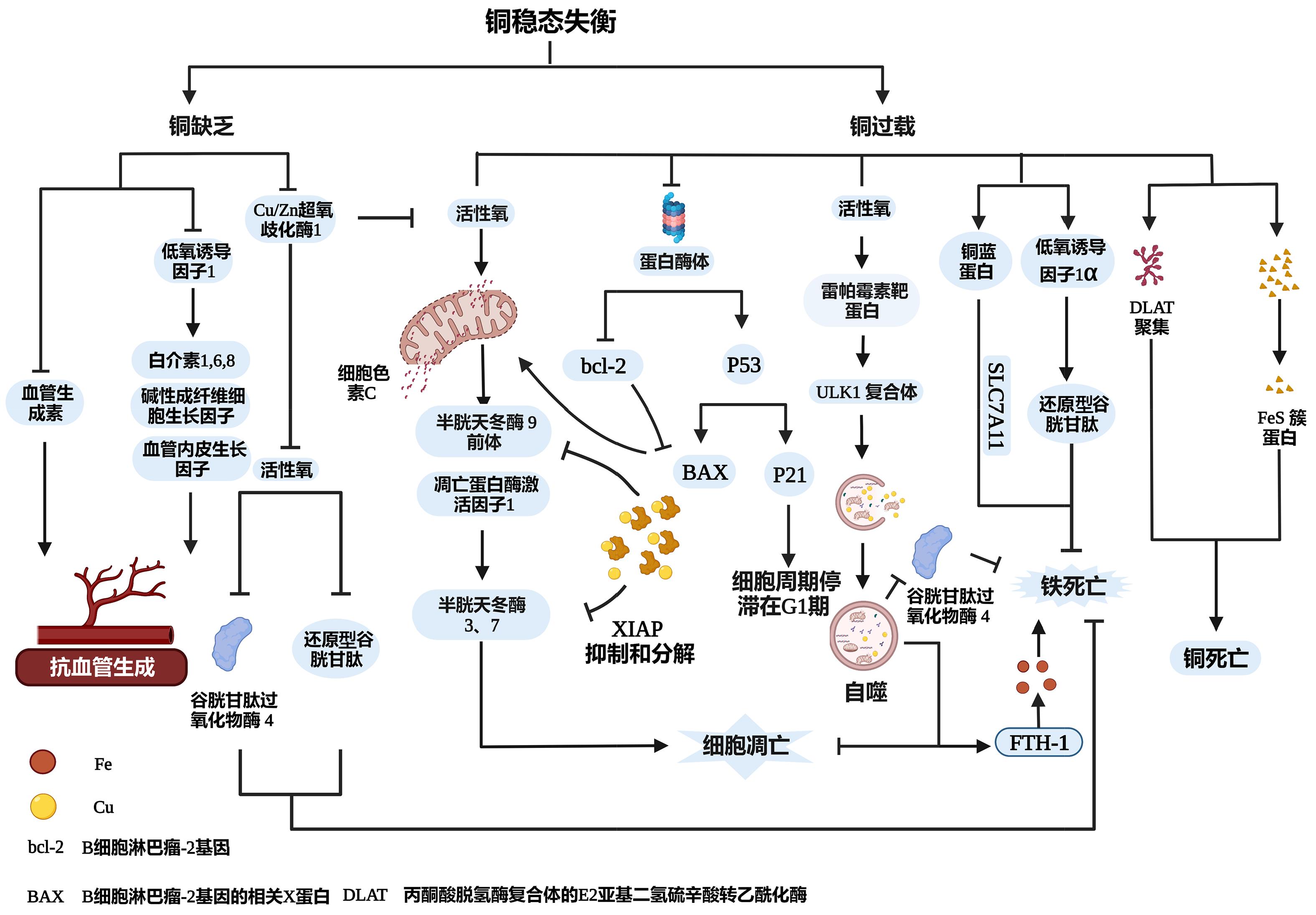
摘要: 铜是人体必需的微量元素,在维持人体健康方面起着至关重要的作用。铜参与人体许多代谢过程,铜代谢失调会导致糖耐量受损和血脂异常等代谢障碍。肝脏在维持体内铜的平衡中起着核心作用,铜缺乏或过量会导致细胞损伤和肝功能障碍。近期有关铜代谢研究的最新进展揭示了铜代谢失调可通过影响氧化应激、蛋白酶体、铜死亡和血管生成引起细胞损伤,并有助于阐明由铜代谢失调引起的肝脏疾病和代谢障碍的假设机制。本文综述了近年来铜代谢失调在细胞损伤/死亡和慢性肝病(包括威尔逊氏病、非酒精性脂肪性肝病、肝细胞癌)中的研究进展,将有助于确定未来的研究重点。Abstract: Copper is an essential trace element in human body and plays an important role in maintaining health in humans. Copper is involved in various metabolic pathways in human body, and copper metabolism disorder may lead to metabolic disorders such as impaired glucose tolerance and dyslipidemia. The liver plays a key role in maintaining copper homeostasis, and copper deficiency or excess may cause cell damage and liver dysfunction. Recent studies on copper metabolism have shown that copper metabolism disorder may result in cell damage by affecting oxidative stress, proteasome, cuproptosis, and angiogenesis and help to clarify the assumed mechanisms of liver diseases and metabolic disorders due to copper metabolism disorder. This article reviews the recent research advances in copper metabolism disorder in cell damage/death and chronic liver diseases, including Wilson’s disease, nonalcoholic fatty liver disease, and hepatocellular carcinoma, which helps to identify future research priorities.
-
Key words:
- Liver Diseases /
- Cell Death /
- Copper Metabolism
-
[1] TSVETKOV P, COY S, PETROVA B, et al. Copper induces cell death by targeting lipoylated TCA cycle proteins[J]. Science, 2022, 375( 6586): 1254- 1261. DOI: 10.1126/science.abf0529. [2] DEV S, KRUSE RL, HAMILTON JP, et al. Wilson disease: update on pathophysiology and treatment[J]. Front Cell Dev Biol, 2022, 10: 871877. DOI: 10.3389/fcell.2022.871877. [3] HIMOTO T, MASAKI T. Current trends of essential trace elements in patients with chronic liver diseases[J]. Nutrients, 2020, 12( 7): 2084. DOI: 10.3390/nu12072084. [4] HUANG R, CHEN H, LIANG J, et al. Dual role of reactive oxygen species and their application in cancer therapy[J]. J Cancer, 2021, 12( 18): 5543- 5561. DOI: 10.7150/jca.54699. [5] ROCHFORD G, MOLPHY Z, KAVANAGH K, et al. Cu(ii) phenanthroline-phenazine complexes dysregulate mitochondrial function and stimulate apoptosis[J]. Metallomics, 2020, 12( 1): 65- 78. DOI: 10.1039/c9mt00187e. [6] HILTON JB, WHITE AR, CROUCH PJ. Metal-deficient SOD1 in amyotrophic lateral sclerosis[J]. J Mol Med(Berl), 2015, 93( 5): 481- 487. DOI: 10.1007/s00109-015-1273-3. [7] GAŁCZYŃSKA K, DRULIS-KAWA Z, ARABSKI M. Antitumor activity of Pt(II), Ru(III) and Cu(II) complexes[J]. Molecules, 2020, 25( 15): 3492. DOI: 10.3390/molecules25153492. [8] SANTORO AM, MONACO I, ATTANASIO F, et al. Copper(II) ions affect the gating dynamics of the 20S proteasome: a molecular and in cell study[J]. Sci Rep, 2016, 6: 33444. DOI: 10.1038/srep33444. [9] TSVETKOV P, DETAPPE A, CAI K, et al. Mitochondrial metabolism promotes adaptation to proteotoxic stress[J]. Nat Chem Biol, 2019, 15( 7): 681- 689. DOI: 10.1038/s41589-019-0291-9. [10] LI Y. Copper homeostasis: Emerging target for cancer treatment[J]. IUBMB Life, 2020, 72( 9): 1900- 1908. DOI: 10.1002/iub.2341. [11] PARK KC, FOUANI L, JANSSON PJ, et al. Copper and conquer: copper complexes of di-2-pyridylketone thiosemicarbazones as novel anti-cancer therapeutics[J]. Metallomics, 2016, 8( 9): 874- 886. DOI: 10.1039/c6mt00105j. [12] XU J, HUA X, YANG R, et al. XIAP interaction with E2F1 and Sp1 via its BIR2 and BIR3 domains specific activated MMP2 to promote bladder cancer invasion[J]. Oncogenesis, 2019, 8( 12): 71. DOI: 10.1038/s41389-019-0181-8. [13] KALITA J, KUMAR V, MISRA UK. A study on apoptosis and anti-apoptotic status in wilson disease[J]. Mol Neurobiol, 2016, 53( 10): 6659- 6667. DOI: 10.1007/s12035-015-9570-y. [14] YANG F, LIAO J, PEI R, et al. Autophagy attenuates copper-induced mitochondrial dysfunction by regulating oxidative stress in chicken hepatocytes[J]. Chemosphere, 2018, 204: 36- 43. DOI: 10.1016/j.chemosphere.2018.03.192. [15] HAZARI Y, BRAVO-SAN PEDRO JM, HETZ C, et al. Autophagy in hepatic adaptation to stress[J]. J Hepatol, 2020, 72( 1): 183- 196. DOI: 10.1016/j.jhep.2019.08.026. [16] POLISHCHUK EV, MEROLLA A, LICHTMANNEGGER J, et al. Activation of autophagy, observed in liver tissues from patients with Wilson disease and from ATP7B-deficient animals, protects hepatocytes from copper-induced apoptosis[J]. Gastroenterology, 2019, 156( 4): 1173- 1189. DOI: 10.1053/j.gastro.2018.11.032. [17] GAO W, HUANG Z, DUAN J, et al. Elesclomol induces copper-dependent ferroptosis in colorectal cancer cells via degradation of ATP7A[J]. Mol Oncol, 2021, 15( 12): 3527- 3544. DOI: 10.1002/1878-0261.13079. [18] LI F, WU X, LIU H, et al. Copper depletion strongly enhances ferroptosis via mitochondrial perturbation and reduction in antioxidative mechanisms[J]. Antioxidants(Basel), 2022, 11( 11): 2084. DOI: 10.3390/antiox11112084. [19] GUO H, OUYANG Y, YIN H, et al. Induction of autophagy via the ROS-dependent AMPK-mTOR pathway protects copper-induced spermatogenesis disorder[J]. Redox Biol, 2022, 49: 102227. DOI: 10.1016/j.redox.2021.102227. [20] YANG M, WU X, HU J, et al. COMMD10 inhibits HIF1α/CP loop to enhance ferroptosis and radiosensitivity by disrupting Cu-Fe balance in hepatocellular carcinoma[J]. J Hepatol, 2022, 76( 5): 1138- 1150. DOI: 10.1016/j.jhep.2022.01.009. [21] CHEN M, ZHENG J, LIU G, et al. Ceruloplasmin and hephaestin jointly protect the exocrine pancreas against oxidative damage by facilitating iron efflux[J]. Redox Biol, 2018, 17: 432- 439. DOI: 10.1016/j.redox.2018.05.013. [22] ZISCHKA H, LICHTMANNEGGER J, SCHMITT S, et al. Liver mitochondrial membrane crosslinking and destruction in a rat model of Wilson disease[J]. J Clin Invest, 2011, 121( 4): 1508- 1518. DOI: 10.1172/JCI45401. [23] HAMILTON JP, KOGANTI L, MUCHENDITSI A, et al. Activation of liver X receptor/retinoid X receptor pathway ameliorates liver disease in Atp7B(-/-)(Wilson disease) mice[J]. Hepatology, 2016, 63( 6): 1828- 1841. DOI: 10.1002/hep.28406. [24] MEDICI V, SARODE GV, NAPOLI E, et al. mtDNA depletion-like syndrome in Wilson disease[J]. Liver Int, 2020, 40( 11): 2776- 2787. DOI: 10.1111/liv.14646. [25] SHRIBMAN S, POUJOIS A, BANDMANN O, et al. Wilson’s disease: update on pathogenesis, biomarkers and treatments[J]. J Neurol Neurosurg Psychiatry, 2021, 92( 10): 1053- 1061. DOI: 10.1136/jnnp-2021-326123. [26] PFEIFFENBERGER J, MOGLER C, GOTTHARDT DN, et al. Hepatobiliary malignancies in Wilson disease[J]. Liver Int, 2015, 35( 5): 1615- 1622. DOI: 10.1111/liv.12727. [27] van MEER S, de MAN RA, van DEN BERG AP, et al. No increased risk of hepatocellular carcinoma in cirrhosis due to Wilson disease during long-term follow-up[J]. J Gastroenterol Hepatol, 2015, 30( 3): 535- 539. DOI: 10.1111/jgh.12716. [28] YOUNOSSI Z, TACKE F, ARRESE M, et al. Global perspectives on nonalcoholic fatty liver disease and nonalcoholic steatohepatitis[J]. Hepatology, 2019, 69( 6): 2672- 2682. DOI: 10.1002/hep.30251. [29] HEFFERN MC, PARK HM, AU-YEUNG HY, et al. In vivo bioluminescence imaging reveals copper deficiency in a murine model of nonalcoholic fatty liver disease[J]. Proc Natl Acad Sci U S A, 2016, 113( 50): 14219- 14224. DOI: 10.1073/pnas.1613628113. [30] TOSCO A, FONTANELLA B, DANISE R, et al. Molecular bases of copper and iron deficiency-associated dyslipidemia: a microarray analysis of the rat intestinal transcriptome[J]. Genes Nutr, 2010, 5( 1): 1- 8. DOI: 10.1007/s12263-009-0153-2. [31] SONG M, SCHUSCHKE DA, ZHOU Z, et al. High fructose feeding induces copper deficiency in Sprague-Dawley rats: a novel mechanism for obesity related fatty liver[J]. J Hepatol, 2012, 56( 2): 433- 440. DOI: 10.1016/j.jhep.2011.05.030. [32] AIGNER E, THEURL I, HAUFE H, et al. Copper availability contributes to iron perturbations in human nonalcoholic fatty liver disease[J]. Gastroenterology, 2008, 135( 2): 680- 688. DOI: 10.1053/j.gastro.2008.04.007. [33] TALLINO S, DUFFY M, RALLE M, et al. Nutrigenomics analysis reveals that copper deficiency and dietary sucrose up-regulate inflammation, fibrosis and lipogenic pathways in a mature rat model of nonalcoholic fatty liver disease[J]. J Nutr Biochem, 2015, 26( 10): 996- 1006. DOI: 10.1016/j.jnutbio.2015.04.009. [34] BUZZETTI E, PARIKH PM, GERUSSI A, et al. Gender differences in liver disease and the drug-dose gender gap[J]. Pharmacol Res, 2017, 120: 97- 108. DOI: 10.1016/j.phrs.2017.03.014. [35] LAN Y, WU S, WANG Y, et al. Association between blood copper and nonalcoholic fatty liver disease according to sex[J]. Clin Nutr, 2021, 40( 4): 2045- 2052. DOI: 10.1016/j.clnu.2020.09.026. [36] STÄTTERMAYER AF, TRAUSSNIGG S, AIGNER E, et al. Low hepatic copper content and PNPLA3 polymorphism in non-alcoholic fatty liver disease in patients without metabolic syndrome[J]. J Trace Elem Med Biol, 2017, 39: 100- 107. DOI: 10.1016/j.jtemb.2016.08.006. [37] EL-RAYAH EA, TWOMEY PJ, WALLACE EM, et al. Both α-1-antitrypsin Z phenotypes and low caeruloplasmin levels are over-represented in alcohol and nonalcoholic fatty liver disease cirrhotic patients undergoing liver transplant in Ireland[J]. Eur J Gastroenterol Hepatol, 2018, 30( 4): 364- 367. DOI: 10.1097/MEG.0000000000001056. [38] YANG JD, HAINAUT P, GORES GJ, et al. A global view of hepatocellular carcinoma: trends, risk, prevention and management[J]. Nat Rev Gastroenterol Hepatol, 2019, 16( 10): 589- 604. DOI: 10.1038/s41575-019-0186-y. [39] BALDARI S, DI ROCCO G, TOIETTA G. Current biomedical use of copper chelation therapy[J]. Int J Mol Sci, 2020, 21( 3): 1069. DOI: 10.3390/ijms21031069. [40] DAVIS CI, GU X, KIEFER RM, et al. Altered copper homeostasis underlies sensitivity of hepatocellular carcinoma to copper chelation[J]. Metallomics, 2020, 12( 12): 1995- 2008. DOI: 10.1039/d0mt00156b. [41] PORCU C, ANTONUCCI L, BARBARO B, et al. Copper/MYC/CTR1 interplay: a dangerous relationship in hepatocellular carcinoma[J]. Oncotarget, 2018, 9( 10): 9325- 9343. DOI: 10.18632/oncotarget.24282. [42] ZHU J, HUANG S, WU G, et al. Lysyl oxidase is predictive of unfavorable outcomes and essential for regulation of vascular endothelial growth factor in hepatocellular carcinoma[J]. Dig Dis Sci, 2015, 60( 10): 3019- 3031. DOI: 10.1007/s10620-015-3734-5. [43] CHOI J, CHUNG T, RHEE H, et al. Increased expression of the matrix-modifying enzyme lysyl oxidase-like 2 in aggressive hepatocellular carcinoma with poor prognosis[J]. Gut Liver, 2019, 13( 1): 83- 92. DOI: 10.5009/gnl17569. [44] MORISAWA A, OKUI T, SHIMO T, et al. Ammonium tetrathiomolybdate enhances the antitumor effects of cetuximab via the suppression of osteoclastogenesis in head and neck squamous carcinoma[J]. Int J Oncol, 2018, 52( 3): 989- 999. DOI: 10.3892/ijo.2018.4242. [45] SINGLA A, CHEN Q, SUZUKI K, et al. Regulation of murine copper homeostasis by members of the COMMD protein family[J]. Dis Model Mech, 2021, 14( 1): dmm045963. DOI: 10.1242/dmm.045963. [46] YOSHII J, YOSHIJI H, KURIYAMA S, et al. The copper-chelating agent, trientine, suppresses tumor development and angiogenesis in the murine hepatocellular carcinoma cells[J]. Int J Cancer, 2001, 94( 6): 768- 773. DOI: 10.1002/ijc.1537. [47] REZAEI A, MAHMOODI M, MOHAMMADIZADEH F, et al. A novel copper(II) complex activated both extrinsic and intrinsic apoptotic pathways in liver cancerous cells[J]. J Cell Biochem, 2019, 120( 8): 12280- 12289. DOI: 10.1002/jcb.28491. [48] FANG AP, CHEN PY, WANG XY, et al. Serum copper and zinc levels at diagnosis and hepatocellular carcinoma survival in the Guangdong Liver Cancer Cohort[J]. Int J Cancer, 2019, 144( 11): 2823- 2832. DOI: 10.1002/ijc.31991. [49] BAJ J, TERESIŃSKI G, FORMA A, et al. Chronic alcohol abuse alters hepatic trace element concentrations-metallomic study of hepatic elemental composition by means of ICP-OES[J]. Nutrients, 2022, 14( 3): 546. DOI: 10.3390/nu14030546. [50] ARAIN SA, KAZI TG, AFRIDI HI, et al. Estimation of copper and iron burden in biological samples of various stages of hepatitis C and liver cirrhosis patients[J]. Biol Trace Elem Res, 2014, 160( 2): 197- 205. DOI: 10.1007/s12011-014-0058-9. -



 PDF下载 ( 1115 KB)
PDF下载 ( 1115 KB)


 下载:
下载: