白蛋白相关比值对HBV相关慢加急性肝衰竭患者死亡风险的预测价值
DOI: 10.3969/j.issn.1001-5256.2023.11.011
Value of albumin-related ratios in predicting the risk of death in patients with hepatitis B virus-related acute-on-chronic liver failure
-
摘要:
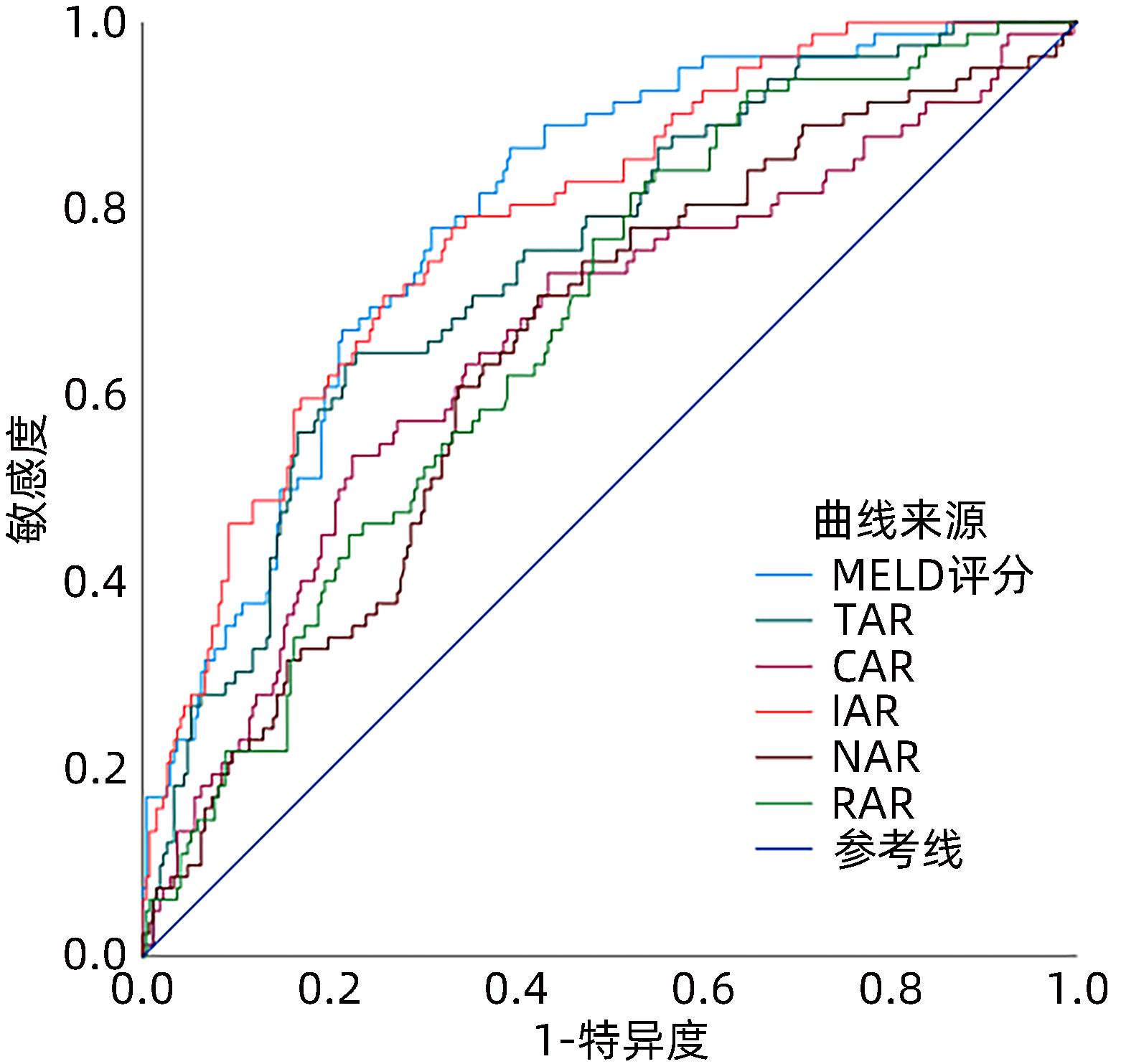
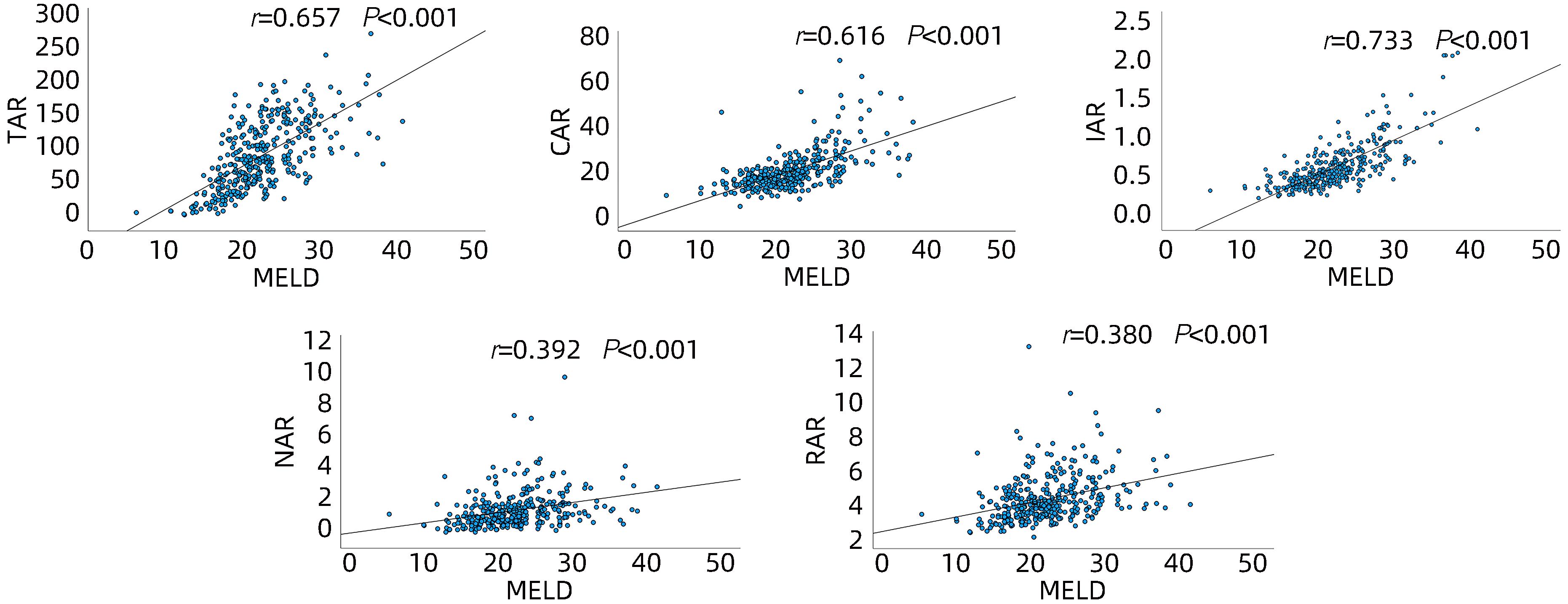
目的 比较分析白蛋白相关比值[总胆红素/白蛋白比值(TAR)、肌酐/白蛋白比值(CAR)、凝血酶原时间国际标准化比值/白蛋白比值(IAR)、中性粒细胞计数/白蛋白比值(NAR)和红细胞分布宽度/白蛋白比值(RAR)]对HBV相关慢加急性肝衰竭(HBV-ACLF)患者短期预后的预测价值。 方法 对2017年6月—2022年2月西南医科大学附属医院感染科收治的354例HBV-ACLF患者进行回顾性研究,根据随访3个月时的转归分为生存组(n=272)和死亡组(n=82),记录患者的年龄、性别、并发症以及入院后首次的血常规、肝功能、凝血等检验指标,同时计算白蛋白相关比值、MELD评分。符合正态分布的计量资料两组间比较采用t检验;非正态分布计量资料两组间比较采用Mann-Whitney U检验;计数资料组间比较采用χ2检验。白蛋白相关比值与MELD评分之间的相关性分析采用Spearman相关性检验。采用Logistic回归分析探讨MELD评分、TAR、CAR、IAR、NAR和RAR与不良预后的关系。采用受试者工作特征曲线(ROC曲线)下面积(AUC)分析白蛋白相关比值及MELD评分对HBV-ACLF患者短期预后的预测准确性。使用De-Long检验进行AUC之间的比较。 结果 生存组的MELD评分(Z=-8.071)、TAR(Z=-6.695)、CAR(Z=-4.463)、IAR(Z=-7.912)、NAR(Z=-4.061)、RAR(Z=-4.788)比死亡组更低,差异均有统计学意义(P值均<0.001)。MELD评分与CAR(r=0.616)、IAR(r=0.733)、TAR(r=0.657)、NAR(r=0.392),RAR(r=0.380)均呈正相关(P值均<0.001)。将MELD评分及白蛋白相关比值进行多因素回归分析,高TAR(OR=1.014,95%CI:1.008~1.020,P<0.001)和高IAR(OR=22.052,95%CI:6.937~70.103,P<0.001)被确定为死亡的独立危险因素。通过绘制白蛋白相关比值及MELD评分的ROC曲线来评估这些指标对死亡率的区分能力,得到相应的AUC值,MELD:0.794、TAR:0.744、CAR:0.663、IAR:0.788、NAR:0.648、RAR:0.674;其中,MELD的敏感度最高为86.59%,而CAR的特异度最高为77.57%。当TAR和IAR联合使用时,其AUC值为0.809,敏感度和特异度分别为76.8%和71.3%。对HBV-ACLF进行亚组分析显示,A型和C型患者TAR和IAR联合使用时,其AUC值最高,分别为0.884、0.733。 结论 TAR、IAR可作为预测HBV-ACLF患者90天死亡率的一种简单有效的预后工具。 -
关键词:
- 慢加急性肝功能衰竭 /
- 乙型肝炎病毒 /
- 血清白蛋白 /
- 预后
Abstract:Objective To investigate and compare the value of albumin-related ratios [total bilirubin-to-albumin ratio (TAR), creatinine-to-albumin ratio (CAR), prothrombin time-international normalized ratio-to-albumin ratio (IAR), neutrophil count-to-albumin ratio (NAR), and red blood cell distribution width-to-albumin ratio (RAR)] in predicting the short-term prognosis of patients with hepatitis B virus-related acute-on-chronic liver failure (HBV-ACLF). Methods A retrospective analysis was performed for 354 patients with HBV-ACLF who were admitted to Department of Infectious Diseases, The Affiliated Hospital of Southwest Medical University, from June 2017 to February 2022, and according to their prognosis at 3 months of follow-up, they were divided into survival group (n=272) and death group (n=82). Related indices were recorded for all patients, including age, sex, complications, and the results of routine blood test, liver function, and coagulation for the first time after admission, and albumin-related ratios and Model for End-Stage Liver Disease (MELD) score were calculated. The t-test was used for comparison of normally distributed continuous data between groups, and the Mann-Whitney U test was used for comparison of non-normally distribution continuous data between groups; the chi-square test was used for comparison of categorical data between groups. The Spearman correlation test was used to investigate the correlation between albumin-related ratios and MELD score. The Logistic regression analysis was used to explore the association of MELD score, TAR, CAR, IAR, NAR, and RAR with poor prognosis. The area under the ROC curve (AUC) was used to as sess the accuracy of albumin-related ratios and MELD score in predicting the short-term prognosis of HBV-ACLF patients, and the De-Long test was used for the comparison of AUC. Results Compared with the death group, the survival group had significantly lower MELD score (Z=-8.071, P<0.001), TAR (Z=-6.695, P<0.001), CAR (Z=-4.463, P<0.001), IAR (Z=-7.912, P<0.001), NAR (Z=-4.061, P<0.001), and RAR (Z=-4.788, P<0.001). MELD score was positively correlated with CAR (r=0.616, P<0.001), IAR (r=0.733, P<0.001), TAR (r=0.657, P<0.001), NAR (r=0.392, P<0.001), and RAR (r=0.380, P<0.001). The multivariate regression analysis of MELD score and albumin-related ratios showed that high TAR (odds ratio [OR]=1.014, 95% confidence interval [CI]: 1.008 — 1.020, P<0.001) and high IAR (OR=22.052, 95%CI: 6.937 — 70.103, P<0.001) were independent risk factors for death. The ROC curves were plotted for albumin-related ratios and MELD score to evaluate their discriminatory ability for mortality, and the results showed that MELD score, TAR, CAR, IAR, NAR, and RAR had an AUC of 0.794, 0.744, 0.663, 0.788, 0.648, and 0.674, respectively, among which MELD score had the highest sensitivity of 86.59% and CAR had the highest specificity of 77.57%. TAR combined with IAR had an AUC of 0.809, with a sensitivity of 76.8% and a specificity of 71.3%. Subgroup analysis of HBV-ACLF showed that TAR combined with IAR had the highest AUC values of 0.884 and 0.733, respectively, in patients with type A or type C HBV-ACLF. Conclusion TAR and IAR can be used as simple and effective prognostic tools to predict the 90-day mortality of HBV-ACLF patients. -
Key words:
- Acute-On-Chronic Liver Failure /
- Hepatitis B virus /
- Serum Albumin /
- Prognosis
-
表 1 生存组和死亡组基线特征的比较
Table 1. Comparisons of baseline characteristics between the survivors and non-survivors
指标 生存组(n=272) 死亡组(n=82) 统计值 P值 性别(男/女) 221/51 71/11 χ2=1.241 0.265 年龄(岁) 46.99±12.54 52.46±11.32 t=-3.541 <0.001 分型[例(%)] χ2=21.159 <0.001 A型 144(52.9) 21(25.6) B型 14(5.1) 3(3.7) C型 114(41.9) 58(70.7) 腹水(有/无,例) 145/127 70/12 χ2=27.151 <0.001 肝性脑病(有/无,例) 19/253 30/52 χ2=46.289 <0.001 肝肾综合征(有/无,例) 3/269 3/79 χ2=1.174 0.279 上消化道出血(有/无,例) 2/270 5/77 χ2=6.785 0.009 细菌感染(有/无,例) 152/120 75/7 χ2=34.673 <0.001 HBV DNA(107 IU/mL) 0.240(0.002~2.270) 0.060(0.001~1.450) Z=-1.066 0.286 ALT(U/L) 841.90(252.35~1 453.93) 443.95(186.45~1 206.18) Z=-2.638 0.008 AST(U/L) 510.25(217.53~1 089.83) 342.04(195.25~996.05) Z=-1.555 0.120 ALP(U/L) 150.65(120.00~186.73) 151.85(122.23~193.63) Z=-0.268 0.788 GGT(U/L) 118.70(86.53~187.85) 97.10(65.28~148.23) Z=-3.041 0.002 Alb(g/dL) 3.27±0.48 2.96±0.46 t=5.193 <0.001 TBil(μmol/L) 251.50(160.88~358.18) 363.12(290.35~482.85) Z=-5.820 <0.001 DBil(μmol/L) 176.65(115.53~250.96) 240.75(174.15~302.23) Z=-4.795 <0.001 CREA(μmol/L) 65.25(55.63~73.75) 68.85(57.85~80.53) Z=-2.087 0.037 INR 1.77(1.54~2.09) 2.29(1.93~3.02) Z=-7.552 <0.001 WBC(×109/L) 6.41(4.96~8.17) 7.06(5.81~9.06) Z=-2.013 0.044 NEU(×109/L) 4.39(3.19~6.04) 5.18(4.13~6.63) Z=-2.958 0.003 Hb(g/L) 135(120~148) 129(115~142) Z=-2.703 0.007 RDW(%) 14.30(13.50~15.80) 14.90(13.80~17.03) Z=-2.693 0.007 PLT(×109/L) 118.00(84.00~159.00) 96.00(69.00~126.25) Z=-3.315 0.001 MELD评分 19.68(17.08~22.49) 24.88(21.96~28.26) Z=-8.071 <0.001 TAR 80.61(49.01~114.72) 136.86(89.17~164.43) Z=-6.695 <0.001 CAR 19.44(16.53~23.09) 23.80(19.16~29.15) Z=-4.463 <0.001 IAR 0.56(0.45~0.69) 0.79(0.63~1.05) Z=-7.912 <0.001 NAR 1.34(0.94~1.96) 1.80(1.32~2.34) Z=-4.061 <0.001 RAR 4.47(3.89~5.29) 5.10(4.50~6.09) Z=-4.788 <0.001 表 2 白蛋白相关比值与MELD评分的Logistic 回归分析
Table 2. Logistic regression analysis of albumin-related ratios and MELD score
指标 单因素分析 多因素分析 OR 95%CI P值 OR 95%CI P值 MELD 1.245 1.173~1.321 <0.001 TAR 1.019 1.013~1.024 <0.001 1.014 1.008~1.020 <0.001 CAR 1.053 1.026~1.080 <0.001 IAR 43.623 14.274~133.313 <0.001 22.052 6.937~70.103 <0.001 NAR 1.516 1.205~1.908 <0.001 RAR 1.402 1.187~1.655 <0.001 表 3 不同评分系统预测HBV-ACLF患者总人群90天死亡率的准确性
Table 3. Prognostic accuracies of different scoring systems for predicting 90-day mortality in total HBV-ACLF patients
指标 AUC P值 阈值 敏感度(%) 特异度(%) NPV(%) PPV(%) MELD评分 0.794 <0.001 20.90 86.59 60.66 93.74 39.94 TAR 0.744 <0.001 118.86 64.63 77.21 87.84 46.14 CAR 0.6631)2) <0.001 23.61 53.66 77.57 84.71 41.95 IAR 0.7883) <0.001 0.67 70.73 74.26 89.36 45.36 NAR 0.6481)2)4) <0.001 1.48 70.73 57.72 86.72 33.57 RAR 0.6741)2)4) <0.001 4.38 81.71 47.79 89.64 32.10 TAR-IAR 0.8092)3)5)6) <0.001 0.20 76.80 71.30 91.05 44.70 注:与MELD评分比较,1) P<0.001;与TAR比较,2) P<0.05;与CAR比较,3) P<0.001;与IAR比较,4) P<0.001;与NAR比较,5) P<0.001;与RAR比较,6) P<0.001。 表 4 不同评分系统预测A型HBV-ACLF患者90天死亡率的效能
Table 4. Prognostic accuracies of different scoring systems for predicting 90-day mortality in patients with type A HBV-ACLF
指标 AUC P值 阈值 敏感度(%) 特异度(%) NPV(%) PPV(%) MELD评分 0.858 <0.001 23.01 76.19 86.11 96.13 44.38 TAR 0.817 <0.001 130.22 61.90 87.50 94.04 41.87 CAR 0.6761) 0.017 23.42 57.14 85.42 93.19 36.31 IAR 0.8483) <0.001 0.60 85.71 71.53 97.18 30.46 NAR 0.7181)4) <0.001 1.67 76.19 72.22 95.42 28.52 RAR 0.7281)4) <0.001 3.98 100.00 43.75 100.00 20.55 TAR-IAR 0.8842)3)5)6) <0.001 0.11 90.48 75.7 98.20 35.13 注:与MELD评分比较,1) P<0.05;与TAR比较,2) P<0.05;与CAR比较,3) P<0.05;与IAR比较,4) P<0.05;与NAR比较,5) P<0.05;与RAR比较,6) P<0.05。 表 5 不同评分系统预测C型HBC-ACLF患者90天死亡率的效能
Table 5. Prognostic accuracies of different scoring systems for predicting 90-day mortality in patients with type C HBV-ACLF
指标 AUC P值 阈值 敏感度(%) 特异度(%) NPV(%) PPV(%) MELD评分 0.730 <0.001 21.92 77.59 58.77 83.77 48.89 TAR 0.690 <0.001 121.82 65.52 72.81 80.60 55.05 CAR 0.6061) 0.024 26.06 43.10 77.10 72.74 48.99 IAR 0.7123) <0.001 0.69 68.97 66.67 80.87 51.26 NAR 0.5921)2)4) 0.397 1.48 70.69 50.88 77.35 42.25 RAR 0.5681)2)4)5) 0.128 4.38 89.66 32.46 86.06 40.29 TAR-IAR 0.7333)6) <0.001 0.45 53.45 87.72 78.76 68.87 注:与MELD评分比较,1) P<0.05;与TAR比较,2) P<0.05;与CAR比较,3) P<0.05;与IAR比较,4) P<0.05;与NAR比较,5) P<0.001;与RAR比较,6) P<0.001。 -
[1] MOREAU R, GAO B, PAPP M, et al. Acute-on-chronic liver failure: A distinct clinical syndrome[J]. J Hepatol, 2021, 75( Suppl 1): S27- S35. DOI: 10.1016/j.jhep.2020.11.047. [2] SARIN SK, KEDARISETTY CK, ABBAS Z, et al. Acute-on-chronic liver failure: Consensus recommendations of the Asian Pacific Association for the Study of the Liver(APASL) 2014[J]. Hepatol Int, 2014, 8( 4): 453- 471. DOI: 10.1007/s12072-014-9580-2. [3] ZHAO RH, SHI Y, ZHAO H, et al. Acute-on-chronic liver failure in chronic hepatitis B: An update[J]. Expert Rev Gastroenterol Hepatol, 2018, 12( 4): 341- 350. DOI: 10.1080/17474124.2018.1426459. [4] KARVELLAS CJ, FRANCOZ C, WEISS E. Liver transplantation in acute-on-chronic liver failure[J]. Transplantation, 2021, 105( 7): 1471- 1481. DOI: 10.1097/TP.0000000000003550. [5] LI H, ZHENG J, CHEN LA, et al. The scoring systems in predicting short-term outcomes in patients with hepatitis B virus-related acute-on-chronic liver failure[J]. Ann Palliat Med, 2020, 9( 5): 3048- 3058. DOI: 10.21037/apm-20-608. [6] QUINLAN GJ, MARTIN GS, EVANS TW. Albumin: Biochemical properties and therapeutic potential[J]. Hepatology, 2005, 41( 6): 1211- 1219. DOI: 10.1002/hep.20720. [7] BERNARDI M, RICCI CS, ZACCHERINI G. Role of human albumin in the management of complications of liver cirrhosis[J]. J Clin Exp Hepatol, 2014, 4( 4): 302- 311. DOI: 10.1016/j.jceh.2014.08.007. [8] ARROYO V, CLÀRIA J. Acute-on-chronic liver failure, human serum albumin, and immune modulation: The beginning of an exciting adventure[J]. Clin Gastroenterol Hepatol, 2018, 16( 5): 633- 636. DOI: 10.1016/j.cgh.2017.12.008. [9] HAN Z, HE X, PENG SQ. Neutrophil count to albumin ratio as a prognostic indicator for HBV-associated decompensated cirrhosis[J]. J Clin Lab Anal, 2021, 35( 4): e23730. DOI: 10.1002/jcla.23730. [10] CHOI JS, CHUNG KS, LEE EH, et al. The role of bilirubin to albumin ratio as a predictor for mortality in critically ill patients without existing liver or biliary tract disease[J]. Acute Crit Care, 2020, 35( 1): 24- 30. DOI: 10.4266/acc.2019.00738. [11] LU CD, LONG JY, LIU HY, et al. Red blood cell distribution width-to-albumin ratio is associated with all-cause mortality in cancer patients[J]. J Clin Lab Anal, 2022, 36( 5): e24423. DOI: 10.1002/jcla.24423. [12] NI QW, WANG X, WANG J, et al. The red blood cell distribution width-albumin ratio: A promising predictor of mortality in heart failure patients-A cohort study[J]. Clin Chim Acta, 2022, 527: 38- 46. DOI: 10.1016/j.cca.2021.12.027. [13] YıLMAZ MF, KARAGÖZ A, ZEREN G, et al. Relationship between in-hospital mortality and creatinine/albumin in patients with ST-elevation myocardial infarction without standard modifiable risk factors[J]. Biomark Med, 2022, 16( 14): 1043- 1053. DOI: 10.2217/bmm-2022-0241. [14] ÜLGER Y, DELIK A. Prognostic value of international normalized ratio-to-albumin ratio and ferritin level in chronic liver patients with hepatocellular carcinoma[J]. J Gastrointest Cancer, 2022, 53( 4): 1028- 1033. DOI: 10.1007/s12029-021-00738-3. [15] Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, Chinese Medical Association; Severe Liver Disease and Artificial Liver Group, Chinese Society of Hepatology, Chinese Medical Association. Guideline for diagnosis and treatment of liver failure(2018)[J]. J Clin Hepatol, 2019, 35( 1): 38- 44. DOI: 10.3969/j.issn.1001-5256.2019.01.007.中华医学会感染病学分会肝衰竭与人工肝学组, 中华医学会肝病学分会重型肝病与人工肝学组. 肝衰竭诊治指南(2018年版)[J]. 临床肝胆病杂志, 2019, 35( 1): 38- 44. DOI: 10.3969/j.issn.1001-5256.2019.01.007. [16] KAMATH PS, WIESNER RH, MALINCHOC M, et al. A model to predict survival in patients with end-stage liver disease[J]. Hepatology, 2001, 33( 2): 464- 470. DOI: 10.1053/jhep.2001.22172. [17] CLÀRIA J, STAUBER RE, COENRAAD MJ, et al. Systemic inflammation in decompensated cirrhosis: Characterization and role in acute-on-chronic liver failure[J]. Hepatology, 2016, 64( 4): 1249- 1264. DOI: 10.1002/hep.28740. [18] WANG J, HUANG R, YAN XM, et al. Red blood cell distribution width: A promising index for evaluating the severity and long-term prognosis of hepatitis B virus-related diseases[J]. Dig Liver Dis, 2020, 52( 4): 440- 446. DOI: 10.1016/j.dld.2019.12.144. [19] QIN J, QIANG L, CHEN W, et al. Red blood cell distribution width is a independent prognostic indicator for mortality in patients with HBV related acute-on-chronic liver failure[J]. J South Med Univ, 2018, 38( 11): 1354- 1359. DOI: 10.12122/j.issn.1673-4254.2018.11.13.秦娇, 强丽, 陈文, 等. 红细胞分布宽度可作为乙型肝炎相关慢加急性肝衰竭患者短期死亡的独立预测因子[J]. 南方医科大学学报, 2018, 38( 11): 1354- 1359. DOI: 10.12122/j.issn.1673-4254.2018.11.13. [20] RUI CR, LEVADA-PIRES AC, SILVA EBD, et al. The critical role of cell metabolism for essential neutrophil functions[J]. Cell Physiol Biochem, 2020, 54( 4): 629- 647. DOI: 10.33594/000000245. [21] SIMBRUNNER B, TRAUNER M, REIBERGER T, et al. Recent advances in the understanding and management of hepatorenal syndrome[J]. Fac Rev, 2021, 10: 48. DOI: 10.12703/r/10-48. [22] CHEN MJ, LI X, TANG SH. Progress of multidimensional evaluation of liver function in prognosis of patients with liver failure[J]. Clin J Med Offic, 2023, 51( 9): 901- 903, 907. DOI: 10.16680/j.1671-3826.2023.09.05.陈美娟, 李雪, 汤善宏. 多维度评估肝功能在肝衰竭患者预后中研究进展[J]. 临床军医杂志, 2023, 51( 9): 901- 903, 907. DOI: 10.16680/j.1671-3826.2023.09.05. [23] GAO F, CAI MX, LIN MT, et al. Prognostic value of international normalized ratio to albumin ratio among critically ill patients with cirrhosis[J]. Eur J Gastroenterol Hepatol, 2019, 31( 7): 824- 831. DOI: 10.1097/MEG.0000000000001339. [24] GAO X, ZHAO CJ, HU SH. Short-term prognostic value of age-bilirubin-international normalized ratio-creatinine score in patients with hepatitis B virus-related acute-on-chronic liver failure[J/CD]. Chin J Exp Clin Infect Dis(Electronic Edition), 2022, 16( 2): 108- 114. DOI: 10.3877/cma.j.issn.1674-1358.2022.02.005.高祥, 赵成军, 胡世宏. 年龄-胆红素-国际标准化比率-肌酐评分对乙型肝炎相关慢加急性肝功能衰竭患者短期预后的评估价值[J/CD]. 中华实验和临床感染病杂志(电子版), 2022, 16( 2): 108- 114. DOI: 10.3877/cma.j.issn.1674-1358.2022.02.005. [25] PIERRAKOS C, VELISSARIS D, FELLEITER P, et al. Increased mortality in critically ill patients with mild or moderate hyperbilirubinemia[J]. J Crit Care, 2017, 40: 31- 35. DOI: 10.1016/j.jcrc.2017.01.017. [26] LAI M, WANG X, YAO QW, et al. Predictive value of the initial MELD score and its derivative scores for early survival rate after liver transplantation in patients with liver failure[J]. Ogran Transplant, 2022, 13( 4): 489- 494. DOI: 10.3969/j.issn.1674-7445.2022.04.012.赖曼, 王鑫, 姚勤伟, 等. 术后首次MELD评分及其衍生评分对肝衰竭患者肝移植术后早期生存率的预测价值[J]. 器官移植, 2022, 13( 4): 489- 494. DOI: 10.3969/j.issn.1674-7445.2022.04.012. -



 PDF下载 ( 920 KB)
PDF下载 ( 920 KB)

 下载:
下载: