ZJU指数对新疆维吾尔自治区农村地区维吾尔族人群非酒精性脂肪性肝病发生风险的预测价值
DOI: 10.3969/j.issn.1001-5256.2023.11.012
ZJU index and the risk of nonalcoholic fatty liver disease in the Uygur population in the rural area of Xinjiang Uygur Autonomous Region: A cohort study
-
摘要:
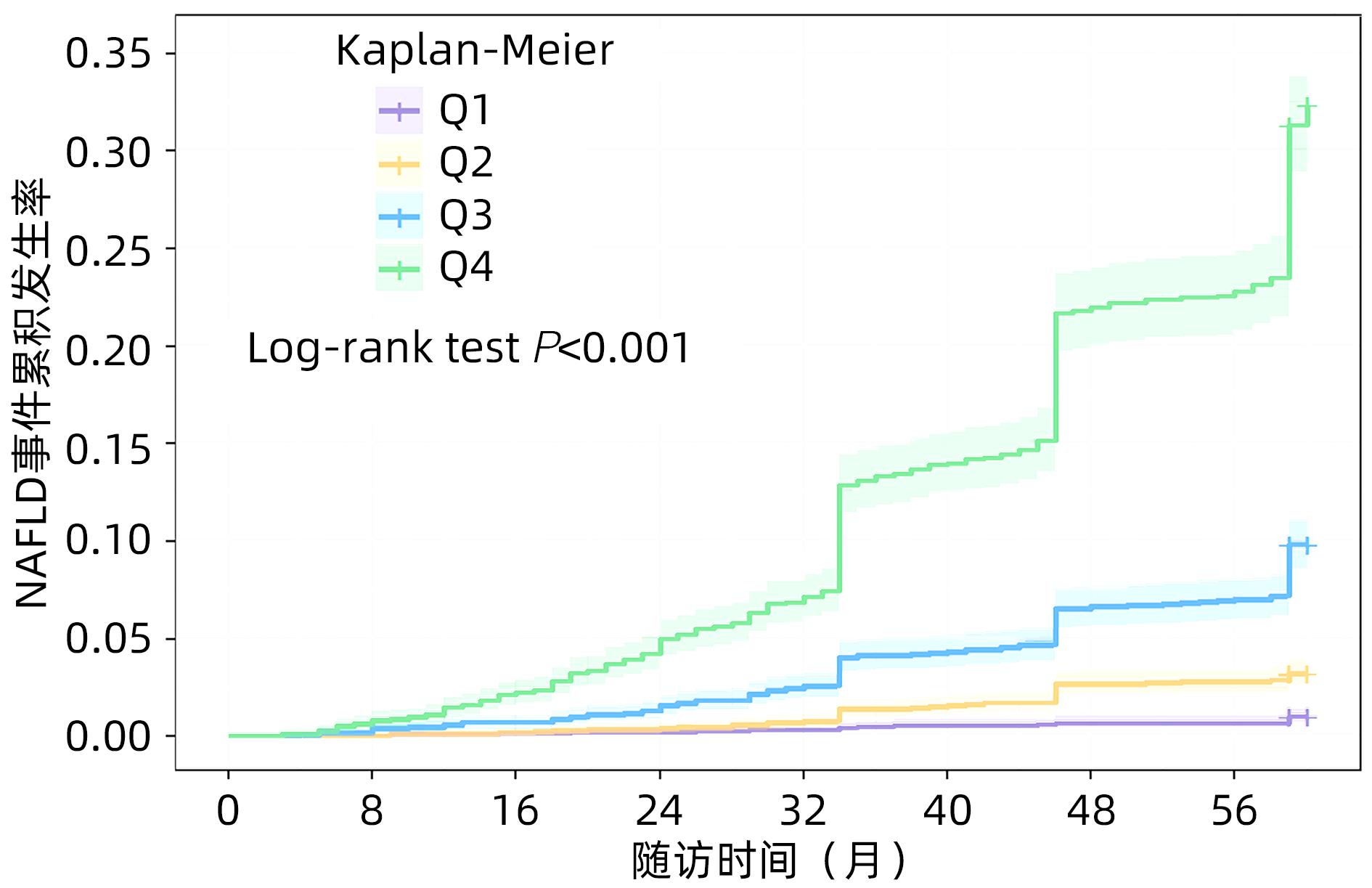
目的 探讨ZJU指数与维吾尔族NAFLD发病的关联性及其对NAFLD发生风险的预测价值。 方法 选择新疆喀什地区兵团第三师51团维吾尔族聚集区为调查现场,研究对象为在当地居住且年龄>18岁的维吾尔族居民。分别在2019、2020和2021年进行随访,2021年6月—8月完成结局调查;最终共纳入研究对象10 597名。连续变量组间比较采用Kruskal-Wallis H检验;分类变量采用χ²检验。根据ZJU指数水平将研究对象分为4组(Q1~Q4组),采用Kaplan-Meier曲线计算NAFLD事件的发生率,采用Cox回归模型分析ZJU指数与NAFLD发病风险的关联;采用受试者工作特征曲线下面积(AUC)评估ZJU指数对NAFLD发生风险的预测价值。 结果 在4.92年的中位随访期间,研究人群NAFLD发病率为9.4%(992/10 597)。经多因素调整后,随着ZJU指数的升高,NAFLD发生风险HR(95%CI)值分别为2.55(1.60~4.06)、7.32(4.78~11.20)、21.74(14.32~33.00),呈明显上升趋势(P趋势值<0.001)。ROC曲线结果显示,ZJU指数预测NAFLD效果更好(AUC=0.816),男性亚组ZJU指数AUC(0.829)高于女性AUC(0.809)。 结论 ZJU指数是新疆维吾尔自治区农村地区维吾尔族NAFLD发生的预测因子,对NAFLD发病风险具有良好的预测价值。 Abstract:Objective To investigate the association between ZJU index and the onset of nonalcoholic fatty liver disease (NAFLD) in the Uygur population and the value of ZJU index in predicting the risk of NAFLD. Methods The Uighur community of The 51st Regiment of The Third Division of Xinjiang Kashgar Corps was selected as the investigation site, and the Uygur residents who lived in this area and had an age of >18 years were selected as subjects. Follow-up studies were conducted in 2019, 2020, and 2021, and the investigation of outcomes was completed in June to August of 2021. Finally 10 597 subjects were enrolled for analysis. The Kruskal-Wallis H test was used for comparison of continuous variables between groups, and the chi-square test was used for comparison of categorical variables between groups. The subjects were divided into Q1-Q4 groups according to the level of ZJU index. The Kaplan-Meier curve was used to predict the incidence rate of NAFLD, and the Cox regression model was used to analyze the association between ZJU index and the risk of NAFLD; the area under the ROC curve (AUC) was used to evaluate the value of ZJU index in predicting the risk of NAFLD. Results During the median follow-up time of 4.92 years, the incidence rate of NAFLD was 9.4% (992/10 597) among the study population. After adjustment for multiple factors, there was a significant increase in the risk of NAFLD with the increase in ZJU index, with a hazard ratio of 2.55 (95% confidence interval [CI]: 1.60 — 4.06), 7.32 (95%CI: 4.78 — 11.20), and 21.74 (95%CI: 14.32 — 33.00), respectively (all Ptrend<0.001). The ROC curve showed that ZJU index had a higher value in predicting NAFLD (AUC=0.816), and the male subgroup had a significantly higher predictive accuracy of ZJU index than the female subgroup (AUC: 0.829 vs 0.809). Conclusion ZJU index is a predictive factor for the onset of NAFLD in the Uygur population in rural areas of Xinjiang and has a good value in predicting the risk of NAFLD. -
Key words:
- Non-alcoholic Fatty Liver Disease /
- Forecasting /
- Xinjiang
-
表 1 新疆维吾尔族ZJU指数四分位数分组人群基线特征的比较
Table 1. Comparison of baseline characteristics of Xinjiang Uyghur ZJU index quartile group population
特征 总例数(n=10 597) Q1组(n=2 649) Q2组(n=2 649) Q3组(n=2 650) Q4组(n=2 649) 统计值 P值 年龄(岁) 35.71±13.03 28.65±10.69 34.44±12.17 38.60±12.56 42.82±12.41 H=2 103.149 <0.001 性别[例(%)] χ²=498.814 <0.001 男 5 285(49.9) 1 691(63.8) 1 437(52.8) 1 255(47.4) 902(34.1) 女 5 312(50.1) 958(36.2) 1 212(45.8) 1 395(52.6) 1 747(65.9) 收缩压(mmHg) 127.02±18.23 120.90±14.74 124.36±16.39 128.93±18.49 135.63±20.14 H=826.487 <0.001 舒张压(mmHg) 75.01±11.70 71.89±10.17 73.43±11.15 75.91±11.43 79.73±12.70 H=624.455 <0.001 血糖(mmol/L) 4.92±1.71 4.43±0.83 4.71±0.89 4.85±0.99 5.85±3.01 H=767.086 <0.001 BMI(kg/m2) 25.49±4.55 20.94±1.94 24.01±1.90 26.90±2.13 31.35±3.83 H=7 850.767 <0.001 AST(U/L) 27.36±15.67 26.91±14.74 26.60±14.34 28.02±16.46 28.10±17.27 H=10.597 0.060 ALT(U/L) 24.13±9.40 22.47±8.70 23.76±8.01 24.60±8.81 26.08±11.67 H=120.604 <0.001 GGT(U/L) 17.33±12.82 14.80±9.96 15.91±11.20 18.35±13.84 21.02±15.39 H=392.526 <0.001 TG(mmol/L) 1.64±1.25 1.12±0.60 1.40±0.79 1.76±1.08 2.45±1.88 H=1 791.191 <0.001 TC(mmol/L) 4.65±1.42 4.25±1.34 4.62±1.45 4.81±1.31 5.02±1.47 H=756.864 <0.001 LDL-C(mmol/L) 2.62±0.71 2.54±0.63 2.57±0.69 2.67±0.74 2.74±0.78 H=115.495 <0.001 HDL-C(mmol/L) 1.66±0.58 1.71±0.52 1.67±0.58 1.63±0.58 1.61±0.64 H=120.755 <0.001 T2DM[例(%)] 525(5.0) 11(0.4) 47(1.8) 87(3.3) 380(14.3) χ²=684.618 <0.001 吸烟[例(%)] 1 834(17.3) 708(26.7) 487(18.4) 402(15.2) 237(8.9) χ²=304.225 <0.001 高血压[例(%)] 2 573(24.3) 332(12.5) 498(18.8) 679(25.6) 1 064(40.2) χ²=675.667 <0.001 NAFLD[例(%)] 992(9.4) 24(0.9) 70(2.6) 220(8.3) 678(25.6) χ²=1 190.359 <0.001 注:按基线ZJU指数水平分为4组(Q1~Q4组),Q1组(≤32.05),Q2组(32.05~35.33),Q3组(35.33~39.28)和Q4组(≥39.28)。 表 2 研究人群不同年龄段NAFLD发病率
Table 2. The incidence of NAFLD in different age groups
不同年龄段 男性 女性 总例数 例数 NAFLD[例(%)] 例数 NAFLD[例(%)] 例数 NAFLD[例(%)] <35岁 2 983 109(3.7 ) 2 917 112(3.8) 5 900 221(3.7) 35~44岁 1 330 169(12.7) 1 244 194(15.6) 2 574 363(14.1) >44岁 972 179(18.4) 1 151 229(19.9) 2 123 408(19.2) χ2趋势值 239.331 289.636 530.567 P趋势值 <0.001 <0.001 <0.001 表 3 新疆维吾尔族ZJU指数与NAFLD发生风险的关联
Table 3. Association of ZJU index with the risk of NAFLD occurrence in Xinjiang Uyghur people
ZJU指数 模型1 模型2 模型3 HR(95%CI) P值 HR(95%CI) P值 HR(95%CI) P值 Q1组 1 1 1 Q2组 2.94(1.85~4.68) <0.001 2.66(1.67~4.24) <0.001 2.55(1.60~4.06) <0.001 Q3组 9.47(6.21~14.43) <0.001 7.98(5.22~12.20) <0.001 7.32(4.78~11.20) <0.001 Q4组 31.73(21.12~47.67) <0.001 25.35(16.75~38.38) <0.001 21.74(14.32~33.00) <0.001 P趋势值 <0.001 <0.001 <0.001 注:模型1无调整;模型2调整性别、年龄;模型3在模型2基础上进一步调整高血压、吸烟、GGT、HDL-C、LDL-C、TC。 表 4 新疆维吾尔族TyG、LAP、HSI、VAI、ZJU指数对NAFLD发病的预测价值
Table 4. Predictive value of TyG, LAP, HSI, VAI, and ZJU indices for the development of NAFLD in Xinjiang Uyghur people
变量 截断值 敏感度 特异度 约登指数 AUC(95%CI) P值 TyG 2.263 0.494 0.792 0.286 0.689(0.671~0.706) <0.001 LAP 43.830 0.775 0.631 0.406 0.768(0.754~0.783) <0.001 WHtR 0.571 0.804 0.650 0.454 0.786(0.772~0.800) <0.001 HSI 35.854 0.702 0.660 0.362 0.733(0.718~0.749) <0.001 VAI 75.585 0.749 0.603 0.352 0.733(0.718~0.749) <0.001 ZJU 37.808 0.786 0.717 0.503 0.816(0.804~0.829) <0.001 表 5 TyG、LAP、WHtR、HSI、VAI、ZJU指数对NAFLD预测准确性的性别差异
Table 5. Gender differences in diagnostic accuracy of TyG, LAP, WHtR, HSI, VAI, and ZJU indices for NAFLD
变量 男性 女性 AUC(95%CI) P值 AUC(95%CI) P值 TyG 0.734(0.710~0.758) <0.001 0.659(0.636~0.683) <0.001 LAP 0.802(0.782~0.822) <0.001 0.737(0.717~0.758) <0.001 WHtR 0.806(0.787~0.824) <0.001 0.772(0.751~0.792) <0.001 HSI 0.730(0.706~0.754) <0.001 0.748(0.727~0.769) <0.001 VAI 0.761(0.738~0.783) <0.001 0.702(0.681~0.724) <0.001 ZJU 0.829(0.811~0.848) <0.001 0.809(0.792~0.826) <0.001 -
[1] PAIK JM, GOLABI P, YOUNOSSI Y, et al. Changes in the global burden of chronic liver diseases from 2012 to 2017: The growing impact of NAFLD[J]. Hepatology, 2020, 72( 5): 1605- 1616. DOI: 10.1002/hep.31173. [2] IOANNOU GN. Epidemiology and risk-stratification of NAFLD-associated HCC[J]. J Hepatol, 2021, 75( 6): 1476- 1484. DOI: 10.1016/j.jhep.2021.08.012. [3] YAN SY, FAN JG. Diagnosis and treatment of hepatocellular carcinoma associated with nonalcoholic fatty liver disease[J]. J Clin Hepatol, 2021, 37( 8): 1748- 1752. DOI: 10.3969/j.issn.1001-5256.2021.08.002.颜士岩, 范建高. 非酒精性脂肪性肝病相关肝细胞癌的诊断和治疗[J]. 临床肝胆病杂志, 2021, 37( 8): 1748- 1752. DOI: 10.3969/j.issn.1001-5256.2021.08.002. [4] ZHOU F, ZHOU JH, WANG WX, et al. Unexpected rapid increase in the burden of NAFLD in China from 2008 to 2018: A systematic review and meta-analysis[J]. Hepatology, 2019, 70( 4): 1119- 1133. DOI: 10.1002/hep.30702. [5] HOU D, SUN Y, ZHANG XR, et al. Analysis of disease spectrum of annual physical examination in Grade A tertiary hospital[J]. Trauma Crit Care Med, 2022, 10( 6): 435- 437. DOI: 10.16048/j.issn.2095-5561.2022.06.12.侯丹, 孙月, 张晓茹, 等. 某三甲医院年度健康体检疾病谱分析[J]. 创伤与急危重病医学, 2022, 10( 6): 435- 437. DOI: 10.16048/j.issn.2095-5561.2022.06.12. [6] WANG CE, XU WT, GONG J, et al. Advances in the treatment of nonalcoholic fatty liver disease[J]. Clin J Med Offic, 2022, 50( 9): 897- 899, 903. DOI: 10.16680/j.1671-3826.2022.09.06.王彩娥, 许文涛, 宫建, 等. 非酒精性脂肪性肝病治疗研究进展[J]. 临床军医杂志, 2022, 50( 9): 897- 899, 903. DOI: 10.16680/j.1671-3826.2022.09.06. [7] LI TX, ZHU JZ, ZHANG Y, et al. Validation of the ZJU index for nonalcoholic fatty liver disease in West China: A cross-sectional study[J]. Int J Clin Exp Med, 2016, 9( 9): 18395- 18399. [8] LI L, YOU W, REN W. The ZJU index is a powerful index for identifying NAFLD in the general Chinese population[J]. Acta Diabetol, 2017, 54( 10): 905- 911. DOI: 10.1007/s00592-017-1024-8. [9] WANG JH, XU CF, XUN YH, et al. ZJU index: A novel model for predicting nonalcoholic fatty liver disease in a Chinese population[J]. Sci Rep, 2015, 5: 16494. DOI: 10.1038/srep16494. [10] FU CP, ALI H, RACHAKONDA VP, et al. The ZJU index is a powerful surrogate marker for NAFLD in severely obese North American women[J]. PLoS One, 2019, 14( 11): e0224942. DOI: 10.1371/journal.pone.0224942. [11] SONG JM, XIAN YJ, MOHEDESI SYT, et al. Prevalence of and risk factors for nonalcoholic fatty liver disease in community residents in Urumqi city[J]. World Chin J Dig, 2016, 24( 12): 1880- 1884.宋江美, 咸亚静, 莫合德斯·斯依提, 等. 乌鲁木齐市社区居民非酒精性脂肪肝流行现状调查[J]. 世界华人消化杂志, 2016, 24( 12): 1880- 1884. [12] National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, Chinese Medical Association, Fatty Liver Expert Committee, Chinese Medical Doctor Association. Guidelines of prevention and treatment for nonalcoholic fatty liver disease: A 2018 update[J]. J Clin Hepatol, 2018, 34( 5): 947- 957. DOI: 10.3969/j.issn.1001-5256.2018.05.007.中华医学会肝病学分会脂肪肝和酒精性肝病学组, 中国医师协会脂肪性肝病专家委员会. 非酒精性脂肪性肝病防治指南(2018年更新版)[J]. 临床肝胆病杂志, 2018, 34( 5): 947- 957. DOI: 10.3969/j.issn.1001-5256.2018.05.007. [13] FARRELL GC, CHITTURI S, LAU GKK, et al. Guidelines for the assessment and management of non-alcoholic fatty liver disease in the Asia-Pacific region: Executive summary[J]. J Gastroenterol Hepatol, 2007, 22( 6): 775- 777. DOI: 10.1111/j.1440-1746.2007.05002.x. [14] Writing Group of 2018 Chinese Guidelines for the Management of Hypertension, Chinese Hypertension League, Chinese Society of Cardiology, et al. 2018 Chinese guidelines for the management of hypertensionWriting Group of 2018[J]. Chin J Cardiovasc Med, 2019, 24( 1): 24- 56. DOI: 10.3969/j.issn.1007-5410.2019.01.002.中国高血压防治指南修订委员会, 高血压联盟(中国), 中华医学会心血管病学分会, 等. 中国高血压防治指南(2018年修订版)[J]. 中国心血管杂志, 2019, 24( 1): 24- 56. DOI: 10.3969/j.issn.1007-5410.2019.01.002. [15] FENG BY, CHEN JC, LI Y, et al. Relationship between overweight/obesity and hypertension among adults in China: A prospective study[J]. Chin J Epidemiol, 2016, 37( 5): 606- 611.冯宝玉, 陈纪春, 李莹, 等. 中国成年人超重和肥胖与高血压发病关系的随访研究[J]. 中华流行病学杂志, 2016, 37( 5): 606- 611. [16] SHENG GT, LU S, XIE QY, et al. The usefulness of obesity and lipid-related indices to predict the presence of non-alcoholic fatty liver disease[J]. Lipids Health Dis, 2021, 20( 1): 134. DOI: 10.1186/s12944-021-01561-2. [17] AMATO MC, GIORDANO C, GALIA M, et al. Visceral Adiposity Index: A reliable indicator of visceral fat function associated with cardiometabolic risk[J]. Diabetes Care, 2010, 33( 4): 920- 922. DOI: 10.2337/dc09-1825. [18] GUERRERO-ROMERO F, SIMENTAL-MENDÍA LE, GONZÁLEZ-ORTIZ M, et al. The product of triglycerides and glucose, a simple measure of insulin sensitivity. Comparison with the euglycemic-hyperinsulinemic clamp[J]. J Clin Endocrinol Metab, 2010, 95( 7): 3347- 3351. DOI: 10.1210/jc.2010-0288. [19] LEE JH, KIM D, KIM HJ, et al. Hepatic steatosis index: A simple screening tool reflecting nonalcoholic fatty liver disease[J]. Dig Liver Dis, 2010, 42( 7): 503- 508. DOI: 10.1016/j.dld.2009.08.002. [20] LU ZY, SHAO Z, LI YL, et al. Prevalence of and risk factors for non-alcoholic fatty liver disease in a Chinese population: An 8-year follow-up study[J]. World J Gastroenterol, 2016, 22( 13): 3663- 3669. DOI: 10.3748/wjg.v22.i13.3663. [21] ZHOU YJ, LI YY, NIE YQ, et al. Natural course of nonalcoholic fatty liver disease in Southern China: A prospective cohort study[J]. J Dig Dis, 2012, 13( 3): 153- 160. DOI: 10.1111/j.1751-2980.2011.00571.x. [22] CAI W, YANG L, NIE YW, et al. Construction and analysis of NAFLD cohort risk assessment model for male and females in Urumqi City[J]. Chongqing Med, 2021, 50( 23): 4028- 4032. DOI: 10.3969/j.issn.1671-8348.2021.23.015.蔡雯, 杨磊, 聂艳武, 等. 乌鲁木齐市男、女性NAFLD队列风险评估模型构建与分析[J]. 重庆医学, 2021, 50( 23): 4028- 4032. DOI: 10.3969/j.issn.1671-8348.2021.23.015. [23] FANG JM. Study on the predictive value of the influencing factors and risk indexes of fatty liver[D]. Jinzhou: Jinzhou Medical University, 2021.方建梅. 脂肪肝影响因素及风险指标对其预测价值研究[D]. 锦州: 锦州医科大学, 2021. [24] HU W, LIU ZY, HAO HR, et al. Correlation between income and non-alcoholic fatty liver disease in a Chinese population[J]. Ann Endocrinol, 2020, 81( 6): 561- 566. DOI: 10.1016/j.ando.2020.07.1109. [25] XU CN, MA ZM, WANG YF, et al. Visceral adiposity index as a predictor of NAFLD: A prospective study with 4-year follow-up[J]. Liver Int, 2018, 38( 12): 2294- 2300. DOI: 10.1111/liv.13941. [26] LIU YX, LIU SY, HUANG JF, et al. Validation of five hepatic steatosis algorithms in metabolic-associated fatty liver disease: A population based study[J]. J Gastroenterol Hepatol, 2022, 37( 5): 938- 945. DOI: 10.1111/jgh.15799. [27] OKADA A, YAMADA G, KIMURA T, et al. Diagnostic ability using fatty liver and metabolic markers for metabolic-associated fatty liver disease stratified by metabolic/glycemic abnormalities[J]. J Diabetes Investig, 2023, 14( 3): 463- 478. DOI: 10.1111/jdi.13966. [28] CAI JW, LIN CT, LAI SQ, et al. Waist-to-height ratio, an optimal anthropometric indicator for metabolic dysfunction associated fatty liver disease in the Western Chinese male population[J]. Lipids Health Dis, 2021, 20( 1): 145. DOI: 10.1186/s12944-021-01568-9. [29] LEE SB, KIM MK, KANG S, et al. Triglyceride glucose index is superior to the homeostasis model assessment of insulin resistance for predicting nonalcoholic fatty liver disease in Korean adults[J]. Endocrinol Metab, 2019, 34( 2): 179- 186. DOI: 10.3803/EnM.2019.34.2.179. [30] JI BL, QU H, WANG H, et al. The ZJU index: A useful indicator for recognizing insulin resistance in the Chinese general population[J]. Acta Diabetol, 2016, 53( 5): 817- 823. DOI: 10.1007/s00592-016-0878-5. [31] FOSCHI FG, CONTI F, DOMENICALI M, et al. External validation of surrogate indices of fatty liver in the general population: The bagnacavallo study[J]. J Clin Med, 2021, 10( 3): 520. DOI: 10.3390/jcm10030520. [32] LI X, QIN P, CAO LM, et al. Dose-response association of the ZJU index and fatty liver disease risk: A large cohort in China[J]. J Gastroenterol Hepatol, 2021, 36( 5): 1326- 1333. DOI: 10.1111/jgh.15286. [33] GAGGINI M, MORELLI M, BUZZIGOLI E, et al. Non-alcoholic fatty liver disease(NAFLD) and its connection with insulin resistance, dyslipidemia, atherosclerosis and coronary heart disease[J]. Nutrients, 2013, 5( 5): 1544- 1560. DOI: 10.3390/nu5051544. [34] PUTRI RR, CASSWALL T, HAGMAN E. Prevalence of increased transaminases and its association with sex, age, and metabolic parameters in children and adolescents with obesity-a nationwide cross-sectional cohort study[J]. BMC Pediatr, 2021, 21( 1): 271. DOI: 10.1186/s12887-021-02747-4. [35] YANG MY, WU QZ, WANG SH, et al. Incidence of fatty liver and its effect on liver function and blood lipid in women of childbearing age[J]. Clin J Med Offic, 2022, 50( 9): 985- 987. DOI: 10.16680/j.1671-3826.2022.09.33.杨沐怿, 武巧珍, 王素花, 等. 育龄期体检女性脂肪肝发生情况及其对肝功能与血脂影响[J]. 临床军医杂志, 2022, 50( 9): 985- 987. DOI: 10.16680/j.1671-3826.2022.09.33. [36] KWON YM, OH SW, HWANG SS, et al. Association of nonalcoholic fatty liver disease with components of metabolic syndrome according to body mass index in Korean adults[J]. Am J Gastroenterol, 2012, 107( 12): 1852- 1858. DOI: 10.1038/ajg.2012.314. [37] LIU M, WANG JH, ZENG J, et al. Association of NAFLD with diabetes and the impact of BMI changes: A 5-year cohort study based on 18, 507 elderly[J]. J Clin Endocrinol Metab, 2017, 102( 4): 1309- 1316. DOI: 10.1210/jc.2016-3440. [38] ZHANG LX, ZHANG MT, WANG M, et al. External validation and comparison of simple tools to screen for nonalcoholic fatty liver disease in Chinese community population[J]. Eur J Gastroenterol Hepatol, 2022, 34( 8): 865- 872. DOI: 10.1097/MEG.0000000000002399. -



 PDF下载 ( 795 KB)
PDF下载 ( 795 KB)

 下载:
下载:


