血清补体C3对原发性胆汁性胆管炎相关肝纤维化分期的诊断价值
DOI: 10.3969/j.issn.1001-5256.2023.11.013
Value of serum complement C3 in the diagnosis of liver fibrosis associated with primary biliary cholangitis
-
摘要:
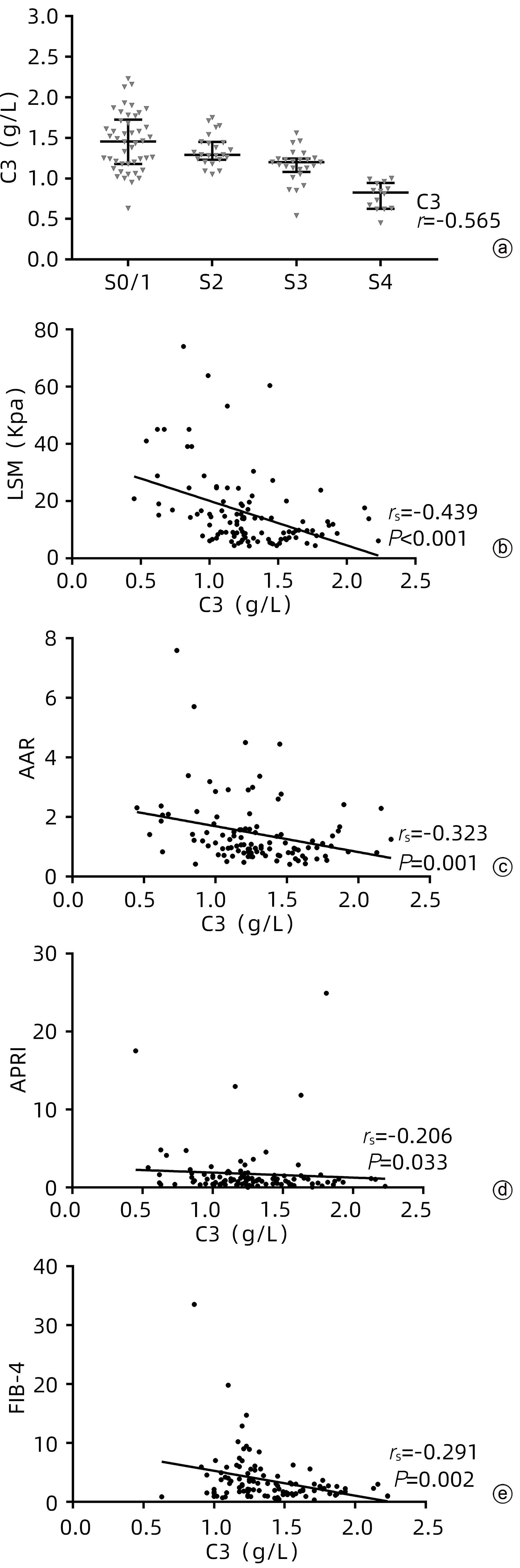
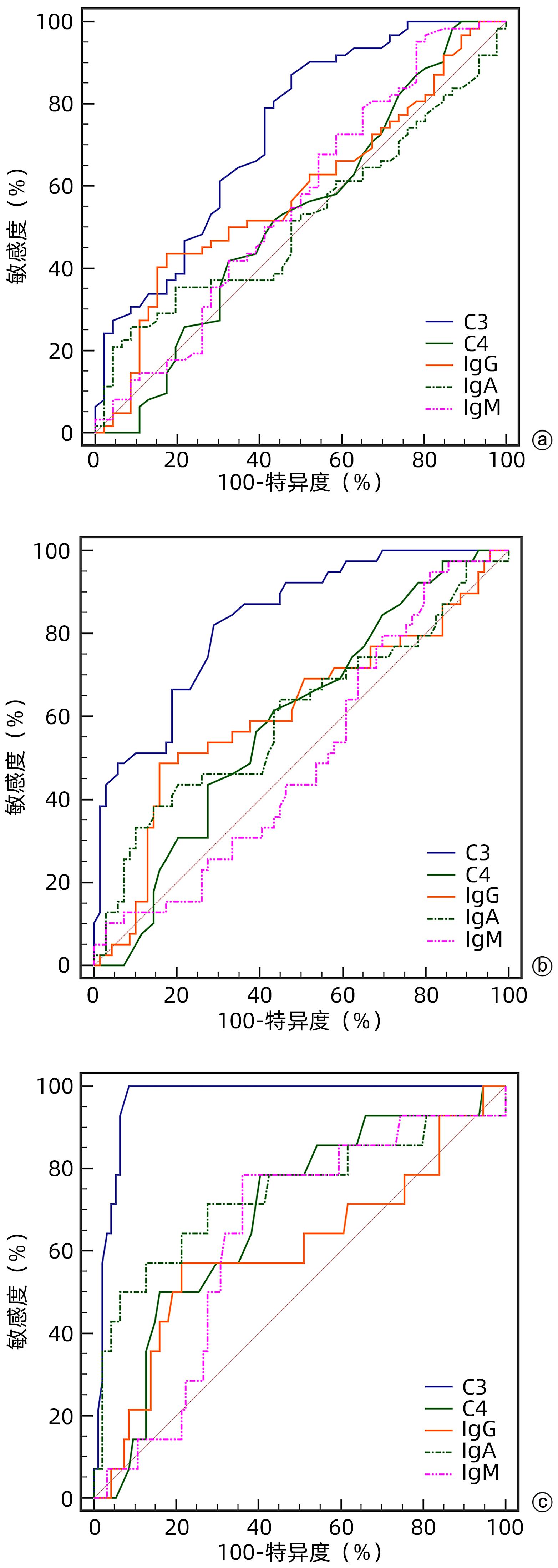
目的 探讨血清补体C3水平对原发性胆汁性胆管炎(PBC)肝纤维化分期的诊断价值。 方法 收集2012年1月—2022年10月在天津市第二人民医院就诊并行肝穿刺活检的108例PBC患者临床资料。依据Scheuer评分系统评估肝纤维化程度(S0~4),其中≥S2定义为显著肝纤维化,≥S3定义为进展期肝纤维化,S4定义为肝硬化。符合正态分布的计量资料两组间比较采用独立样本t检验,多组间比较采用单因素方差分析。不符合正态分布的计量资料两组间比较采用Mann-Whitney U检验,多组间比较采用Kruskal-Wallis H秩和检验。计数资料组间比较采用χ2检验或Fisher精确检验。通过受试者工作特征曲线下面积(AUC)评估补体C3对PBC患者肝纤维化的诊断效能。采用Spearman相关分析评估补体C3与肝纤维化分期的相关性。 结果 本研究108例PBC患者中女性87例(80.6%),自身抗体阳性102例(94.4%)。肝纤维化分期S0期5例(4.6%),S1期41例(38.0%),S2期23例(21.3%),S3期25例(23.1%)、S4期14例(13.0%)。补体C3在不同肝纤维化分期患者中具有统计学差异(H=42.891,P<0.001)。随着肝纤维化程度的加重,补体C3的水平逐渐降低,呈负相关(r=-0.565,P<0.001)。LSM、AAR、APRI及FIB-4与补体C3的相关系数分别为-0.439(P<0.001)、-0.323(P=0.001)、-0.206(P=0.033)和-0.291(P=0.002)。多因素Logistic回归显示补体C3水平均为显著肝纤维化、进展期肝纤维化和肝硬化的独立预测因素,而LSM是显著肝纤维化和进展期肝纤维化的独立预测因素。ROC曲线分析显示,补体C3诊断显著肝纤维化、进展期肝纤维化及肝硬化的AUC分别为0.731、0.832和0.968,对应的cut-off值分别为1.445、1.235和1.005;补体C3联合LSM诊断显著肝纤维化、进展期肝纤维化及肝硬化的AUC分别为0.811、0.941和0.976。C3联合LSM诊断显著纤维化的AUC与补体C3的相比,差异具有统计学意义(Z=2.604,P=0.009);C3联合LSM诊断进展期肝纤维化的AUC与补体C3的相比,差异具有统计学意义(Z=3.033,P=0.002);C3联合LSM诊断肝硬化的AUC与补体C3的相比,差异不具有统计学意义(Z=1.050,P=0.294),而C3联合LSM诊断肝硬化的AUC与LSM的相比,差异具有统计学意义(Z=2.326,P=0.020)。 结论 血清补体C3水平对评估PBC患者肝纤维化程度有一定的临床价值,C3联合LSM能进一步提高补体C3或LSM对PBC肝纤维化的诊断效能。 Abstract:Objective To investigate the value of serum complement C3 level in determining the stage of liver fibrosis in primary biliary cholangitis (PBC). Methods Clinical data were collected from 108 patients with PBC who attended Tianjin Second People’s Hospital and underwent liver biopsy from January 2012 to October 2022. The degree of liver fibrosis (S0-4) was assessed according to the Scheuer scoring system, with ≥S2 defined as significant liver fibrosis, ≥S3 defined as progressive liver fibrosis, and S4 defined as liver cirrhosis. The independent samples t-test was used for comparison of normally distributed continuous data between two groups, and a one-way analysis of variance was used for comparison between multiple groups; the Mann-Whitney U test was used for comparison of non-normally distributed continuous data between two groups, and the Kruskal-Wallis H test was used for comparison between multiple groups; the chi-square test or the Fisher’s exact test was used for comparison of categorical data between groups. The area under the ROC curve (AUC) was used to evaluate the efficacy of complement C3 in the diagnosis of liver fibrosis in patients with PBC. The Spearman correlation analysis was used to investigate the correlation between complement C3 and liver fibrosis stage. Results Among the 108 patients with PBC, there were 87 (80.6%) female patients and 102 patients (94.4%) with positive autoantibody. As for the stage of liver fibrosis, there were 5 patients (4.6%) in S0 stage, 41 (38.0%) in S1 stage, 23 (21.3%) in S2 stage, 25 (23.1%) in S3 stage, and 14 (13.0%) in S4 stage. There was a significant difference in the level of complement C3 between the patients with different liver fibrosis stages (H=42.891, P<0.001). The level of complement C3 gradually decreased with the aggravation of liver fibrosis, with a negative correlation between them (r=-0.565, P<0.001). Liver stiffness measurement (LSM), aspartate aminotransferase/alanine aminotransferase ratio, aspartate aminotransferase-to-platelet ratio index, and fibrosis-4 were negatively correlated with complement C3, with a correlation coefficient of -0.439 (P<0.001), -0.323 (P=0.001), -0.206 (P=0.033), and -0.291 (P=0.002), respectively. The multivariate logistic regression analysis showed that complement C3 level was an independent predictive factor for significant liver fibrosis, progressive liver fibrosis, and liver cirrhosis, while LSM was an independent predictive factor for significant liver fibrosis and progressive liver fibrosis. The ROC curve analysis showed that complement C3 had an AUC of 0.731, 0.832, and 0.968, respectively, in the diagnosis of significant liver fibrosis, progressive liver fibrosis, and liver cirrhosis, with a corresponding cut-off value of 1.445, 1.235, and 1.005, respectively, and complement C3 combined with LSM had an AUC of 0.811, 0.941, and 0.976, respectively, in the diagnosis of significant liver fibrosis, progressive liver fibrosis, and liver cirrhosis. There was a significant difference in AUC between complement C3 combined with LSM and complement C3 alone in the diagnosis of significant liver fibrosis (Z=2.604, P=0.009), and there was also a significant difference in AUC between complement C3 combined with LSM and complement C3 alone in the diagnosis of progressive liver fibrosis (Z=3.033, P=0.002); there was no significant difference in AUC between complement C3 combined with LSM and complement C3 alone in the diagnosis of liver cirrhosis (Z=1.050, P=0.294), while There was a significant difference in AUC between complement C3 combined with LSM and LSM alone in the diagnosis of liver cirrhosis (Z=2.326, P=0.020). Conclusion Serum complement C3 level has a certain clinical value in assessing the degree of liver fibrosis in patients with PBC, and complement C3 combined with LSM can further improve the efficacy of complement C3 or LSM in the diagnosis of liver fibrosis in PBC. -
Key words:
- Cholangitis, Sclerosing /
- Hepatic Fibrosis /
- Complement C3
-
表 1 PBC患者的一般特征
Table 1. General characteristics of PBC patients
指标 数值(n=108) 指标 数值(n=108) 人口学数据 ALT(U/L) 47.0(23.5~100.1) 年龄(岁) 53.6±10.4 AST(U/L) 57.0(34.0~90.8) 男[例(%)] 21(19.4) GGT(U/L) 207.4(113.0~460.3) 女[例(%)] 87(80.6) ALP(U/L) 219.9(124.5~414.0) BMI (kg/m2) 22.3(20.3~24.7) CHE(U/L) 6187.0±2154.3 吸烟史[例(%)] 16(14.8) Alb(g/L) 38.7±6.1 饮酒史[例(%)] 10(9.3) TBil(μmol/L) 19.3(12.5~31.5) 糖尿病[例(%)] 13(12.0) DBil(μmol/L) 6.8(3.3~15.4) 高血压[例(%)] 25(23.1) IBil(μmol/L) 11.4(7.7~15.4) 临床表现[例(%)] 免疫功能指标(g/L) 乏力 42(38.9) C3 1.2(1.1~1.5) 纳差 12(11.1) C4 0.2±0.1 瘙痒 10(9.3) IgG 17.5±5.8 尿黄 16(14.8) IgA 3.1(2.1~3.7) 腹胀 12(11.1) IgM 2.8(1.8~4.8) 肝区不适 16(14.8) 纤维化指标及评分 其他1) 16(14.8) LSM(kPa) 11.7(7.2~18.9) 自身抗体指标[例(%)] AAR(分) 1.1(0.8~1.6) 自身抗体阳性 102(94.4) APRI(分) 0.9(0.4~1.5) ANA阳性 100(92.6) FIB-4(分) 2.3(1.4~4.3) AMA阳性 58(53.7) 肝纤维化分期[例(%)] 抗M2阳性 54(50.0) S0 5(4.6) 抗Sp100阳性 10(9.3) S1 41(38.0) 抗Gp210阳性 24(22.2) S2 23(21.3) 血清学指标 S3 25(23.1) PLT(×109/L) 197.0(120.3~258.3) S4 14(13.0) 注:1)其他包括黄疸、厌油、口干、眼干、关节痛。 表 2 PBC患者肝纤维化分期的一般特征
Table 2. General characteristics of hepatic fibrosis stage in patients with PBC
指标 S0/1(n=46) S2(n=23) S3(n=25) S4(n=14) 统计值 P值 年龄(岁) 53.0±9.7 54.5±8.9 53.2±13.7 54.8±9.2 F=0.173 0.914 性别[例(%)] χ2=0.365 0.985 男 9(19.6) 5(21.7) 5(20.0) 2(14.3) 女 37(80.4) 18(78.3) 20(80.0) 12(85.7) 自身抗体阳性[例(%)] 43(93.5) 22(95.7) 23(92.0) 12(85.7) χ2=1.992 0.641 BMI(kg/m2) 22.2(20.3~24.9) 22.6(20.1~25.0) 22.9(21.3~24.4) 22.7(19.4~24.5) H=0.253 0.969 PLT(×109/L) 230.5(186.3~264.5) 209.0(134.0~253.0) 166.0(95.5~244.5) 87.0(57.8~172.3)1) H=16.880 0.001 ALT(U/L) 49.0(27.7~90.0) 53.0(27.1~118.4) 37.5(18.3~131.8) 28.5(15.2~61.1) H=4.002 0.261 AST(U/L) 58.0(34.3~83.5) 51.2(33.0~65.8) 62.4(35.0~109.5) 80.1(41.8~116) H=2.704 0.440 GGT(U/L) 237.0(118.0~541.0) 198.0(142.0~650.0) 207.4(116.5~369.6) 190.0(86.0~339.0) H=1.368 0.713 ALP(U/L) 278.0(128.6~423.0) 203.0(122.0~414.0) 215.8(118.4~367.0) 236.1(143.5~371.8) H=0.345 0.951 CHE(U/L) 6 711.9±2 124.6 7 044.6±2 037.5 5 869.9±1 663.3 3 906.91±1 526.61)2)3) F=9.124 <0.001 Alb(g/L) 39.9±5.6 40.6±5.0 39.4±5.3 30.9±5.21)2)3) F=11.873 <0.001 TBil(μmol/L) 17.1(13.3~31.5) 13.1(11.2~20.4) 22.7(16.2~30.7) 28.3(17.9~56.7) H=8.092 0.044 DBil(μmol/L) 7.3(2.9~15.9) 4.1(3.2~6.6) 7.7(3.4~13.1) 14.5(7.1~27.3) H=6.890 0.075 IBil(μmol/L) 11.2(7.7~13.6) 9.3(6.7~12.4) 13.9(9.6~18.9) 13.3(7.2~31.4) H=6.361 0.095 C3(g/L) 1.5(1.2~1.7) 1.3(1.2~1.5) 1.2(1.1~1.3) 1) 0.8(0.6~1.0)1)2)3) H=42.891 <0.001 C4(g/L) 0.21±0.11 0.22±0.09 0.20±0.08 0.15±0.08 F=1.797 0.152 IgG(g/L) 16.9±6.6 17.1±4.7 18.2±5.3 19.0±5.6 F=0.651 0.584 IgA(g/L) 3.1(2.2~3.6) 2.7(1.9~3.3) 3.1(1.9~3.8) 4.4(3.1~7.0)2) H=9.454 0.024 IgM(g/L) 2.7(1.5~5.0) 4.0(2.0~5.2) 3.2(2.4~4.8) 2.2(1.6~2.8) H=5.768 0.123 LSM(kPa) 8.4(6.5~12.1) 8.9(6.6~9.8) 18.4(14.3~24.6)1)2) 34.0(16.8~45.1)1)2) H=50.642 <0.001 AAR 1.0(0.7~1.3) 1.0(0.8~1.1) 1.2(0.9~2.1) 2.2(1.8~3.2)1)2)3) H=28.304 <0.001 APRI 0.7(0.4~1.2) 0.9(0.5~1.2) 1.1(0.4~1.7) 1.7(1.0~4.3)1) H=12.461 0.006 FIB-4 1.7(1.1~3.2) 2.3(1.4~3.0) 2.8(1.2~5.2) 8.0(5.4~10.9)1)2)3) H=27.015 <0.001 注:与S0/1分期比较,1)P<0.05;与S2分期比较,2)P<0.05;与S3分期比较,3)P<0.05。 表 3 不同肝纤维化分期患者补体C3水平的一般特征
Table 3. General characteristics of complement C3 levels in patients with different stages of hepatic fibrosis
指标 ≥S2 ≥S3 S4 C3≤1.445 g/L组 (n=76) C3>1.445 g/L组 (n=32) P值 C3≤1.235 g/L组 (n=52) C3>1.235 g/L组 (n=56) P值 C3≤1.005 g/L组 (n=22) C3>1.005 g/L组 (n=86) P值 年龄(岁) 56.0(48.0~63.0) 55.0(45.0~57.6) 0.187 56.0(48.0~63.0) 55.0(47.3~59.8) 0.538 56.1±11.8 53.0±10.0 0.206 女性[例(%)] 63(82.9) 24(75.0) 0.344 43(82.7) 44(78.6) 0.589 16(72.7) 71(82.6) 0.461 自身抗体阳性[例(%)] 72(94.7) 28(87.5) 0.190 48(92.3) 52(92.9) 1.000 20(90.9) 80(93.0) 1.000 BMI(kg/m2) 22.9(21.1~24.8) 21.7(19.7~24.3) 0.090 22.8±3.1 22.6±3.4 0.675 22.5±3.1 22.7±3.2 0.739 PLT(×109/L) 177.2±82.5 244.0±84.4 <0.001 149.5(87.0~230.0) 231.5(170.3~274.5) <0.001 100.5(72.3~172.3) 217.0(153.5~263.3) <0.001 ALT(U/L) 36.0(21.5~84.4) 57.6(36.3~115.3) 0.053 30.4(21.5~91.6) 50.9(31.3~105.5) 0.068 34.4(20.8~63.1) 49.0(24.0~103.5) 0.233 AST(U/L) 52.0(33.9~91.0) 67.4(42.1~92.8) 0.234 51.5(33.9~91.0) 60.5(34.3~92.8) 0.593 64.8(38.2~99.8) 57.0(33.1~87.8) 0.407 GGT(U/L) 190.4(92.8~324.1) 391.3(170.5~748.5) 0.006 173.5(84.0~308.7) 286.5(166.2~705.0) 0.003 168.4(96.5~324.1) 222.5(122.3~563.5) 0.173 ALP(U/L) 200.1(121.0~341.2) 391.1(195.0~494.8) 0.004 200.5(121.2~341.7) 312.8(135.3~440.5) 0.079 212.5(132.3~341.7) 240.7(122.4~416.4) 0.643 CHE(U/L) 6 065.1±2 090.8 6 471.4±2 307.2 0.390 5 379.3±1 865.4 6 903.2±2 155.3 <0.001 4 320.1±1 690.7 6 683.2±1 992.5 <0.001 Alb(g/L) 37.9±6.5 40.6±4.8 0.037 36.6±6.4 40.7±5.2 <0.001 32.8±6.3 40.3±5.1 <0.001 TBil(μmol/L) 17.0(11.3~28.6) 20.4(16.6~40.7) 0.041 17.7(11.8~27.7) 19.6(13.4~34.6) 0.448 25.3(14.5~35.6) 17.9(12.4~30.6) 0.265 DBil(μmol/L) 5.8(2.9~13.5) 8.0(4.8~21.5) 0.069 6.6(2.7~14.4) 7.4(3.9~15.6) 0.421 12.5(3.9~19.3) 5.8(3.2~13.1) 0.101 IBil(μmol/L) 11.2(7.1~14.9) 11.6(9.0~15.7) 0.498 11.7(7.5~15.4) 11.2(7.9~15.2) 0.749 13.3(7.2~18.1) 11.1(7.9~14.6) 0.377 C4(g/L) 0.19±0.09 0.24±0.12 0.007 0.16±0.08 0.24±0.10 <0.001 0.15(0.09~0.18) 0.22(0.15~0.28) 0.004 IgG(g/L) 18.1±6.4 16.3±3.8 0.082 19.0±7.1 16.2±4.0 0.015 18.5±6.3 17.3±5.7 0.403 IgA(g/L) 3.1(2.3~3.8) 2.9(1.9~3.7) 0.348 3.2(2.1~3.9) 3.0(2.1~3.6) 0.246 4.1(2.6~6.3) 3.0(2.1~3.6) 0.006 IgM(g/L) 2.9(1.8~4.8) 2.8(1.7~5.7) 0.597 2.6(1.4~4.8) 3.0(2.0~5.1) 0.155 2.3(1.6~4.8) 3.0(1.8~4.8) 0.358 LSM(kPa) 14.2(8.2~21.6) 8.9(6.5~12.6) 0.002 15.4(9.0~24.6) 8.9(6.6~14.0) <0.001 22.7(15.3~42.0) 9.3(6.8~14.6) <0.001 AAR 1.2(0.9~1.9) 0.9(0.7~1.3) 0.017 1.4(0.9~2.1) 1.0(0.7~1.4) 0.004 1.8(1.2~2.5) 1.0(0.8~1.5) <0.001 APRI 1.1(0.5~1.8) 0.7(0.4~1.1) 0.058 1.1(0.5~1.9) 0.8(0.4~1.1) 0.054 1.4(0.6~2.6) 0.8(0.4~1.3) 0.023 FIB-4 2.8(1.7~5.4) 1.7(1.1~3.1) 0.012 3.0(1.7~5.9) 1.9(1.2~3.5) 0.023 6.1(1.8~9.1) 2.2(1.4~3.6) 0.002 肝纤维化分期[例(%)] <0.001 <0.001 <0.001 S0 2(2.6) 3(9.4) 1(1.9) 4(7.1) 1(4.5) 4(4.7) S1 21(27.6) 20(62.5) 14(26.9) 27(48.2) 4(18.2) 37(43.0) S2 17(22.4) 6(18.8) 6(11.5) 17(30.4) 0(0.0) 23(26.7) S3 22(28.9) 3(9.4) 17(32.7) 8(14.3) 4(18.2) 21(24.4) S4 14(18.4) 0(0.0) 14(26.9) 0(0.0) 13(59.1) 1(1.2) 表 4 不同肝纤维化分期指标的单因素分析
Table 4. Univariate analysis of different liver fibrosis staging indicators
指标 ≥S2 ≥S3 S4 OR(95%CI) P值 OR(95%CI) P值 OR(95%CI) P值 年龄(岁) 0.987(0.377~2.585) 0.978 1.003(0.965~1.041) 0.895 1.013(0.958~1.071) 0.653 性别 1.010(0.973~1.048) 0.606 0.859(0.314~2.351) 0.768 0.658(0.136~3.192) 0.603 自身抗体阳性 1.372(0.264~7.129) 0.707 0.545(0.105~2.843) 0.472 0.73(0.079~6.755) 0.782 BMI(kg/m2) 1.002(0.889~1.130) 0.973 1.002(0.886~1.134) 0.971 0.974(0.813~1.166) 0.771 PLT(×109/L) 0.993(0.988~0.997) 0.003 0.991(0.985~0.996) 0.001 0.987(0.978~0.996) 0.003 ALT(U/L) 0.999(0.997~1.002) 0.644 0.999(0.996~1.002) 0.492 0.986(0.970~1.003) 0.114 AST(U/L) 1.001(0.997~1.004) 0.754 1.000(0.997~1.003) 0.805 1.000(0.996~1.004) 0.821 GGT(U/L) 1.000(0.999~1.001) 0.656 1.000(0.998~1.001) 0.460 0.998(0.996~1.001) 0.234 ALP(U/L) 1.000(0.998~1.001) 0.964 1.000(0.998~1.002) 0.923 1.001(0.999~1.003) 0.476 CHE(U/L) 1.000(1.000~1.000) 0.045 1.000(0.999~1.000) <0.001 0.999(0.999~1.000) <0.001 Alb(g/L) 0.944(0.883~1.009) 0.090 0.893(0.830~0.961) 0.003 0.728(0.623~0.850) <0.001 TBil(μmol/L) 1.009(0.993~1.026) 0.259 1.020(1.002~1.039) 0.033 1.010(0.996~1.023) 0.153 DBil(μmol/L) 1.007(0.989~1.025) 0.465 1.018(0.997~1.04) 0.090 1.009(0.992~1.026) 0.321 IBil(μmol/L) 1.042(0.991~1.095) 0.105 1.066(1.012~1.122) 0.015 1.047(1.004~1.092) 0.032 C3(g/L) 0.048(0.011~0.210) <0.001 0.006(0.001~0.052) <0.001 0.000(0.000~0.007) <0.001 C4(g/L) 0.212(0.004~10.707) 0.438 0.034(0.001~2.234) 0.113 0.001(0.000~0.508) 0.031 IgG(g/L) 1.035(0.965~1.109) 0.335 1.047(0.977~1.122) 0.191 1.047(0.960~1.142) 0.302 IgA(g/L) 1.127(0.881~1.442) 0.342 1.268(0.989~1.625) 0.061 1.727(1.251~2.385) 0.001 IgM(g/L) 1.093(0.898~1.331) 0.376 1.007(0.826~1.228) 0.945 0.798(0.573~1.113) 0.183 LSM(kPa) 1.147(1.064~1.236) <0.001 1.299(1.168~1.445) <0.001 1.108(1.055~1.163) <0.001 AAR 2.155(1.196~3.885) 0.011 3.024(1.658~5.517) <0.001 3.145(1.688~5.858) <0.001 APRI 1.021(0.904~1.153) 0.739 1.072(0.947~1.212) 0.273 1.111(0.980~1.259) 0.099 FIB-4 1.234(1.031~1.478) 0.022 1.333(1.115~1.594) 0.002 1.541(1.225~1.938) <0.001 表 5 不同肝纤维化分期调节混杂因素后指标的多因素分析
Table 5. Multi-factor analysis of indicators after adjustment of confounding factors for different liver fibrosis stages
指标 ≥S2 ≥S3 S4 OR(95%CI) P值 OR(95%CI) P值 OR(95%CI) P值 模型1 C3(g/L) 0.116(0.020~0.684) 0.017 0.013(0.001~0.309) 0.007 0.001(0.000~0.159) 0.009 LSM(kPa) 1.102(1.009~1.204) 0.031 1.277(1.115~1.464) <0.001 1.057(0.984~1.135) 0.129 模型2 C3(g/L) 0.108(0.018~0.633) 0.014 0.010(0.000~0.244) 0.005 0.000(0.000~0.118) 0.007 LSM(kPa) 1.103(1.009~1.205) 0.031 1.288(1.121~1.479) <0.001 1.033(0.955~1.117) 0.421 模型3 C3(g/L) 0.091(0.016~0.528) 0.008 0.005(0.000~0.145) 0.002 0.001(0.000~0.179) 0.011 LSM(kPa) 1.134(1.029~1.251) 0.012 1.383(1.164~1.643) <0.001 1.051(0.978~1.128) 0.175 模型4 C3(g/L) 0.082(0.014~0.487) 0.006 0.003(0.000~0.103) 0.001 0.001(0.000~0.168) 0.010 LSM(kPa) 1.134(1.030~1.248) 0.010 1.381(1.169~1.631) <0.001 1.028(0.953~1.108) 0.481 注:除了最终模型所示的变量外,以下也包括在初始模型中:模型1 PLT、CHE和AAR,模型2 PLT、CHE、FIB-4,模型3 PLT、Alb和AAR,模型4 PLT、Alb和FIB-4。 表 6 C3、LSM及C3联合LSM对不同肝纤维化分期的诊断性能
Table 6. Diagnostic performance of C3, LSM and C3 combined with LSM for different liver fibrosis stages
指标 C3 LSM C3联合LSM ≥S2 ≥S3 S4 ≥S2 ≥S3 S4 ≥S2 ≥S3 S4 AUC 0.731 0.832 0.968 0.764 0.911 0.910 0.811 0.941 0.976 P值 <0.001 <0.001 <0.001 <0.001 <0.001 <0.001 <0.001 <0.001 <0.001 95%CI 0.637~0.812 0.748~0.897 0.915~0.992 0.672~0.840 0.840~0.957 0.839~0.956 0.725~0.880 0.879~0.977 0.926~0.996 约登指数 0.393 0.531 0.915 0.504 0.756 0.745 0.542 0.782 0.915 敏感度(%) 87.10 82.05 100.00 61.29 87.18 100.00 62.90 89.74 100.00 特异度(%) 52.17 71.01 91.49 89.13 88.41 74.47 91.30 88.41 91.49 阳性预测值(%) 71.1 61.5 63.6 88.4 81.0 36.8 90.7 81.4 63.6 阴性预测值(%) 75.0 87.5 100.0 63.1 92.4 100.0 64.6 93.8 100.0 阳性似然比 1.82 2.83 11.75 5.64 7.52 3.92 7.23 7.74 11.75 阴性似然比 0.25 0.25 0.00 0.43 0.15 0.00 0.41 0.12 0.00 -
[1] COLAPIETRO F, BERTAZZONI A, LLEO A. Contemporary epidemiology of primary biliary cholangitis[J]. Clin Liver Dis, 2022, 26( 4): 555- 570. DOI: 10.1016/j.cld.2022.06.001. [2] Chinese Society of Hepatology, Chinese Society of Gastroenterology, Chinese Society of Infectious Diseases. Consensus on the diagnosis and treatment of primary biliary cirrhosis(also known as primary biliary cholangitis)(2015)[J]. J Clin Hepatol, 2015, 31( 12): 1980- 1988. DOI: 10.3969/j.issn.1001-5256.2015.12.004.中华医学会肝病学分会, 中华医学会消化病学分会, 中华医学会感染病学分会. 原发性胆汁性肝硬化(又名原发性胆汁性胆管炎)诊断和治疗共识(2015)[J]. 临床肝胆病杂志, 2015, 31( 12): 1980- 1988. DOI: 10.3969/j.issn.1001-5256.2015.12.004. [3] Chinese Medical Association, Branch Hepatology. Guidelines for the diagnosis and treatment of primary biliary cholangitis(2021)[J]. J Clin Hepatol, 2022, 38( 1): 35- 41. DOI: 10.3969/j.issn.1001-5256.2022.01.007.中华医学会肝病学分会. 原发性胆汁性胆管炎的诊断和治疗指南(2021)[J]. 临床肝胆病杂志, 2022, 38( 1): 35- 41. DOI: 10.3969/j.issn.1001-5256.2022.01.007. [4] Chinese Society of Hepatology, Chinese Society of Gastroenterology, Chinese Society of Infectious Diseases. Consensus on the diagnosis and treatment of liver fibrosis(2019)[J]. J Clin Hepatol, 2019, 35( 10): 2163- 2172. DOI: 10.3969/j.issn.1001-5256.2019.10.007.中华医学会肝病学分会, 中华医学会消化病学分会, 中华医学会感染病学分会. 肝纤维化诊断及治疗共识(2019年)[J]. 临床肝胆病杂志, 2019, 35( 10): 2163- 2172. DOI: 10.3969/j.issn.1001-5256.2019.10.007. [5] TRIVEDI PJ, HIRSCHFIELD GM. Recent advances in clinical practice: Epidemiology of autoimmune liver diseases[J]. Gut, 2021, 70( 10): 1989- 2003. DOI: 10.1136/gutjnl-2020-322362. [6] HOHENESTER S, OUDE-ELFERINK RPJ, BEUERS U. Primary biliary cirrhosis[J]. Semin Immunopathol, 2009, 31( 3): 283- 307. DOI: 10.1007/s00281-009-0164-5. [7] YANG YL, ZHAO RC, ZHANG FC. Potential mesenchymal stem cell therapeutics for treating primary biliary cholangitis: Advances, challenges, and perspectives[J]. Front Cell Dev Biol, 2022, 10: 933565. DOI: 10.3389/fcell.2022.933565. [8] BUGDACI MS, ALKIM C, KARACA C, et al. Could complement C4 be an alternative to biopsy for chronic hepatitis B histopathologic findings?[J]. J Clin Gastroenterol, 2011, 45( 5): 449- 455. DOI: 10.1097/MCG.0b013e31820f7ee5. [9] LI Q, LU Q, ZHU MQ, et al. Lower level of complement component C3 and C3a in the plasma means poor outcome in the patients with hepatitis B virus related acute-on-chronic liver failure[J]. BMC Gastroenterol, 2020, 20( 1): 106. DOI: 10.1186/s12876-020-01258-3. [10] CHEN C, YUAN Z, LI WX, et al. Complement C3 facilitates stratification of stages of chronic hepatitis B and signifies development of acute-on-chronic liver failure in acute decompensated cirrhosis[J]. Adv Ther, 2023, 40( 3): 1171- 1186. DOI: 10.1007/s12325-022-02416-7. [11] RICKLIN D, HAJISHENGALLIS G, YANG K, et al. Complement: A key system for immune surveillance and homeostasis[J]. Nat Immunol, 2010, 11( 9): 785- 797. DOI: 10.1038/ni.1923. [12] TROUW LA, DAHA MR. Role of complement in innate immunity and host defense[J]. Immunol Lett, 2011, 138( 1): 35- 37. DOI: 10.1016/j.imlet.2011.02.014. [13] SAHU A, LAMBRIS JD. Structure and biology of complement protein C3, a connecting link between innate and acquired immunity[J]. Immunol Rev, 2001, 180: 35- 48. DOI: 10.1034/j.1600-065x.2001.1800103.x. [14] LUBBERS R, van ESSEN MF, van KOOTEN C, et al. Production of complement components by cells of the immune system[J]. Clin Exp Immunol, 2017, 188( 2): 183- 194. DOI: 10.1111/cei.12952. [15] SELMI C, BOWLUS CL, GERSHWIN ME, et al. Primary biliary cirrhosis[J]. Lancet, 2011, 377( 9777): 1600- 1609. DOI: 10.1016/S0140-6736(10)61965-4. [16] SCHLESINGER M, BENBASSAT C, SHOENFELD Y. Complement profile in primary biliary cirrhosis[J]. Immunol Res, 1992, 11( 2): 98- 103. DOI: 10.1007/BF02918614. [17] BARAK V, SELMI C, SCHLESINGER M, et al. Serum inflammatory cytokines, complement components, and soluble interleukin 2 receptor in primary biliary cirrhosis[J]. J Autoimmun, 2009, 33( 3-4): 178- 182. DOI: 10.1016/j.jaut.2009.09.010. [18] BIEWENGA M, FARINA SARASQUETA A, TUSHUIZEN ME, et al. The role of complement activation in autoimmune liver disease[J]. Autoimmun Rev, 2020, 19( 6): 102534. DOI: 10.1016/j.autrev.2020.102534. [19] HOMANN C, VARMING K, HØGÅSEN K, et al. Acquired C3 deficiency in patients with alcoholic cirrhosis predisposes to infection and increased mortality[J]. Gut, 1997, 40( 4): 544- 549. DOI: 10.1136/gut.40.4.544. [20] GARRED P, LYON H, CHRISTOFFERSEN P, et al. Deposition of C3, the terminal complement complex and vitronectin in primary biliary cirrhosis and primary sclerosing cholangitis[J]. Liver, 1993, 13( 6): 305- 310. DOI: 10.1111/j.1600-0676.1993.tb00650.x. [21] YUAN H, LI YW, LI J, et al. Clinical feature of patients with primary biliary cholangitis and primary biliary cirrhosis[J]. J Pract Hepatol, 2022, 25( 3): 403- 406. DOI: 10.3969/j.issn.1672-5069.2022.03.025.袁慧, 李毓雯, 李军, 等. 原发性胆汁性胆管炎与肝硬化患者临床指标差异分析[J]. 实用肝脏病杂志, 2022, 25( 3): 403- 406. DOI: 10.3969/j.issn.1672-5069.2022.03.025. -



 PDF下载 ( 1065 KB)
PDF下载 ( 1065 KB)

 下载:
下载: