肝纤维化-4指数(FIB-4)联合预后营养指数(PNI)对早期肝癌射频消融术后复发及生存期的预测价值
DOI: 10.3969/j.issn.1001-5256.2023.11.015
Value of fibrosis-4 combined with prognostic nutritional index in predicting recurrence and survival time after radiofrequency ablation for early-stage hepatocellular carcinoma
-
摘要:
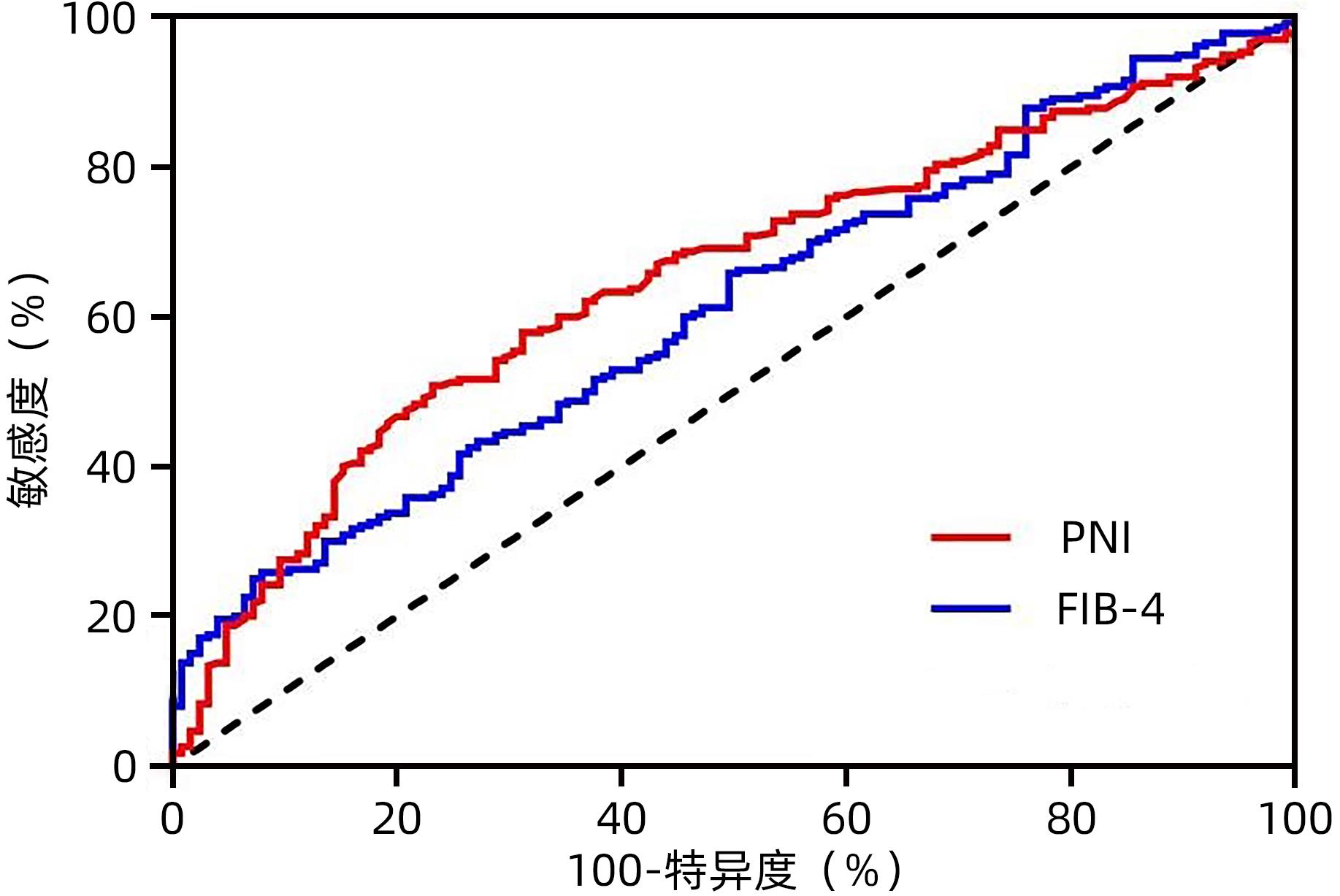
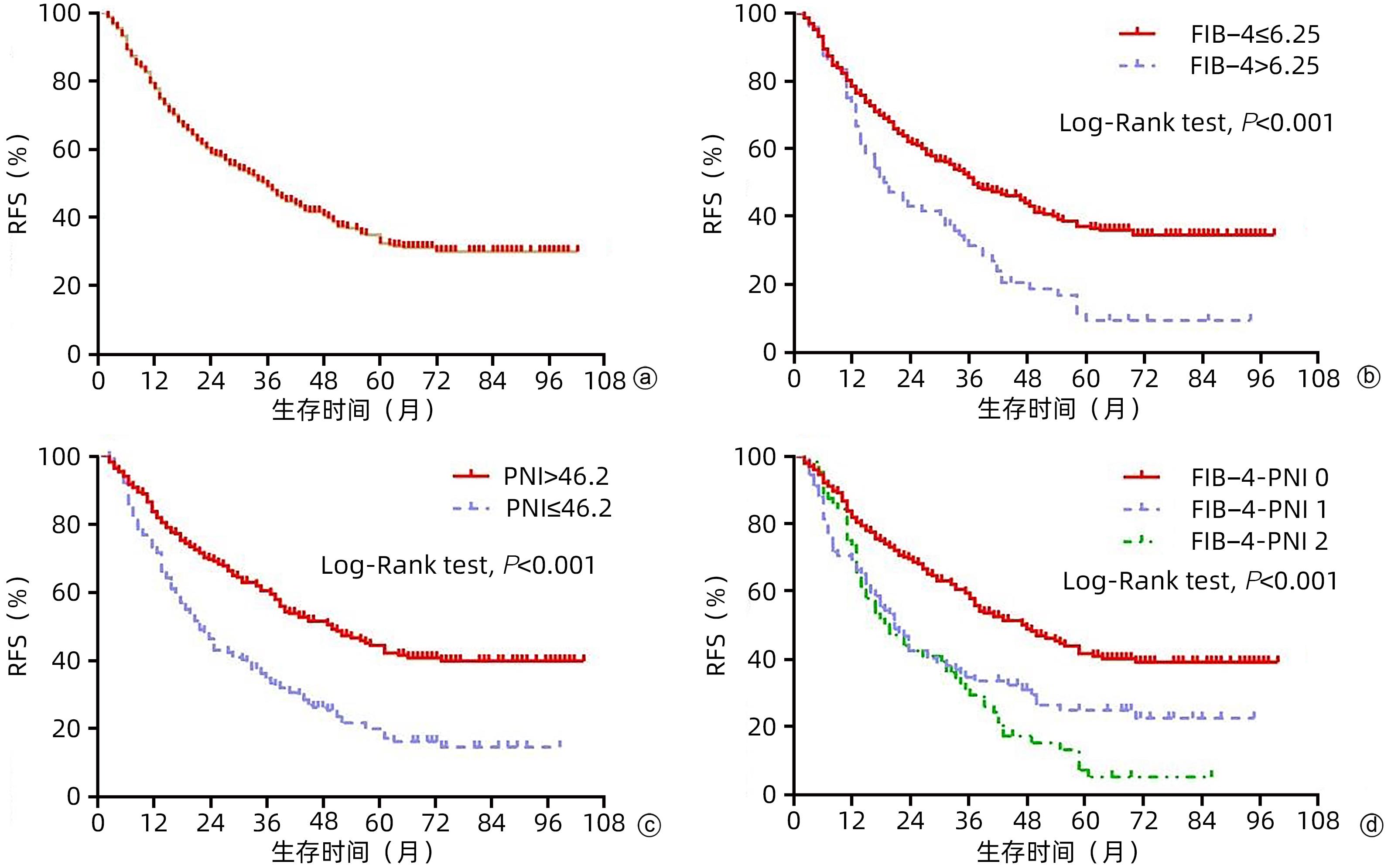
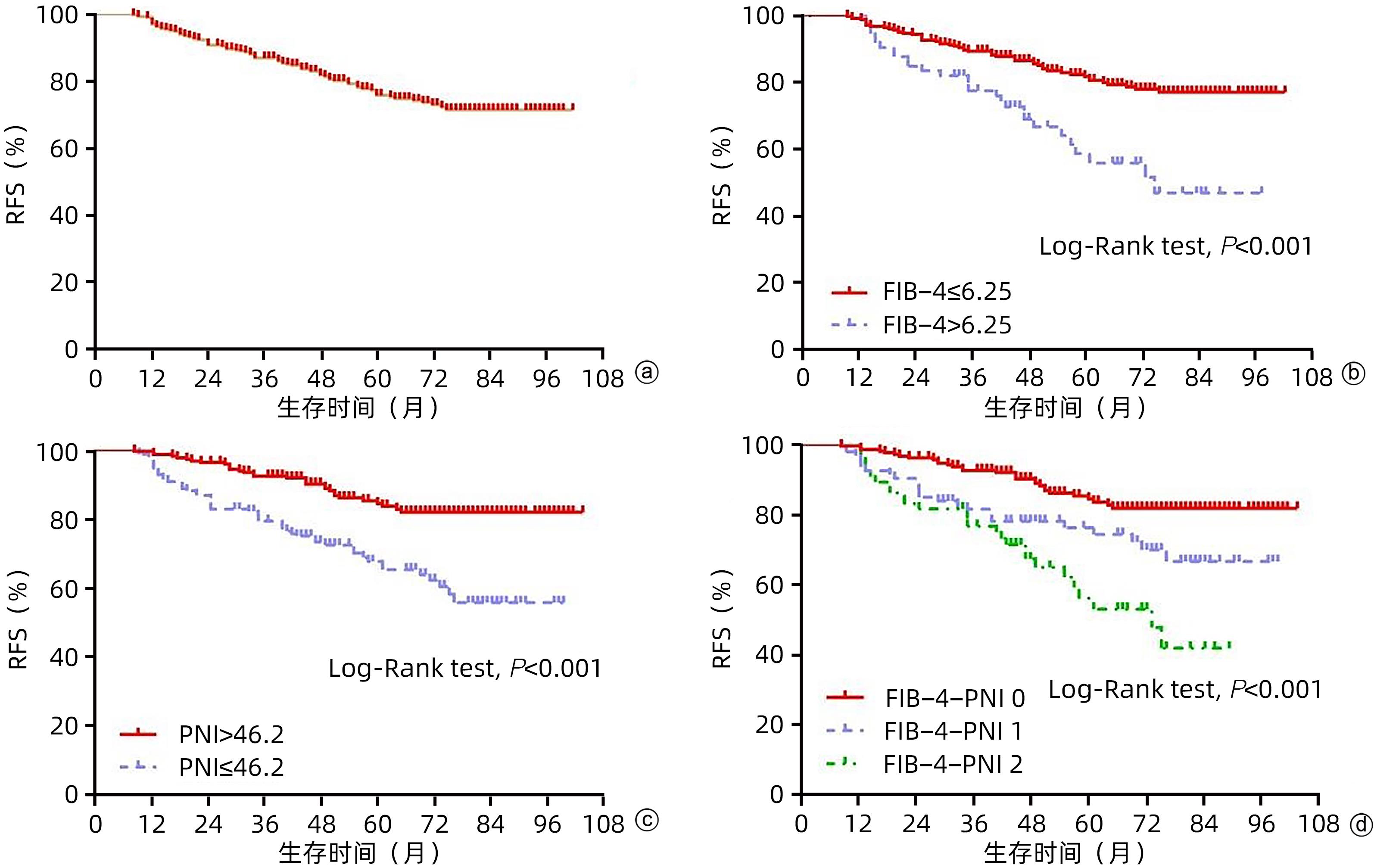
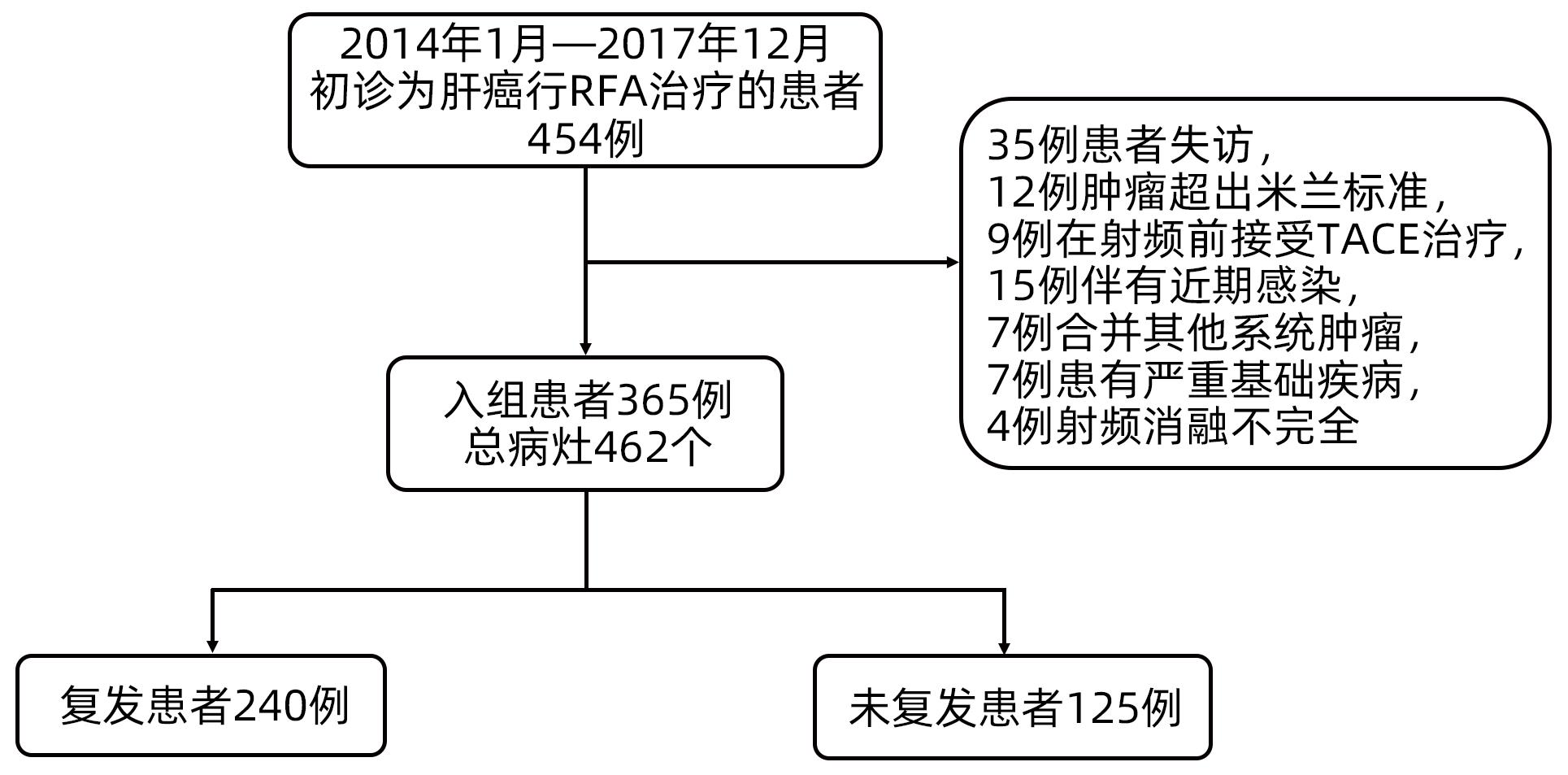
目的 探讨术前肝纤维化-4指数(FIB-4)联合预后营养指数(PNI)对于早期肝癌射频治疗(RFA)术后复发的预测价值。 方法 回顾性分析2013年1月—2017年12月于天津市第三中心医院行RFA的365例初诊为早期肝癌患者的临床资料,统计患者的复发及生存情况。以术后肿瘤复发为阳性事件绘制FIB-4、PNI的ROC曲线,选取最佳cut-off值,进行FIB-4和PNI的分级,组合为FIB-4-PNI评分,据此分为FIB-4-PNI 0分组(n=207)、1分组(n=93)和2分组(n=65)。计数资料组间比较采用χ2检验。采用Kaplan-Meier生存分析及Log-rank检验分析不同FIB-4-PNI等级组无复发生存率(RFS)及总生存率(OS)的差异。采用Cox回归模型筛选影响患者RFS、OS的相关因素。 结果 所有患者的1、3和5年RFS率分别为79.2%、49.8%和34.3%,中位RFS为35个月,1、3和5年OS率分别为98.9%、86.9%和77.3%。不同FIB-4、PNI、FIB-4-PNI水平患者累积RFS率(χ2值分别为17.890、29.826、32.397,P值均<0.001)、OS率(χ2值分别为16.896、21.070、26.121,P值均<0.001)差异均有统计学意义。多因素Cox回归分析显示,糖尿病史(HR=1.418,95%CI:1.046~1.922,P=0.024),肿瘤数目2个(HR=1.516,95%CI:1.094~2.101,P=0.012)、3个(HR=2.146,95%CI:1.278~3.604,P=0.004),FIB-4-PNI 1分(HR=1.875,95%CI:1.385~2.539,P<0.001)、2分(HR=2.350,95%CI:1.706~3.236,P<0.001)是RFS的独立危险因素;肿瘤数目2个(HR=1.732,95%CI:1.005~2.983,P=0.048)、3个(HR=3.511,95%CI:1.658~7.433,P=0.001),FIB-4-PNI 1分(HR=2.094,95%CI:1.230~3.565,P=0.006)、2分(HR=3.908,95%CI:2.306~6.624,P<0.001)是影响OS的独立危险因素。 结论 FIB-4-PNI评分可作为早期肝癌RFA术后复发及总生存期的独立预测因素,可联合肿瘤特征预测患者术后的复发及生存情况。 Abstract:Objective To investigate the value of preoperative fibrosis 4 score (FIB-4) combined with prognostic nutritional index (PNI) in predicting recurrence after radiofrequency ablation (RFA) for early-stage hepatocellular carcinoma (HCC). Methods A retrospective analysis was performed for the clinical data of 365 patients with the initial diagnosis of early-stage HCC who underwent RFA at Tianjin Third Central Hospital from January 2013 to December 2017, and a statistical analysis was performed for recurrence and survival. The receiver operating characteristic (ROC) curve was plotted for FIB-4 and PNI with postoperative tumor recurrence as the positive event, and their optimal cut-off values were selected. FIB-4 and PNI were graded and combined as FIB-4-PNI score, based on which the patients were divided into 0-point group with 207 patients, 1-point group with 93 patients, and 2-point group with 65 patients. The chi-square test was used for comparison of categorical data between groups. The Kaplan-Meier survival analysis and the log-rank test were used to compare the recurrence-free survival (RFS) and overall survival (OS) between groups, and the Cox regression model was used to investigate the influencing factors for RFS and OS. Results The 1-, 3-, and 5-year RFS rates of all patients were 79.2%, 49.8%, and 34.3%, respectively, with a median RFS of 35 months, while the 1-, 3-, and 5-year OS rates of all patients were 98.9%, 86.9%, and 77.3%, respectively. There were significant differences in cumulative RFS and OS rates between the patients with different levels of FIB-4, PNI, and FIB-4-PNI (RFS rate: χ2=17.890, 29.826, and 32.397, all P<0.001; OS rate: χ2=16.896, 21.070, and 26.121, all P<0.001). The multivariate Cox regression analysis showed that history of diabetes (hazard ratio [HR]=1.418, 95% confidence interval [CI]: 1.046 — 1.922, P=0.024), two tumors (HR=1.516, 95%CI: 1.094 — 2.101, P=0.012), three tumors (HR=2.146, 95%CI: 1.278 — 3.604, P=0.004), FIB-4-PNI 1 point (HR=1.875, 95%CI: 1.385 — 2.539, P<0.001), and FIB-4-PNI 2 points (HR=2.35, 95%CI: 1.706 — 3.236, P<0.001) were independent risk factors for RFS, while two tumors (HR=1.732, 95%CI: 1.005 — 2.983, P=0.048), three tumors (HR=3.511, 95%CI: 1.658 — 7.433, P=0.001), FIB-4-PNI 1 point (HR=2.094, 95%CI: 1.230 — 3.565, P=0.006), and FIB-4-PNI 2 points (HR=3.908, 95%CI: 2.306 — 6.624, P<0.001) were independent risk factors for OS. Conclusion FIB-4-PNI score can be used as an independent predictive factor for recurrence and overall survival time after RFA for early-stage HCC, and it can be combined with tumor features to predict postoperative recurrence and survival. -
Key words:
- Carcinoma, Hepatocellular /
- Radiofrequency Ablation /
- Nutrition Assessment /
- Prognosis
-
表 1 FIB-4和PNI联合作为预后指标分组标准
Table 1. Combination of FIB-4 and PNI as recurrence indices
变量 评分(分) FIB-4 ≤6.25 0 >6.25 1 PNI ≤46.20 1 >46.20 0 FIB-4-PNI FIB-4=0和PNI=0 0 FIB-4=1和PNI=1 1 FIB-4=2和PNI=2 2 表 2 不同FIB-4-PNI水平组临床资料比较
Table 2. Comparison of clinical data between different FIB-4-PNI grades
指标 FIB-4-PNI 0分组 (n=207) FIB-4-PNI 1分组 (n=93) FIB-4-PNI 2分组 (n=65) χ2值 P值 年龄[例(%)] 2.771 0.250 <55岁 46(22.2) 29(31.2) 17(26.2) ≥55岁 161(77.8) 64(68.8) 48(73.8) 性别[例(%)] 1.352 0.509 女 46(22.2) 26(28.0) 14(21.5) 男 161(77.8) 67(72.0) 51(78.5) 肝硬化[例(%)] 174(84.1) 91(97.8) 60(92.3) 13.373 0.001 肝癌家族史[例(%)] 28(13.5) 7(7.5) 11(16.9) 3.437 0.179 糖尿病病史[例(%)] 46(22.2) 19(20.4) 11(16.9) 0.854 0.652 肝病原因[例(%)] 6.968 0.314 乙型肝炎 170(82.1) 76(81.7) 47(72.3) 丙型肝炎 14(6.8) 10(10.8) 9(13.8) 酒精肝 13(6.3) 3(3.2) 3(4.6) 其他 10(4.8) 4(4.3) 6(9.2) ALT[例(%)] 6.708 0.035 ≤45 U/L 176(85.0) 76(81.7) 46(70.8) >45 U/L 31(15.0) 17(18.3) 19(29.2) AST[例(%)] 89.514 <0.001 ≤45 U/L 188(90.8) 78(83.9) 24(36.9) >45 U/L 19(9.2) 15(16.1) 41(63.1) Alb[例(%)] 111.260 <0.001 ≥35 g/L 207(100.0) 72(77.4) 31(47.7) <35 g/L 0(0) 21(22.6) 34(52.3) TBil[例(%)] 48.447 <0.001 ≤20 μmol/L 165(79.7) 64(68.8) 22(33.8) >20 μmol/L 42(20.3) 29(31.2) 43(66.2) PLT[例(%)] 100.611 <0.001 ≥100×109/L 160(77.3) 42(45.2) 6(9.2) <100×109/L 47(22.7) 51(54.8) 59(90.8) 淋巴细胞计数[例(%)] 76.494 <0.001 ≤1.18×109/L 63(30.4) 66(71.0) 54(83.1) >1.18×109/L 144(69.6) 27(29.0) 11(16.9) AFP[例(%)] 8.285 0.016 ≤15 ng/mL 123(59.4) 46(49.5) 26(40.0) >15 ng/mL 84(40.6) 47(50.5) 39(60.0) ALBI分级[例(%)] 229.489 <0.001 1级 191(92.3) 31(33.3) 4(6.2) 2级 16(7.7) 62(66.7) 54(83.1) 3级 0(0) 0(0) 7(10.8) 肿瘤数目[例(%)] 0.765 0.954 1个 164(79.2) 72(77.4) 51(78.5) 2个 32(15.5) 17(18.3) 10(15.4) 3个 11(5.3) 4(4.3) 4(6.2) 肿瘤直径[例(%)] 8.699 0.013 ≤2.5 cm 102(49.3) 55(59.1) 45(69.2) >2.5 cm 105(50.7) 38(40.9) 20(30.8) BCLC分期[例(%)] 2.609 0.271 0期 52(25.1) 26(28.0) 23(35.4) A期 155(74.9) 67(72.0) 42(64.6) 表 3 影响患者RFS的Cox回归模型分析
Table 3. Analysis of Cox proportional hazards model affecting RFS
因素 单因素分析 多因素分析 HR(95%CI) χ2值 P值 HR(95%CI) χ2值 P值 年龄(<55岁/≥55岁) 1.123(0.834~1.511) 0.580 0.446 性别(女/男) 1.107(0.816~1.502) 0.426 0.514 肝硬化(无/有) 1.468(0.929~2.321) 2.704 0.100 肝病原因 1.294 0.730 乙型肝炎 1.000 丙型肝炎 0.790(0.499~1.252) 1.008 0.315 酒精肝 0.981(0.547~1.758) 0.004 0.949 其他 0.835(0.466~1.496) 0.368 0.544 肝癌家族史(无/有) 1.128(0.777~1.637) 0.401 0.527 糖尿病史(无/有) 1.392(1.029~1.882) 4.614 0.032 1.418(1.046~1.922) 5.068 0.024 AFP(≤15 ng/mL/>15 ng/mL) 1.255(0.974~1.616) 3.089 0.079 ALBI分级 22.179 <0.001 1级 1.000 2级 1.856(1.434~2.402) 22.105 <0.001 3级 1.500(0.613~3.667) 0.790 0.374 肿瘤数目 12.565 0.002 12.856 0.002 1个 1.000 1.000 2个 1.515(1.095~2.096) 6.291 0.012 1.516(1.094~2.101) 6.245 0.012 3个 2.088(1.251~3.487) 7.925 0.005 2.146(1.278~3.604) 8.340 0.004 肿瘤直径(≤2.5 cm/>2.5 cm) 1.055(0.817~1.361) 0.167 0.683 BCLC分期(0期/A期) 1.245(0.933~1.663) 2.210 0.137 FIB-4-PNI 30.337 <0.001 32.828 <0.001 0分 1.000 1.000 1分 1.764(1.306~2.384) 13.668 <0.001 1.875(1.385~2.539) 16.530 <0.001 2分 2.308(1.678~3.176) 26.395 <0.001 2.350(1.706~3.236) 27.339 <0.001 表 4 影响患者OS的Cox回归模型分析
Table 4. Analysis of Cox proportional hazards model affecting OS
因素 单因素分析 多因素分析 HR(95%CI) χ2值 P值 HR(95%CI) χ2值 P值 年龄(<55岁/≥55岁) 0.688(0.432~1.096) 2.481 0.115 性别(女/男) 0.884(0.538~1.452) 0.236 0.627 肝硬化(无/有) 3.188(1.006~10.099) 3.883 0.049 肝病原因 0.335 0.953 乙型肝炎 1.000 丙型肝炎 1.207(0.601~2.424) 0.281 0.596 酒精肝 1.150(0.418~3.163) 0.074 0.786 其他 1.005(0.366~2.760) 0.000 0.993 肝癌家族史(无/有) 1.247(0.689~2.255) 0.531 0.466 糖尿病史(无/有) 1.065(0.624~1.817) 0.053 0.817 AFP(≤15 ng/mL/>15 ng/mL) 1.577(1.018~2.443) 4.166 0.041 ALBI分级 18.443 <0.001 1级 1.000 2级 2.522(1.617~3.936) 16.609 <0.001 3级 3.762(1.152~12.286) 4.813 0.028 肿瘤数目 9.839 0.007 12.787 0.002 1个 1.000 1.000 2个 1.647(0.958~2.833) 3.258 0.071 1.732(1.005~2.983) 3.913 0.048 3个 2.922(1.392~6.132) 8.033 0.005 3.511(1.658~7.433) 10.768 0.001 肿瘤直径(≤2.5 cm/>2.5 cm) 1.323(0.858~2.040) 1.602 0.206 BCLC分期(0期/A期) 1.703(0.986~2.940) 3.645 0.056 FIB-4-PNI 23.400 <0.001 25.812 <0.001 0分 1.000 1.000 1分 2.060(1.211~3.504) 7.118 0.008 2.094(1.230~3.565) 7.411 0.006 2分 3.606(2.139~6.081) 23.159 <0.001 3.908(2.306~6.624) 25.640 <0.001 -
[1] BRAY F, FERLAY J, SOERJOMATARAM I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2018, 68( 6): 394- 424. DOI: 10.3322/caac.21492. [2] YANG JD, HAINAUT P, GORES GJ, et al. A global view of hepatocellular carcinoma: Trends, risk, prevention and management[J]. Nat Rev Gastroenterol Hepatol, 2019, 16( 10): 589- 604. DOI: 10.1038/s41575-019-0186-y. [3] FENG K, YAN J, LI XW, et al. A randomized controlled trial of radiofrequency ablation and surgical resection in the treatment of small hepatocellular carcinoma[J]. J Hepatol, 2012, 57( 4): 794- 802. DOI: 10.1016/j.jhep.2012.05.007. [4] DHIR M, MELIN AA, DOUAIHER J, et al. A review and update of treatment options and controversies in the management of hepatocellular carcinoma[J]. Ann Surg, 2016, 263( 6): 1112- 1125. DOI: 10.1097/SLA.0000000000001556. [5] TSAI MY, YEN YH, HUANG PY, et al. The pre- and postoperative FIB-4 indexes are good predictors to the outcomes of HBV-related HCC patients after resection[J]. Gastroenterol Res Pract, 2019, 2019: 8945798. DOI: 10.1155/2019/8945798. [6] SAITO Y, IMURA S, MORINE Y, et al. Preoperative prognostic nutritional index predicts short- and long-term outcomes after liver resection in patients with hepatocellular carcinoma[J]. Oncol Lett, 2021, 21( 2): 153. DOI: 10.3892/ol.2020.12414. [7] CHU MO, SHEN CH, CHANG TS, et al. Pretreatment inflammation-based markers predict survival outcomes in patients with early stage hepatocellular carcinoma after radiofrequency ablation[J]. Sci Rep, 2018, 8( 1): 16611. DOI: 10.1038/s41598-018-34543-z. [8] General Office of National Health Commission. Standard for diagnosis and treatment of primary liver cancer(2022 edition)[J]. J Clin Hepatol, 2022, 38( 2): 288- 303. DOI: 10.3969/j.issn.1001-5256.2022.02.009.国家卫生健康委办公厅. 原发性肝癌诊疗指南(2022年版)[J]. 临床肝胆病杂志, 2022, 38( 2): 288- 303. DOI: 10.3969/j.issn.1001-5256.2022.02.009. [9] ONODERA T, GOSEKI N, KOSAKI G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients[J]. Nihon Geka Gakkai Zasshi, 1984, 85( 9): 1001- 1005. [10] STERLING RK, LISSEN E, CLUMECK N, et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection[J]. Hepatology, 2006, 43( 6): 1317- 1325. DOI: 10.1002/hep.21178. [11] Chinese Expert Consensus Statement Chinese Society of Liver Cancer CSLC, Chinese Society of Clinical Oncology CSCO, Liver Cancer Group, Chinese Society of Hepatology. Guidelines for radiofrequency ablation therapy of liver cancer[J]. J Clin Hepatol, 2011, 27( 3): 236- 238, 244.中国抗癌协会肝癌专业委员会, 中国抗癌协会临床肿瘤学协作委员会, 中华医学会肝病学分会肝癌学组. 肝癌射频消融治疗规范的专家共识[J]. 临床肝胆病杂志, 2011, 27( 3): 236- 238, 244. [12] KULIK L, EL-SERAG HB. Epidemiology and management of hepatocellular carcinoma[J]. Gastroenterology, 2019, 156( 2): 477- 491. e 1. DOI: 10.1053/j.gastro.2018.08.065. [13] WEI CY, CHAU GY, CHEN PH, et al. A comparison of prognoses between surgical resection and radiofrequency ablation therapy for patients with hepatocellular carcinoma and esophagogastric varices[J]. Sci Rep, 2020, 10( 1): 17259. DOI: 10.1038/s41598-020-74424-y. [14] GUPTA P, MARALAKUNTE M, KUMAR-M P, et al. Overall survival and local recurrence following RFA, MWA, and cryoablation of very early and early HCC: A systematic review and Bayesian network meta-analysis[J]. Eur Radiol, 2021, 31( 7): 5400- 5408. DOI: 10.1007/s00330-020-07610-1. [15] ZHANG F, LU SX, HU KS, et al. Albumin-to-alkaline phosphatase ratio as a predictor of tumor recurrence and prognosis in patients with early-stage hepatocellular carcinoma undergoing radiofrequency ablation as initial therapy[J]. Int J Hyperthermia, 2021, 38( 1): 1- 10. DOI: 10.1080/02656736.2020.1850885. [16] CHU WK, WU X, ZHANG P, et al. Value of inflammatory biomarkers in predicting the prognosis of early small hepatocellular carcinoma after radiofre-quency ablation[J]. J Clin Hepatol, 2022, 38( 4): 843- 850. DOI: 10.3969/j.issn.1001-5256.2022.04.020.楚伟可, 吴雪, 张鹏, 等. 炎症标志物对早期小肝癌行射频消融术预后的预测价值[J]. 临床肝胆病杂志, 2022, 38( 4): 843- 850. DOI: 10.3969/j.issn.1001-5256.2022.04.020. [17] O’ROURKE JM, SAGAR VM, SHAH T, et al. Carcinogenesis on the background of liver fibrosis: Implications for the management of hepatocellular cancer[J]. World J Gastroenterol, 2018, 24( 39): 4436- 4447. DOI: 10.3748/wjg.v24.i39.4436. [18] KIM MN, LEE JH, CHON YE, et al. Fibrosis-4, aspartate transaminase-to-platelet ratio index, and gamma-glutamyl transpeptidase-to-platelet ratio for risk assessment of hepatocellular carcinoma in chronic hepatitis B patients: Comparison with liver biopsy[J]. Eur J Gastroenterol Hepatol, 2020, 32( 3): 433- 439. DOI: 10.1097/MEG.0000000000001520. [19] XU XL, JIANG LS, WU CS, et al. The role of fibrosis index FIB-4 in predicting liver fibrosis stage and clinical prognosis: A diagnostic or screening tool?[J]. J Formos Med Assoc, 2022, 121( 2): 454- 466. DOI: 10.1016/j.jfma.2021.07.013. [20] ZHANG Y, WANG R, YANG XJ. FIB-4 index serves as a noninvasive prognostic biomarker in patients with hepatocellular carcinoma: A meta-analysis[J]. Medicine, 2018, 97( 51): e13696. DOI: 10.1097/MD.0000000000013696. [21] EDITORS PLOS ONE. Retraction: The prognostic value of prognostic nutritional index in hepatocellular carcinoma patients: A meta-analysis of observational studies[J]. PLoS One, 2022, 17( 8): e0273618. DOI: 10.1371/journal.pone.0273618. [22] NAJAFI M, FARHOOD B, MORTEZAEE K. Contribution of regulatory T cells to cancer: A review[J]. J Cell Physiol, 2019, 234( 6): 7983- 7993. DOI: 10.1002/jcp.27553. [23] CHEN Y, YANG Y, ZHANG XY, et al. Nomogram based on neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio to predict recurrence in patients with hepatocellular carcinoma after radiofrequency ablation[J]. Cardiovasc Intervent Radiol, 2021, 44( 10): 1551- 1560. DOI: 10.1007/s00270-021-02872-8. [24] ZHANG CY, LIU S, YANG M. Hepatocellular carcinoma and obesity, type 2 diabetes mellitus, cardiovascular disease: Causing factors, molecular links, and treatment options[J]. Front Endocrinol, 2021, 12: 808526. DOI: 10.3389/fendo.2021.808526. [25] PEARSON-STUTTARD J, PAPADIMITRIOU N, MARKOZANNES G, et al. Type 2 diabetes and cancer: An umbrella review of observational and Mendelian randomization studies[J]. Cancer Epidemiol Biomarkers Prev, 2021, 30( 6): 1218- 1228. DOI: 10.1158/1055-9965.EPI-20-1245. [26] XU XF, XING H, HAN J, et al. Risk factors, patterns, and outcomes of late recurrence after liver resection for hepatocellular carcinoma: A multicenter study from China[J]. JAMA Surg, 2019, 154( 3): 209- 217. DOI: 10.1001/jamasurg.2018.4334. [27] LEE HA, LEE YS, KIM BK, et al. Change in the recurrence pattern and predictors over time after complete cure of hepatocellular carcinoma[J]. Gut Liver, 2021, 15( 3): 420- 429. DOI: 10.5009/gnl20101. -



 PDF下载 ( 1118 KB)
PDF下载 ( 1118 KB)

 下载:
下载: