非酒精性脂肪性肝病与肌少症双向关系的新见解与展望
DOI: 10.3969/j.issn.1001-5256.2023.11.025
利益冲突声明:本文不存在任何利益冲突。
作者贡献声明:冯巩、任艺琳、吴天悦、张佳怡负责资料分析,撰写论文;冯巩、马永红、闫晓妮、宋娟娟参与文献检索,修改论文;冯巩、弥曼、李雪萍负责拟定写作思路,指导撰写文章并最后定稿。
Bidirectional relationship between nonalcoholic fatty liver disease and sarcopenia: New insights and perspectives
-
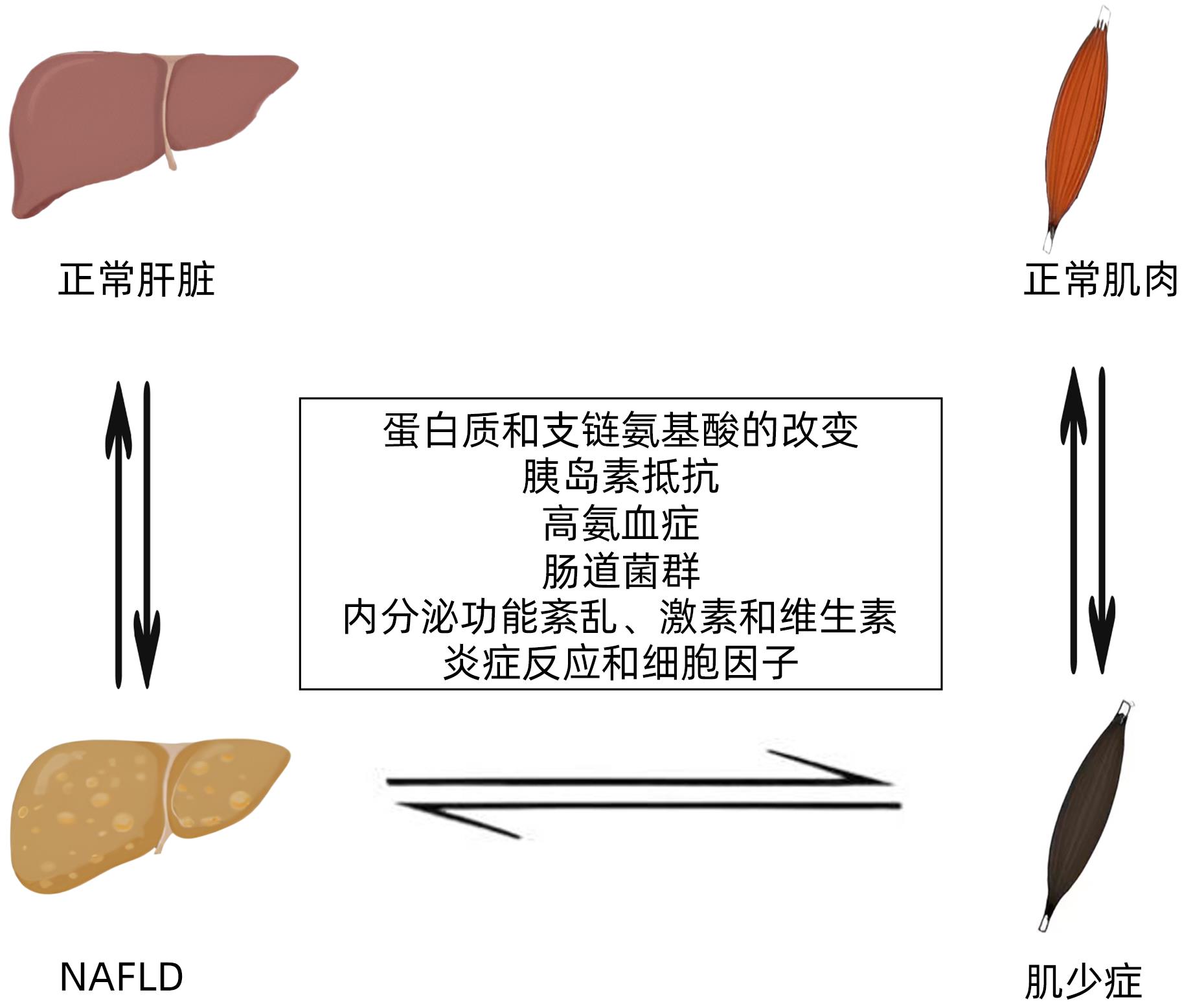
摘要: 非酒精性脂肪性肝病(NAFLD)是一组高度异质性疾病,与代谢功能障碍密切相关。肌少症是指肌肉质量、强度和功能持续下降引起的综合征,与NAFLD常伴随出现。胰岛素抵抗是引起肌少症和NAFLD的主要病理机制,此外还有蛋白质和支链氨基酸的改变、高氨血症、肠道菌群、内分泌功能紊乱等因素也会共同导致肌少症和NAFLD。随着临床研究的不断深入,不少已发表的前瞻性研究文章已证实肌少症与NAFLD之间在病理生理上存在双向且复杂的关系。本文主要梳理了肌少症与NAFLD之间的双向关系,并在此基础上讨论了肌少症与NAFLD的共同发病机制,总结了本领域面临的挑战,为未来NAFLD与肌少症的双向关系研究提出了新的方向。Abstract: Nonalcoholic fatty liver disease (NAFLD) is a group of highly heterogeneous diseases closely associated with metabolic dysfunction. Sarcopenia is a syndrome caused by a continuous decline in muscle mass, strength, and function, and it is often accompanied by NAFLD. Insulin resistance is the main pathological mechanism for sarcopenia and NAFLD, and in addition, factors such as changes in proteins and branched-chain amino acid, hyperammonemia, intestinal flora, and endocrine dysfunction can also lead to sarcopenia and NAFLD. With the deepening of clinical research, many published prospective studies have confirmed the existence of a bidirectional and complex pathophysiological relationship between sarcopenia and NAFLD. This article reviews the bidirectional relationship between sarcopenia and NAFLD, discusses the common pathogenesis of sarcopenia and NAFLD, summarizes the challenges faced in this field, and proposes new directions for the research on the bidirectional relationship between NAFLD and sarcopenia.
-
Key words:
- Sarcopenia /
- Non-alcoholic Fatty Liver Disease /
- Therapeutics
-
[1] WANG CE, XU WT, GONG J, et al. Research progress in the treatment of non-alcoholic fatty liver disease[J]. Clin J Med Offic, 2022, 50( 9): 897- 899, 903. DOI: 10.16680/j.1671-3826.2022.09.06.王彩娥, 许文涛, 宫建, 等. 非酒精性脂肪性肝病治疗研究进展[J]. 临床军医杂志, 2022, 50( 9): 897- 899, 903. DOI: 10.16680/j.1671-3826.2022.09.06. [2] SUN C, FAN JG. Characteristics and prevention strategies of patients with non-alcoholic fatty liver disease combined with sarcopenia[J]. Chin J Gastroenterol Hepatol, 2020, 29( 8): 841 -845. DOI: 10.3969/j.issn.1006-5709.2020.08.001.孙超, 范建高. 非酒精性脂肪性肝病合并肌少症患者的特征和防治策略[J]. 胃肠病学和肝病学杂志, 2020, 29( 8): 841- 845. DOI: 10.3969/j.issn.1006-5709.2020.08.001. [3] YOUNOSSI ZM, KOENIG AB, ABDELATIF D, et al. Global epidemidogy of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes[J]. Hepatology, 2016, 64( 1): 73- 84. DOI: 10.1002/hep.28431. [4] LI J, ZOU B, YEO YH, et al. Prevalence, incidence, and outcome of non-alcoholic fatty liver disease in Asia, 1999-2019: a systematic review and meta-analysis[J]. Lancet Gastroenterol Hepatol, 2019, 4( 5): 389- 398. DOI: 10.1016/S2468-1253(19)30039-1. [5] JOO SK, KIM W. Interaction between sarcopenia and nonalcoholic fatty liver disease[J]. Clin Mol Hepatol, 2023, 29( Suppl): S68- S78. DOI: 10.3350/cmh.2022.0358. [6] IANNUZZI-SUCICH M, PRESTWOOD KM, KENNY AM. Prevalence of sarcopenia and predictors of skeletal muscle mass in healthy, older men and women[J]. J Gerontol A Biol Sci Med Sci, 2002, 57( 12): M772- M777. DOI: 10.1093/gerona/57.12.m772. [7] POUWELS S, SAKRAN N, GRAHAM Y, et al. Non-alcoholic fatty liver disease(NAFLD): a review of pathophysiology, clinical management and effects of weight loss[J]. BMC Endocr Disord, 2022, 22( 1): 63. DOI: 10.1186/s12902-022-00980-1. [8] PÁR A, HEGYI JP, VÁNCSA S, et al. Sarcopenia-2021: Pathophysiology, diagnosis, therapy[J]. Orv Hetil, 2021, 162( 1): 3- 12. DOI: 10.1556/650.2021.32015. [9] CHOE EK, KANG HY, PARK B, et al. The association between nonalcoholic fatty liver disease and CT-measured skeletal muscle mass[J]. J Clin Med, 2018, 7( 10): 310. DOI: 10.3390/jcm7100310. [10] HONG HC, HWANG SY, CHOI HY, et al. Relationship between sarcopenia and nonalcoholic fatty liver disease: the Korean Sarcopenic Obesity Study[J]. Hepatology, 2014, 59( 5): 1772- 1778. DOI: 10.1002/hep.26716. [11] LEE YH, JUNG KS, KIM SU, et al. Sarcopaenia is associated with NAFLD independently of obesity and insulin resistance: Nationwide surveys(KNHANES 2008-2011)[J]. J Hepatol, 2015, 63( 2): 486- 493. DOI: 10.1016/j.jhep.2015.02.051. [12] LEE YH, KIM SU, SONG K, et al. Sarcopenia is associated with significant liver fibrosis independently of obesity and insulin resistance in nonalcoholic fatty liver disease: Nationwide surveys(KNHANES 2008-2011)[J]. Hepatology, 2016, 63( 3): 776- 786. DOI: 10.1002/hep.28376. [13] KIM HY, KIM CW, PARK CH, et al. Low skeletal muscle mass is associated with non-alcoholic fatty liver disease in Korean adults: the Fifth Korea National Health and Nutrition Examination Survey[J]. Hepatobiliary Pancreat Dis Int, 2016, 15( 1): 39- 47. DOI: 10.1016/s1499-3872(15)60030-3. [14] KOO BK, KIM D, JOO SK, et al. Sarcopenia is an independent risk factor for non-alcoholic steatohepatitis and significant fibrosis[J]. J Hepatol, 2017, 66( 1): 123- 131. DOI: 10.1016/j.jhep.2016.08.019. [15] PETTA S, CIMINNISI S, DI MARCO V, et al. Sarcopenia is associated with severe liver fibrosis in patients with non-alcoholic fatty liver disease[J]. Aliment Pharmacol Ther, 2017, 45( 4): 510- 518. DOI: 10.1111/apt.13889. [16] WIJARNPREECHA K, KIM D, RAYMOND P, et al. Associations between sarcopenia and nonalcoholic fatty liver disease and advanced fibrosis in the USA[J]. Eur J Gastroenterol Hepatol, 2019, 31( 9): 1121- 1128. DOI: 10.1097/MEG.0000000000001397. [17] KIM G, LEE SE, LEE YB, et al. Relationship between relative skeletal muscle mass and nonalcoholic fatty liver disease: A 7-year longitudinal study[J]. Hepatology, 2018, 68( 5): 1755- 1768. DOI: 10.1002/hep.30049. [18] HSIEH YC, JOO SK, KOO BK, et al. Myosteatosis, but not sarcopenia, predisposes NAFLD subjects to early steatohepatitis and fibrosis progression[J]. Clin Gastroenterol Hepatol, 2023, 21( 2): 388- 397. e 10. DOI: 10.1016/j.cgh.2022.01.020. [19] ISSA D, ALKHOURI N, TSIEN C, et al. Presence of sarcopenia(muscle wasting) in patients with nonalcoholic steatohepatitis[J]. Hepatology, 2014, 60( 1): 428- 429. DOI: 10.1002/hep.26908. [20] SINN DH, KANG D, KANG M, et al. Nonalcoholic fatty liver disease and accelerated loss of skeletal muscle mass: A longitudinal cohort study[J]. Hepatology, 2022, 76( 6): 1746- 1754. DOI: 10.1002/hep.32578. [21] ROH E, HWANG SY, YOO HJ, et al. Impact of non-alcoholic fatty liver disease on the risk of sarcopenia: a nationwide multicenter prospective study[J]. Hepatol Int, 2022, 16( 3): 545- 554. DOI: 10.1007/s12072-021-10258-8. [22] CANNATARO R, CARBONE L, PETRO JL, et al. Sarcopenia: etiology, nutritional approaches, and miRNAs[J]. Int J Mol Sci, 2021, 22( 18): 9724. DOI: 10.3390/ijms22189724. [23] NASSIR F. NAFLD: mechanisms, treatments, and biomarkers[J]. Biomolecules, 2022, 12( 6): 824. DOI: 10.3390/biom12060824. [24] BREEN L, PHILLIPS SM. Skeletal muscle protein metabolism in the elderly: Interventions to counteract the‘anabolic resistance’ of ageing[J]. Nutr Metab(Lond), 2011, 8: 68. DOI: 10.1186/1743-7075-8-68. [25] KAMIMURA H, SATO T, NATSUI K, et al. Molecular mechanisms and treatment of sarcopenia in liver disease: a review of current knowledge[J]. Int J Mol Sci, 2021, 22( 3): 1425. DOI: 10.3390/ijms22031425. [26] NEINAST M, MURASHIGE D, ARANY Z. Branched chain amino acids[J]. Annu Rev Physiol, 2019, 81: 139- 164. DOI: 10.1146/annurev-physiol-020518-114455. [27] MASTROTOTARO L, RODEN M. Insulin resistance and insulin sensitizing agents[J]. Metabolism, 2021, 125: 154892. DOI: 10.1016/j.metabol.2021.154892. [28] RINALDI L, PAFUNDI PC, GALIERO R, et al. Mechanisms of non-alcoholic fatty liver disease in the metabolic syndrome. a narrative review[J]. Antioxidants(Basel), 2021, 10( 2): 270. DOI: 10.3390/antiox10020270. [29] LANG T, STREEPER T, CAWTHON P, et al. Sarcopenia: etiology, clinical consequences, intervention, and assessment[J]. Osteoporos Int, 2010, 21( 4): 543- 559. DOI: 10.1007/s00198-009-1059-y. [30] ZENG WL, WANG Y. Advances in ammonia lowering therapy for hepatic encephalopathy[J]. Liver, 2022, 27( 6): 622- 624. DOI: 10.14000/j.cnki.issn.1008-1704.2022.06.028.曾伟兰, 汪艳. 肝性脑病降氨治疗进展[J]. 肝脏, 2022, 27( 6): 622- 624. DOI: 10.14000/j.cnki.issn.1008-1704.2022.06.028. [31] QIU J, THAPALIYA S, RUNKANA A, et al. Hyperammonemia in cirrhosis induces transcriptional regulation of myostatin by an NF-κB-mediated mechanism[J]. Proc Natl Acad Sci U S A, 2013, 110( 45): 18162- 18167. DOI: 10.1073/pnas.1317049110. [32] OWEN OE, KALHAN SC, HANSON RW. The key role of anaplerosis and cataplerosis for citric acid cycle function[J]. J Biol Chem, 2002, 277( 34): 30409- 30412. DOI: 10.1074/jbc.R200006200. [33] ROMBOUTS K, MARRA F. Molecular mechanisms of hepatic fibrosis in non-alcoholic steatohepatitis[J]. Dig Dis, 2010, 28( 1): 229- 235. DOI: 10.1159/000282094. [34] WANG ZX, FAN JG. Relationships and mechanisms of sarcopenia and nonalcoholic fatty liver disease[J]. Int J Dig Dis, 2021, 41( 2): 88- 91, 107. DOI: 10.3969/j.issn.1673-534X.2021.02.004.王子璇, 范建高. 肌少症与非酒精性脂肪性肝病的关系及机制[J]. 国际消化病杂志, 2021, 41( 2): 88- 91, 107. DOI: 10.3969/j.issn.1673-534X.2021.02.004. [35] MIELE L, VALENZA V, LA TORRE G, et al. Increased intestinal permeability and tight junction alterations in nonalcoholic fatty liver disease[J]. Hepatology, 2009, 49( 6): 1877- 1887. DOI: 10.1002/hep.22848. [36] TRIPATHI A, DEBELIUS J, BRENNER DA, et al. The gut-liver axis and the intersection with the microbiome[J]. Nat Rev Gastroenterol Hepatol, 2018, 15( 7): 397- 411. DOI: 10.1038/s41575-018-0011-z. [37] SARKAR M, YATES K, SUZUKI A, et al. Low testosterone is associated with nonalcoholic steatohepatitis and fibrosis severity in men[J]. Clin Gastroenterol Hepatol, 2021, 19( 2): 400- 402. e 2. DOI: 10.1016/j.cgh.2019.11.053. [38] KUMAR R, PRAKASH SS, PRIYADARSHI RN, et al. Sarcopenia in chronic liver disease: a metabolic perspective[J]. J Clin Transl Hepatol, 2022, 10( 6): 1213- 1222. DOI: 10.14218/JCTH.2022.00239. [39] DASARATHY S. Is the adiponectin-AMPK-mitochondrial axis involved in progression of nonalcoholic fatty liver disease?[J]. Hepatology, 2014, 60( 1): 22- 25. DOI: 10.1002/hep.27134. [40] LI H, LIU DG, YAN SQ, et al. Improvement effect of 1,25(OH)2D3 combined with astragalus polysaccharide on insulin resistance of skeletal muscle cells in vitro and its mechanism[J]. J Jilin Univ(Med Edit), 2022, 48( 6): 1411- 1421. DOI: 10.13481/j.1671-587X.20220606.李浩, 刘东阁, 闫姝琪, 等. 1,25(OH)2D3联合黄芪多糖对体外骨骼肌细胞胰岛素抵抗的改善作用及其机制[J]. 吉林大学学报(医学版), 2022, 48( 6): 1411- 1421. DOI: 10.13481/j.1671-587X.20220606. [41] XIE Y, LIANG ZR, WANG J. Advances in research on the relationship between nonalcoholic fatty liver disease and vitamin D[J]. Transl Med J, 2021, 10( 5): 343- 346. DOI: 10.3969/j.issn.2095-3097.2021.05.015.谢艳, 梁子荣, 王钧. 非酒精性脂肪性肝病与维生素D关系研究进展[J]. 转化医学杂志, 2021, 10( 5): 343- 346. DOI: 10.3969/j.issn.2095-3097.2021.05.015. [42] HAMRICK MW. Role of the cytokine-like hormone leptin in muscle-bone crosstalk with aging[J]. J Bone Metab, 2017, 24( 1): 1- 8. DOI: 10.11005/jbm.2017.24.1.1. [43] YI Y, WANG C, DING Y, et al. Diet was less significant than physical activity in the prognosis of people with sarcopenia and metabolic dysfunction-associated fatty liver diseases: Analysis of the national health and nutrition examination survey III[J]. Front Endocrinol(Lausanne), 2023, 14: 1101892. DOI: 10.3389/fendo.2023.1101892. [44] PASCO JA, WILLIAMS LJ, JACKA FN, et al. Sarcopenia and the common mental disorders: a potential regulatory role of skeletal muscle on brain function?[J]. Curr Osteoporos Rep, 2015, 13( 5): 351- 357. DOI: 10.1007/s11914-015-0279-7. [45] SUBRAMANIAN M, WOJTUSCISZYN A, FAVRE L, et al. Precision medicine in the era of artificial intelligence: implications in chronic disease management[J]. J Transl Med, 2020, 18( 1): 472. DOI: 10.1186/s12967-020-02658-5. [46] FENG G, WANG XY, LI SS, et al. Application of artificial intelligence and machine learning in nonalcoholic fatty liver disease[J]. J Clin Hepatol, 2022, 38( 10): 2352- 2356. DOI: 10.3969/j.issn.1001-5256.2022.10.029.冯巩, 王雪莹, 李珊珊, 等. 人工智能及机器学习在非酒精性脂肪性肝病中的应用[J]. 临床肝胆病杂志, 2022, 38( 10): 2352- 2356. DOI: 10.3969/j.issn.1001-5256.2022.10.029. -



 PDF下载 ( 728 KB)
PDF下载 ( 728 KB)

 下载:
下载:


