肠-肝轴:肠道微生物稳态与肝细胞癌
DOI: 10.3969/j.issn.1001-5256.2023.11.029
利益冲突声明:本文不存在任何利益冲突。
作者贡献声明:周荃负责拟定写作思路,检索文献,撰写及修改论文;李金强、蔡春琳负责指导,最终定稿。
-
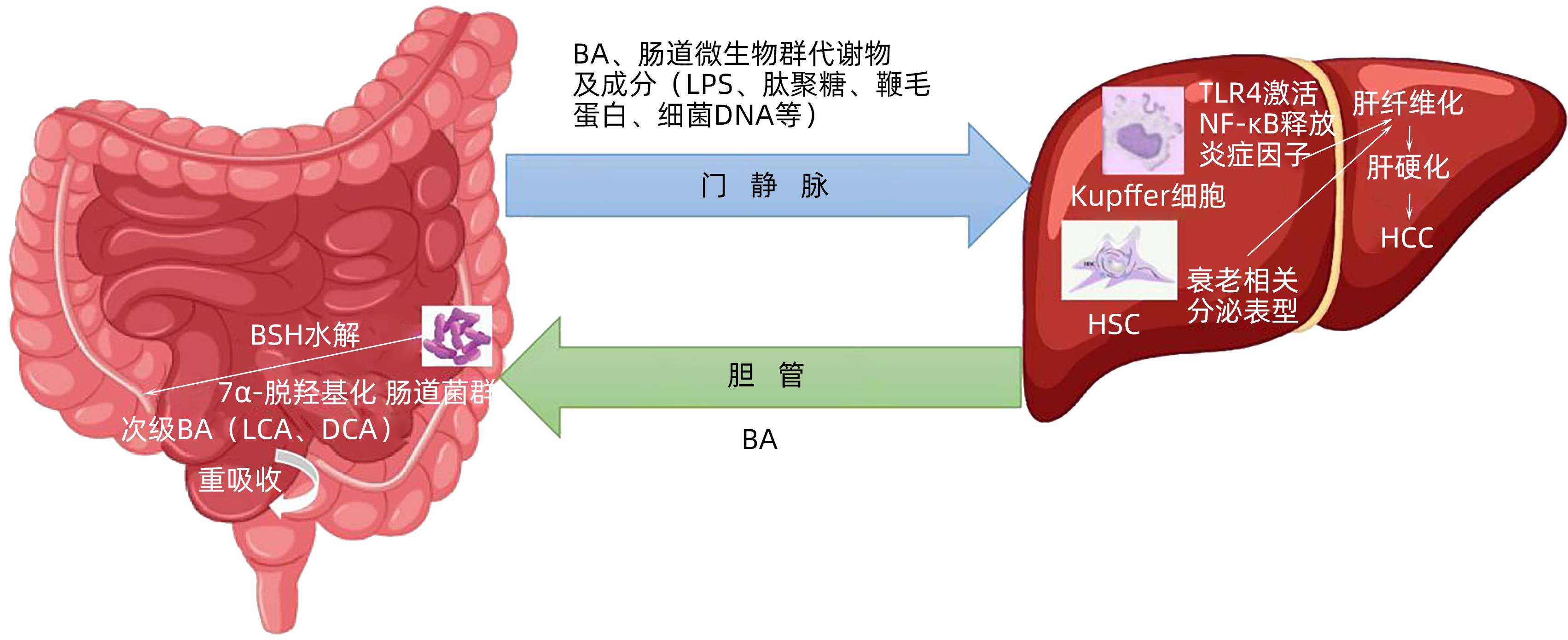
摘要: 肠道微生物群在维持肝脏代谢稳态中扮演重要角色,其通过参与胆汁酸代谢影响肝细胞癌的发生发展。“肠-肝轴”在肝脏疾病发病机制中占据举足轻重的地位,通过纠正肠道生态失衡以恢复正常胆汁酸水平,可能是阻止肝细胞癌进展的有效方法之一。本文总结了胆汁酸受体影响肝细胞癌的相关机制以及最新治疗靶点,旨在为早期防治肝癌提供参考依据。Abstract: Intestinal microbiota plays an important role in maintaining liver metabolic homeostasis and affects the development and progression of hepatocellular carcinoma by participating in bile acid metabolism. Gut-liver axis plays an important role in the pathogenesis of liver diseases, and it might be one of the effective methods to prevent the progression of hepatocellular carcinoma by correcting intestinal ecological imbalance to restore normal bile acid level. This article summarizes the mechanism of bile acid receptor affecting hepatocellular carcinoma and the latest therapeutic targets, in order to provide a reference for the early prevention and treatment of hepatocellular carcinoma.
-
[1] WANG GQ, JIANG Y, LU CD, et al. CircFOXM1 promotes proliferation and metastasis of hepatocellular carcinoma via regulating miR-1179/SPAG5 axis[J]. Sci Rep, 2021, 11( 1): 23890. DOI: 10.1038/s41598-021-03285-w. [2] COSTANTE F, AIROLA C, SANTOPAOLO F, et al. Immunotherapy for nonalcoholic fatty liver disease-related hepatocellular carcinoma: Lights and shadows[J]. World J Gastrointest Oncol, 2022, 14( 9): 1622- 1636. DOI: 10.4251/wjgo.v14.i9.1622. [3] WU LW, FENG J, LI JJ, et al. The gut microbiome-bile acid axis in hepatocarcinogenesis[J]. Biomed Pharmacother, 2021, 133: 111036. DOI: 10.1016/j.biopha.2020.111036. [4] CHIANG JYL, FERRELL JM. Bile acid metabolism in liver pathobiology[J]. Gene Expr, 2018, 18( 2): 71- 87. DOI: 10.3727/105221618X15156018385515. [5] GUPTA H, YOUN GS, SHIN MJ, et al. Role of gut microbiota in hepatocarcinogenesis[J]. Microorganisms, 2019, 7( 5): 121. DOI: 10.3390/microorganisms7050121. [6] SCHNEIDER KM, MOHS A, GUI WF, et al. Imbalanced gut microbiota fuels hepatocellular carcinoma development by shaping the hepatic inflammatory microenvironment[J]. Nat Commun, 2022, 13( 1): 3964. DOI: 10.1038/s41467-022-31312-5. [7] ZHANG R, MA WQ, FU MJ, et al. Overview of bile acid signaling in the cardiovascular system[J]. World J Clin Cases, 2021, 9( 2): 308- 320. DOI: 10.12998/wjcc.v9.i2.308. [8] CHEN MJ, LIU C, WAN Y, et al. Enterohepatic circulation of bile acids and their emerging roles on glucolipid metabolism[J]. Steroids, 2021, 165: 108757. DOI: 10.1016/j.steroids.2020.108757. [9] DONG SJ, ZHU M, WANG K, et al. Dihydromyricetin improves DSS-induced colitis in mice via modulation of fecal-bacteria-related bile acid metabolism[J]. Pharmacol Res, 2021, 171: 105767. DOI: 10.1016/j.phrs.2021.105767. [10] GRÜNER N, MATTNER J. Bile acids and microbiota: Multifaceted and versatile regulators of the liver-gut axis[J]. Int J Mol Sci, 2021, 22( 3): 1397. DOI: 10.3390/ijms22031397. [11] MOHAMADKHANI A. On the potential role of intestinal microbial community in hepatocarcinogenesis in chronic hepatitis B[J]. Cancer Med, 2018, 7( 7): 3095- 3100. DOI: 10.1002/cam4.1550. [12] SONG I, GOTOH Y, OGURA Y, et al. Comparative genomic and physiological analysis against Clostridium scindens reveals Eubacterium sp. c-25 as an atypical deoxycholic acid producer of the human gut microbiota[J]. Microorganisms, 2021, 9( 11): 2254. DOI: 10.3390/microorganisms9112254. [13] ZENG HW, UMAR S, RUST B, et al. Secondary bile acids and short chain fatty acids in the colon: A focus on colonic microbiome, cell proliferation, inflammation, and cancer[J]. Int J Mol Sci, 2019, 20( 5): 1214. DOI: 10.3390/ijms20051214. [14] LIU P, TANG QH, CHEN MM, et al. Hepatocellular senescence: Immunosurveillance and future senescence-induced therapy in hepatocellular carcinoma[J]. Front Oncol, 2020, 10: 589908. DOI: 10.3389/fonc.2020.589908. [15] GENG SJ, CHENG SS, LI Y, et al. Faecal microbiota transplantation reduces susceptibility to epithelial injury and modulates tryptophan metabolism of the microbial community in a piglet model[J]. J Crohns Colitis, 2018, 12( 11): 1359- 1374. DOI: 10.1093/ecco-jcc/jjy103. [16] SEBŐK C, TRÁJ P, VÖRÖSHÁZI J, et al. Two sides to every question: Attempts to activate chicken innate immunity in 2D and 3D hepatic cell cultures[J]. Cells, 2021, 10( 8): 1910. DOI: 10.3390/cells10081910. [17] ZHANG WJ, LI KY, HUANG BH, et al. The hepatocyte in the innate immunity[J]. Virology, 2022, 576: 111- 116. DOI: 10.1016/j.virol.2022.09.011. [18] CHEN SN, TAN Y, XIAO XC, et al. Deletion of TLR4 attenuates lipopolysaccharide-induced acute liver injury by inhibiting inflammation and apoptosis[J]. Acta Pharmacol Sin, 2021, 42( 10): 1610- 1619. DOI: 10.1038/s41401-020-00597-x. [19] GAO B, AHMAD MF, NAGY LE, et al. Inflammatory pathways in alcoholic steatohepatitis[J]. J Hepatol, 2019, 70( 2): 249- 259. DOI: 10.1016/j.jhep.2018.10.023. [20] WANG SC, CHEN YC, CHEN SJ, et al. Alcohol addiction, gut microbiota, and alcoholism treatment: A review[J]. Int J Mol Sci, 2020, 21( 17): 6413. DOI: 10.3390/ijms21176413. [21] ROHR MW, NARASIMHULU CA, RUDESKI-ROHR TA, et al. Negative effects of a high-fat diet on intestinal permeability: A review[J]. Adv Nutr, 2020, 11( 1): 77- 91. DOI: 10.1093/advances/nmz061. [22] MALESZA IJ, MALESZA M, WALKOWIAK J, et al. High-fat, western-style diet, systemic inflammation, and gut microbiota: A narrative review[J]. Cells, 2021, 10( 11): 3164. DOI: 10.3390/cells10113164. [23] GILLARD J, CLERBAUX LA, NACHIT M, et al. Bile acids contribute to the development of non-alcoholic steatohepatitis in mice[J]. JHEP Rep, 2021, 4( 1): 100387. DOI: 10.1016/j.jhepr.2021.100387. [24] BEYOĞLU D, IDLE JR. The gut microbiota- A vehicle for the prevention and treatment of hepatocellular carcinoma[J]. Biochem Pharmacol, 2022, 204: 115225. DOI: 10.1016/j.bcp.2022.115225. [25] XUE R, SU LY, LAI SY, et al. Bile acid receptors and the gut-liver axis in nonalcoholic fatty liver disease[J]. Cells, 2021, 10( 11): 2806. DOI: 10.3390/cells10112806. [26] WANG TY, WEI W, ZHONG H, et al. Progress on the treatment of metabolic dysfunction-associated fatty liver disease by farnesol X receptor agonist[J/CD]. Chin J Liver Dis Electron Version, 2023, 15( 1): 6- 11. DOI: 10.3969/j.issn.1674-7380.2023.01.002.王霆宇, 魏尉, 钟黄, 等. 法尼醇X受体激动剂对非酒精性脂肪性肝炎治疗作用研究进展[J/CD]. 中国肝脏病杂志(电子版), 2023, 15( 1): 6- 11. DOI: 10.3969/j.issn.1674-7380.2023.01.002. [27] LI YQ, TIAN YY, CAI WZ, et al. Novel ι-carrageenan tetrasaccharide alleviates liver lipid accumulation via the bile acid-FXR-SHP/PXR pathway to regulate cholesterol conversion and fatty acid metabolism in insulin-resistant mice[J]. J Agric Food Chem, 2021, 69( 34): 9813- 9821. DOI: 10.1021/acs.jafc.1c04035. [28] HARTMANN P, HOCHRATH K, HORVATH A, et al. Modulation of the intestinal bile acid/farnesoid X receptor/fibroblast growth factor 15 axis improves alcoholic liver disease in mice[J]. Hepatology, 2018, 67( 6): 2150- 2166. DOI: 10.1002/hep.29676. [29] ZHONG XC, LIU YM, GAO XX, et al. Caffeic acid phenethyl ester suppresses intestinal FXR signaling and ameliorates nonalcoholic fatty liver disease by inhibiting bacterial bile salt hydrolase activity[J]. Acta Pharmacol Sin, 2023, 44( 1): 145- 156. DOI: 10.1038/s41401-022-00921-7. [30] IRACHETA-VELLVE A, CALENDA CD, PETRASEK J, et al. FXR and TGR5 agonists ameliorate liver injury, steatosis, and inflammation after binge or prolonged alcohol feeding in mice[J]. Hepatol Commun, 2018, 2( 11): 1379- 1391. DOI: 10.1002/hep4.1256. [31] SHAPIRO H, KOLODZIEJCZYK AA, HALSTUCH D, et al. Bile acids in glucose metabolism in health and disease[J]. J Exp Med, 2018, 215( 2): 383- 396. DOI: 10.1084/jem.20171965. [32] JIA W, XIE GX, JIA WP. Bile acid-microbiota crosstalk in gastrointestinal inflammation and carcinogenesis[J]. Nat Rev Gastroenterol Hepatol, 2018, 15( 2): 111- 128. DOI: 10.1038/nrgastro.2017.119. [33] LI CL, LIN YK, CHEN HA, et al. Smoking as an independent risk factor for hepatocellular carcinoma due to the α7-nachr modulating the JAK2/STAT3 signaling axis[J]. J Clin Med, 2019, 8( 9): 1391. DOI: 10.3390/jcm8091391. [34] SPATZ M, CIOCAN D, MERLEN G, et al. Bile acid-receptor TGR5 deficiency worsens liver injury in alcohol-fed mice by inducing intestinal microbiota dysbiosis[J]. JHEP Rep, 2021, 3( 2): 100230. DOI: 10.1016/j.jhepr.2021.100230. [35] ZHANG GH, LIU MJ, SONG M, et al. Patchouli alcohol activates PXR and suppresses the NF-κB-mediated intestinal inflammatory[J]. J Ethnopharmacol, 2020, 248: 112302. DOI: 10.1016/j.jep.2019.112302. [36] SHIN DJ, WANG L. Bile acid-activated receptors: A review on FXR and other nuclear receptors[J]. Handb Exp Pharmacol, 2019, 256: 51- 72. DOI: 10.1007/164_2019_236. [37] LIU X, WANG Y. An overview of bile acid synthesis and its physiological and pathological functions[J]. Hereditas, 2019, 41( 5): 365- 374. DOI: 10.16288/j.yczz.19-011.刘笑, 王琰. 胆汁酸的合成调控及其在生理与病理中的功能机制[J]. 遗传, 2019, 41( 5): 365- 374. DOI: 10.16288/j.yczz.19-011. [38] LIU L, PANZITT K, RACEDO S, et al. Bile acids increase steroidogenesis in cholemic mice and induce cortisol secretion in adrenocortical H295R cells via S1PR2, ERK and SF-1[J]. Liver Int, 2019, 39( 11): 2112- 2123. DOI: 10.1111/liv.14052. [39] KWONG EK, ZHOU HP. Sphingosine-1-phosphate signaling and the gut-liver axis in liver diseases[J]. Liver Res, 2019, 3( 1): 19- 24. DOI: 10.1016/j.livres.2019.02.003. [40] GOETTEL M, FEGERT I, HONARVAR N, et al. Comparative studies on the effects of sodium phenobarbital and two other constitutive androstane receptor(CAR) activators on induction of cytochrome P450 enzymes and replicative DNA synthesis in cultured hepatocytes from wild type and CAR knockout rats[J]. Toxicology, 2020, 433-434: 152394. DOI: 10.1016/j.tox.2020.152394. [41] NOH K, CHOW ECY, QUACH HP, et al. Significance of the vitamin D receptor on crosstalk with nuclear receptors and regulation of enzymes and transporters[J]. AAPS J, 2022, 24( 4): 71. DOI: 10.1208/s12248-022-00719-9. [42] QIN X, WANG X. Role of vitamin D receptor in the regulation of CYP3A gene expression[J]. Acta Pharm Sin B, 2019, 9( 6): 1087- 1098. DOI: 10.1016/j.apsb.2019.03.005. [43] DONG BN, ZHOU Y, WANG W, et al. Vitamin D receptor activation in liver macrophages ameliorates hepatic inflammation, steatosis, and insulin resistance in mice[J]. Hepatology, 2020, 71( 5): 1559- 1574. DOI: 10.1002/hep.30937. [44] ŠARENAC TM, MIKOV M. Bile acid synthesis: From nature to the chemical modification and synthesis and their applications as drugs and nutrients[J]. Front Pharmacol, 2018, 9: 939. DOI: 10.3389/fphar.2018.00939. [45] FUKUI H. Role of gut dysbiosis in liver diseases: What have we learned so far?[J]. Diseases, 2019, 7( 4): 58. DOI: 10.3390/diseases7040058. [46] LIU YH, CHEN KF, LI FY, et al. Probiotic Lactobacillus rhamnosus GG prevents liver fibrosis through inhibiting hepatic bile acid synthesis and enhancing bile acid excretion in mice[J]. Hepatology, 2020, 71( 6): 2050- 2066. DOI: 10.1002/hep.30975. [47] CHEN QW, LI QR, CAO MW, et al. Hierarchy-assembled dual probiotics system ameliorates cholestatic drug-induced liver injury via gut-liver axis modulation[J]. Adv Sci, 2022, 9( 17): e2200986. DOI: 10.1002/advs.202200986. [48] MENDES KL, DE FARIAS LELIS D, DE FREITAS DF, et al. Acute oral treatment with resveratrol and Lactococcus Lactis Subsp. Lactis decrease body weight and improve liver proinflammatory markers in C57BL/6 mice[J]. Mol Biol Rep, 2021, 48( 2): 1725- 1734. DOI: 10.1007/s11033-021-06190-7. [49] GUERRERO-ENCINAS I, GONZÁLEZ-GONZÁLEZ JN, SANTIAGO-LÓPEZ L, et al. Protective effect of Lacticaseibacillus casei CRL 431 postbiotics on mitochondrial function and oxidative status in rats with aflatoxin B1-induced oxidative stress[J]. Probiotics Antimicrob Proteins, 2021, 13( 4): 1033- 1043. DOI: 10.1007/s12602-021-09747-x. [50] HUANG L, ZHAO ZJ, DUAN CC, et al. Lactobacillus plantarum C88 protects against aflatoxin B1-induced liver injury in mice via inhibition of NF-κB-mediated inflammatory responses and excessive apoptosis[J]. BMC Microbiol, 2019, 19( 1): 170. DOI: 10.1186/s12866-019-1525-4. [51] DUAN RX, ZHAO YF, YE YJ, et al. Mechanism of action of bile acid metabolism in regulating inflamm atory bowel disease and the research and development of drugs[J]. Chin J Chin Pharmacol Ther, 2022, 27( 10): 1171- 1181. DOI: 10.12092/j.issn.1009-2501.2022.10.012.段睿潇, 赵一帆, 叶永娟, 等. 胆汁酸代谢调节炎症性肠病的作用机制及药物研发[J]. 中国临床药理学与治疗学, 2022, 27( 10): 1171- 1181. DOI: 10.12092/j.issn.1009-2501.2022.10.012. [52] LIU HX, KANG X, YANG XD, et al. Compound probiotic ameliorates acute alcoholic liver disease in mice by modulating gut microbiota and maintaining intestinal barrier[J]. Probiotics Antimicrob Proteins, 2023, 15( 1): 185- 201. DOI: 10.1007/s12602-022-10005-x. [53] KIM ER, PARK JS, KIM JH, et al. A GLP-1/GLP-2 receptor dual agonist to treat NASH: Targeting the gut-liver axis and microbiome[J]. Hepatology, 2022, 75( 6): 1523- 1538. DOI: 10.1002/hep.32235. [54] GAO A, XU YJ, LU SW, et al. Effect of fecal microbiota transplantation on intestinal flora in mice with acute-on-chronic liver failure[J]. J Clin Hepatol, 2021, 37( 6): 1379- 1385. DOI: 10.3969/j.issn.1001-5256.2021.06.031.高安, 徐玉静, 陆圣威, 等. 粪菌移植对慢加急性肝衰竭小鼠模型肠道菌群的影响[J]. 临床肝胆病杂志, 2021, 37( 6): 1379- 1385. DOI: 10.3969/j.issn.1001-5256.2021.06.031. [55] SHARMA A, ROY A, PREMKUMAR M, et al. Fecal microbiota transplantation in alcohol-associated acute-on-chronic liver failure: An open-label clinical trial[J]. Hepatol Int, 2022, 16( 2): 433- 446. DOI: 10.1007/s12072-022-10312-z. [56] KANG SH, LEE YB, LEE JH, et al. Rifaximin treatment is associated with reduced risk of cirrhotic complications and prolonged overall survival in patients experiencing hepatic encephalopathy[J]. Aliment Pharmacol Ther, 2017, 46( 9): 845- 855. DOI: 10.1111/apt.14275. [57] TAJIRI K, SHIMIZU Y. Branched-chain amino acids in liver diseases[J]. Transl Gastroenterol Hepatol, 2018, 3: 47. DOI: 10.21037/tgh.2018.07.06. [58] SIVAK KV, STOSMAN KI, RASSOKHA TA, et al. The effect of TLR4 blockade on some indicators of systemic inflammatory response to Proteus mirabilis LPS in rats[J]. Bull Exp Biol Med, 2020, 169( 6): 795- 797. DOI: 10.1007/s10517-020-04981-9. [59] PARADA E, CASAS AI, PALOMINO-ANTOLIN A, et al. Early toll-like receptor 4 blockade reduces ROS and inflammation triggered by microglial pro-inflammatory phenotype in rodent and human brain ischaemia models[J]. Br J Pharmacol, 2019, 176( 15): 2764- 2779. DOI: 10.1111/bph.14703. [60] HSIEH YC, LEE KC, WU PS, et al. Eritoran attenuates hepatic inflammation and fibrosis in mice with chronic liver injury[J]. Cells, 2021, 10( 6): 1562. DOI: 10.3390/cells10061562. [61] CAO Y, XIAO YT, ZHOU KJ, et al. FXR agonist GW4064 improves liver and intestinal pathology and alters bile acid metabolism in rats undergoing small intestinal resection[J]. Am J Physiol Gastrointest Liver Physiol, 2019, 317( 2): G108- G115. DOI: 10.1152/ajpgi.00356.2017. [62] DENG H, ZHANG B, ZHU B, et al. Research advances in the role of gut microbiota in chronic hepatitis B, chronic hepatitis C, and related liver diseases[J]. J Clin Hepatol, 2022, 38( 5): 1143- 1147. DOI: 10.3969/j.issn.1001-5256.2022.05.035.邓辉, 张斌, 朱彬, 等. 肠道菌群影响慢性乙型肝炎、慢性丙型肝炎及相关肝病的研究进展[J]. 临床肝胆病杂志, 2022, 38( 5): 1143- 1147. DOI: 10.3969/j.issn.1001-5256.2022.05.035. [63] de BOER JF, de VRIES HD, PALMIOTTI A, et al. Cholangiopathy and biliary fibrosis in Cyp2c70-deficient mice are fully reversed by ursodeoxycholic acid[J]. Cell Mol Gastroenterol Hepatol, 2021, 11( 4): 1045- 1069. DOI: 10.1016/j.jcmgh.2020.12.004. [64] ITO K, OKUMURA A, TAKEUCHI JS, et al. Dual agonist of farnesoid X receptor and takeda G protein-coupled receptor 5 inhibits hepatitis B virus infection in vitro and in vivo[J]. Hepatology, 2021, 74( 1): 83- 98. DOI: 10.1002/hep.31712. [65] WANG XX, XIE C, LIBBY AE, et al. The role of FXR and TGR5 in reversing and preventing progression of Western diet-induced hepatic steatosis, inflammation, and fibrosis in mice[J]. J Biol Chem, 2022, 298( 11): 102530. DOI: 10.1016/j.jbc.2022.102530. [66] FANG S, WANG TM, LI YY, et al. Gardenia jasminoides Ellis polysaccharide ameliorates cholestatic liver injury by alleviating gut microbiota dysbiosis and inhibiting the TLR4/NF-κB signaling pathway[J]. Int J Biol Macromol, 2022, 205: 23- 36. DOI: 10.1016/j.ijbiomac.2022.02.056. -



 PDF下载 ( 811 KB)
PDF下载 ( 811 KB)

 下载:
下载:


