| [1] |
HILSCHER MB, SHAH VH. Neutrophil extracellular traps and liver disease[J]. Semin Liver Dis, 2020, 40( 2): 171- 179. DOI: 10.1055/s-0039-3399562. |
| [2] |
LINHARES-LACERDA L, TEMEROZO JR, RIBEIRO-ALVES M, et al. Neutrophil extracellular trap-enriched supernatants carry microRNAs able to modulate TNF-α production by macrophages[J]. Sci Rep, 2020, 10( 1): 2715. DOI: 10.1038/s41598-020-59486-2. |
| [3] |
VARRICCHI G, MODESTINO L, POTO R, et al. Neutrophil extracellular traps and neutrophil-derived mediators as possible biomarkers in bronchial asthma[J]. Clin Exp Med, 2022, 22( 2): 285- 300. DOI: 10.1007/s10238-021-00750-8. |
| [4] |
TABRIZI ZA, KHOSROJERDI A, ASLANI S, et al. Multi-facets of neutrophil extracellular trap in infectious diseases: Moving beyond immunity[J]. Microb Pathog, 2021, 158: 105066. DOI: 10.1016/j.micpath.2021.105066. |
| [5] |
CHAPMAN EA, LYON M, SIMPSON D, et al. Caught in a trap? proteomic analysis of neutrophil extracellular traps in rheumatoid arthritis and systemic lupus erythematosus[J]. Front Immunol, 2019, 10: 423. DOI: 10.3389/fimmu.2019.00423. |
| [6] |
JORCH SK, KUBES P. An emerging role for neutrophil extracellular traps in noninfectious disease[J]. Nat Med, 2017, 23( 3): 279- 287. DOI: 10.1038/nm.4294. |
| [7] |
HELMY KY, KATSCHKE KJ Jr, GORGANI NN, et al. CRIg: a macrophage complement receptor required for phagocytosis of circulating pathogens[J]. Cell, 2006, 124( 5): 915- 927. DOI: 10.1016/j.cell.2005.12.039. |
| [8] |
MEIJENFELDT F, JENNE CN. Netting liver disease: neutrophil extracellular traps in the initiation and exacerbation of liver pathology[J]. Semin Thromb Hemost, 2020, 46( 6): 724- 734. DOI: 10.1055/s-0040-1715474. |
| [9] |
HU S, LIU X, GAO Y, et al. Hepatitis B virus inhibits neutrophil extracellular trap release by modulating reactive oxygen species production and autophagy[J]. J Immunol, 2019, 202( 3): 805- 815. DOI: 10.4049/jimmunol.1800871. |
| [10] |
ZHAN X, WU R, KONG XH, et al. Elevated neutrophil extracellular traps by HBV-mediated S100A9-TLR4/RAGE-ROS cascade facilitate the growth and metastasis of hepatocellular carcinoma[J]. Cancer Commun(Lond), 2023, 43( 2): 225- 245. DOI: 10.1002/cac2.12388. |
| [11] |
|
| [12] |
ARELAKI S, KOLETSA T, SINAKOS E, et al. Neutrophil extracellular traps enriched with IL-1β and IL-17A participate in the hepatic inflammatory process of patients with non-alcoholic steatohepatitis[J]. Virchows Arch, 2022, 481( 3): 455- 465. DOI: 10.1007/s00428-022-03330-7. |
| [13] |
XU L, LIU X, JIA T, et al. Tanshinone IIA ameliorates nonalcoholic steatohepatitis in mice by modulating neutrophil extracellular traps and hepatocyte apoptosis[J]. Evid Based Complement Alternat Med, 2022, 2022: 5769350. DOI: 10.1155/2022/5769350. |
| [14] |
DU J, ZHANG J, CHEN X, et al. Neutrophil extracellular traps induced by pro-inflammatory cytokines enhance procoagulant activity in NASH patients[J]. Clin Res Hepatol Gastroenterol, 2022, 46( 1): 101697. DOI: 10.1016/j.clinre.2021.101697. |
| [15] |
WANG H, ZHANG H, WANG Y, et al. Regulatory T-cell and neutrophil extracellular trap interaction contributes to carcinogenesis in non-alcoholic steatohepatitis[J]. J Hepatol, 2021, 75( 6): 1271- 1283. DOI: 10.1016/j.jhep.2021.07.032. |
| [16] |
ZHANG S, ZHANG Q, WANG F, et al. Hydroxychloroquine inhibiting neutrophil extracellular trap formation alleviates hepatic ischemia/reperfusion injury by blocking TLR9 in mice[J]. Clin Immunol, 2020, 216: 108461. DOI: 10.1016/j.clim.2020.108461. |
| [17] |
WU X, YANG Z, WANG H, et al. High-mobility group box protein-1 induces acute pancreatitis through activation of neutrophil extracellular trap and subsequent production of IL-1β[J]. Life Sci, 2021, 286: 119231. DOI: 10.1016/j.lfs.2021.119231. |
| [18] |
TOHME S, YAZDANI HO, SUD V, et al. Computational analysis supports IL-17A as a central driver of neutrophil extracellular trap-mediated injury in liver ischemia reperfusion[J]. J Immunol, 2019, 202( 1): 268- 277. DOI: 10.4049/jimmunol.1800454. |
| [19] |
HUANG H, TOHME S, AL-KHAFAJI AB, et al. Damage-associated molecular pattern-activated neutrophil extracellular trap exacerbates sterile inflammatory liver injury[J]. Hepatology, 2015, 62( 2): 600- 614. DOI: 10.1002/hep.27841. |
| [20] |
GUO J, AKAHOSHI T, MIZUTA Y, et al. Histidine-rich glycoprotein alleviates liver ischemia/reperfusion injury in mice with nonalcoholic steatohepatitis[J]. Liver Transpl, 2021, 27( 6): 840- 853. DOI: 10.1002/lt.25960. |
| [21] |
ZHANG QG, LING S, LIU J, et al. Effect of neutrophil extracellular snare on ischemia-reperfusion injury and progress of Chinese medicine intervention[J]. J Shanghai Univ Traditional Chin Med, 2018, 32( 3): 97- 102, 108. DOI: 10.16306/j.1008-861x.2018.03.020. 张庆光, 凌霜, 刘俊, 等. 嗜中性粒细胞胞外诱捕网对缺血再灌注损伤的影响及中医药干预研究进展[J]. 上海中医药大学学报, 2018, 32( 3): 97- 102, 108. DOI: 10.16306/j.1008-861x. 2018.03.020.
|
| [22] |
ARUMUGAM S, GIRISH SUBBIAH K, KEMPARAJU K, et al. Neutrophil extracellular traps in acrolein promoted hepatic ischemia reperfusion injury: Therapeutic potential of NOX2 and p38MAPK inhibitors[J]. J Cell Physiol, 2018, 233( 4): 3244- 3261. DOI: 10.1002/jcp.26167. |
| [23] |
LLOVET JM, CASTET F, HEIKENWALDER M, et al. Immunotherapies for hepatocellular carcinoma[J]. Nat Rev Clin Oncol, 2022, 19( 3): 151- 172. DOI: 10.1038/s41571-021-00573-2. |
| [24] |
XIAO Y, CONG M, LI J, et al. Cathepsin C promotes breast cancer lung metastasis by modulating neutrophil infiltration and neutrophil extracellular trap formation[J]. Cancer Cell, 2021, 39( 3): 423- 437. e 7. DOI: 10.1016/j.ccell.2020.12.012. |
| [25] |
ZENLANDER R, HAVERVALL S, MAGNUSSON M, et al. Neutrophil extracellular traps in patients with liver cirrhosis and hepatocellular carcinoma[J]. Sci Rep, 2021, 11( 1): 18025. DOI: 10.1038/s41598-021-97233-3. |
| [26] |
KALTENMEIER CT, YAZDANI H, van der WINDT D, et al. Neutrophil extracellular traps as a novel biomarker to predict recurrence-free and overall survival in patients with primary hepatic malignancies[J]. HPB(Oxford), 2021, 23( 2): 309- 320. DOI: 10.1016/j.hpb.2020.06.012. |
| [27] |
WANG T, ZHOU Y, ZHOU Z, et al. Secreted protease PRSS35 suppresses hepatocellular carcinoma by disabling CXCL2-mediated neutrophil extracellular traps[J]. Nat Commun, 2023, 14( 1): 1513. DOI: 10.1038/s41467-023-37227-z. |
| [28] |
GUAN X, LU Y, ZHU H, et al. The Crosstalk between cancer cells and neutrophils enhances hepatocellular carcinoma metastasis via neutrophil extracellular traps-associated cathepsin G component: a potential therapeutic target[J]. J Hepatocell Carcinoma, 2021, 8: 451- 465. DOI: 10.2147/JHC.S303588. |
| [29] |
YANG LY, SHEN XT, SUN HT, et al. Neutrophil extracellular traps in hepatocellular carcinoma are enriched in oxidized mitochondrial DNA which is highly pro-inflammatory and pro-metastatic[J]. J Cancer, 2022, 13( 4): 1261- 1271. DOI: 10.7150/jca.64170. |
| [30] |
HU L, GAO L, DIRK H, et al. Regulatory effect of tumor-associated neutrophils in the development and progression of liver cancer[J]. J Clin Hepatol, 2020, 36( 9): 2100- 2102. DOI: 10.3969/j.issn.1001-5256.2020.09.2100.03. |
| [31] |
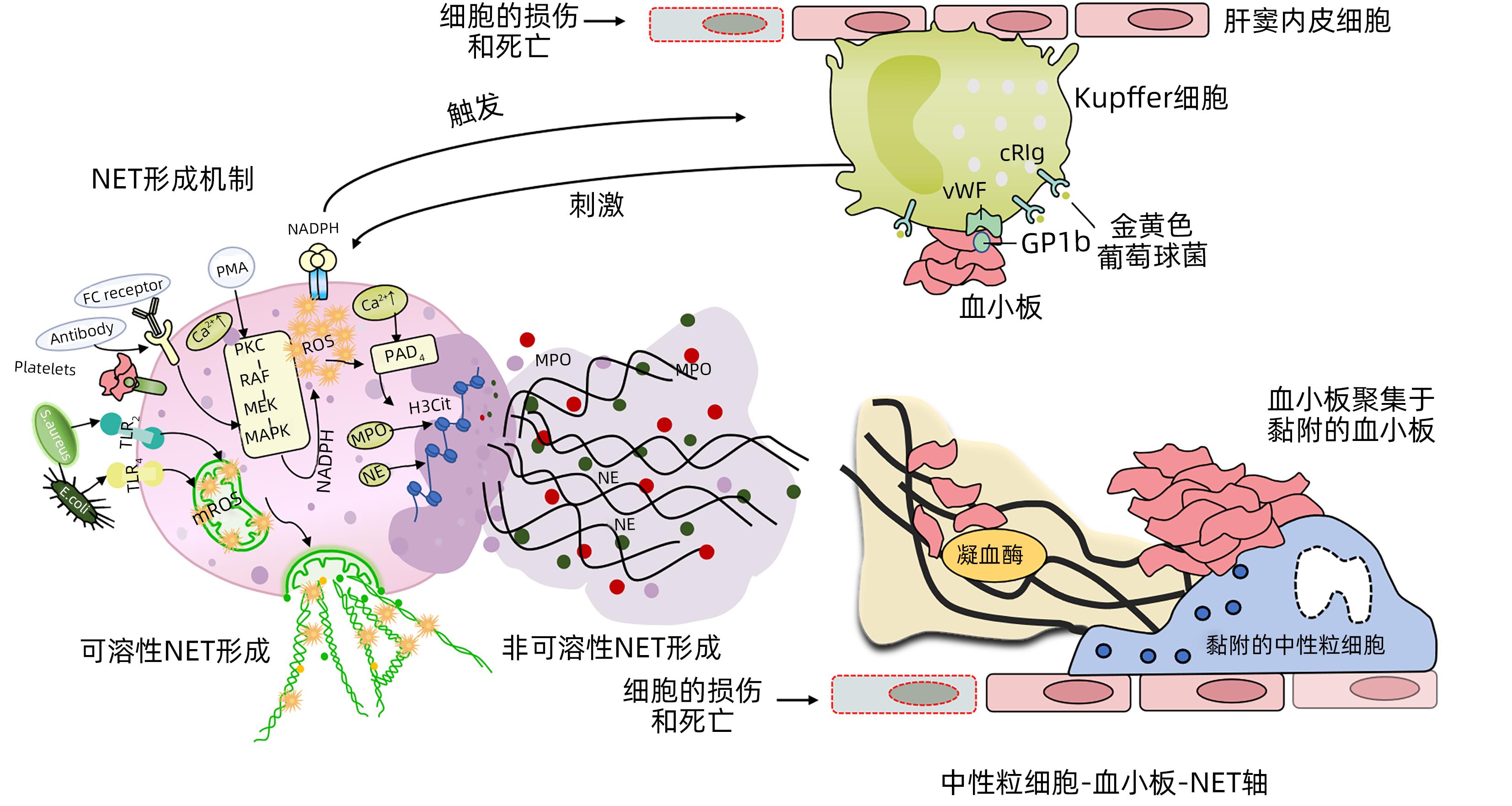
CAO L, LI Q, JI LS, et al. Formation mechanism of neutrophil extracellular traps and their role in liver diseases[J]. J Clin Hepatol, 2020, 36( 1): 205- 207. DOI: 10.3969/j.issn.1001-5256.2020.01.049. |






 DownLoad:
DownLoad:
