| [1] |
LESMANA CRA, RAHARJO M, GANI RA. Managing liver cirrhotic complications: Overview of esophageal and gastric varices[J]. Clin Mol Hepatol, 2020, 26( 4): 444- 460. DOI: 10.3350/cmh.2020.0022. |
| [2] |
LUO R, GAO J, GAN W, et al. Clinical-radiomics nomogram for predicting esophagogastric variceal bleeding risk noninvasively in patients with cirrhosis[J]. World J Gastroenterol, 2023, 29( 6): 1076- 1089. DOI: 10.3748/wjg.v29.i6.1076. |
| [3] |
LUO XF, HERNÁNDEZ-GEA V. Update on the management of gastric varices[J]. Liver Int, 2022, 42( 6): 1250- 1258. DOI: 10.1111/liv.15181. |
| [4] |
KHOURY T, NADELLA D, WILES A, et al. A review article on gastric varices with focus on the emerging role of endoscopic ultrasound-guided angiotherapy[J]. Eur J Gastroenterol Hepatol, 2018, 30( 12): 1411- 1415. DOI: 10.1097/MEG.0000000000001200. |
| [5] |
GARCIA-TSAO G, SANYAL AJ, GRACE ND, et al. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis[J]. Hepatology, 2007, 46( 3): 922- 938. DOI: 10.1002/hep.21907. |
| [6] |
de FRANCHIS R, FACULTY BV. Revising consensus in portal hypertension: Report of the Baveno V consensus workshop on methodology of diagnosis and therapy in portal hypertension[J]. J Hepatol, 2010, 53( 4): 762- 768. DOI: 10.1016/j.jhep.2010.06.004. |
| [7] |
TAN YY, GONG J, CHU Y, et al. Current status of diagnosis and treatment for gastric varices in liver cirrhosis with spontaneous portalsystemic shunt[J]. Chin J Dig Endosc, 2023, 40( 1): 78- 81. DOI: 10.3760/cma.j.cn321463-20220222-00029. |
| [8] |
WU Q, JIANG H, LINGHU EQ, et al. BRTO assisted endoscopic Histoacryl injection in treating gastric varices with gastrorenal shunt[J]. Minim Invasive Ther Allied Technol, 2016, 25( 6): 337- 344. DOI: 10.1080/13645706.2016.1192552. |
| [9] |
LO GH, LIN CW, TAI CM, et al. A prospective, randomized trial of thrombin versus cyanoacrylate injection in the control of acute gastric variceal hemorrhage[J]. Endoscopy, 2020, 52( 7): 548- 555. DOI: 10.1055/a-1127-3170. |
| [10] |
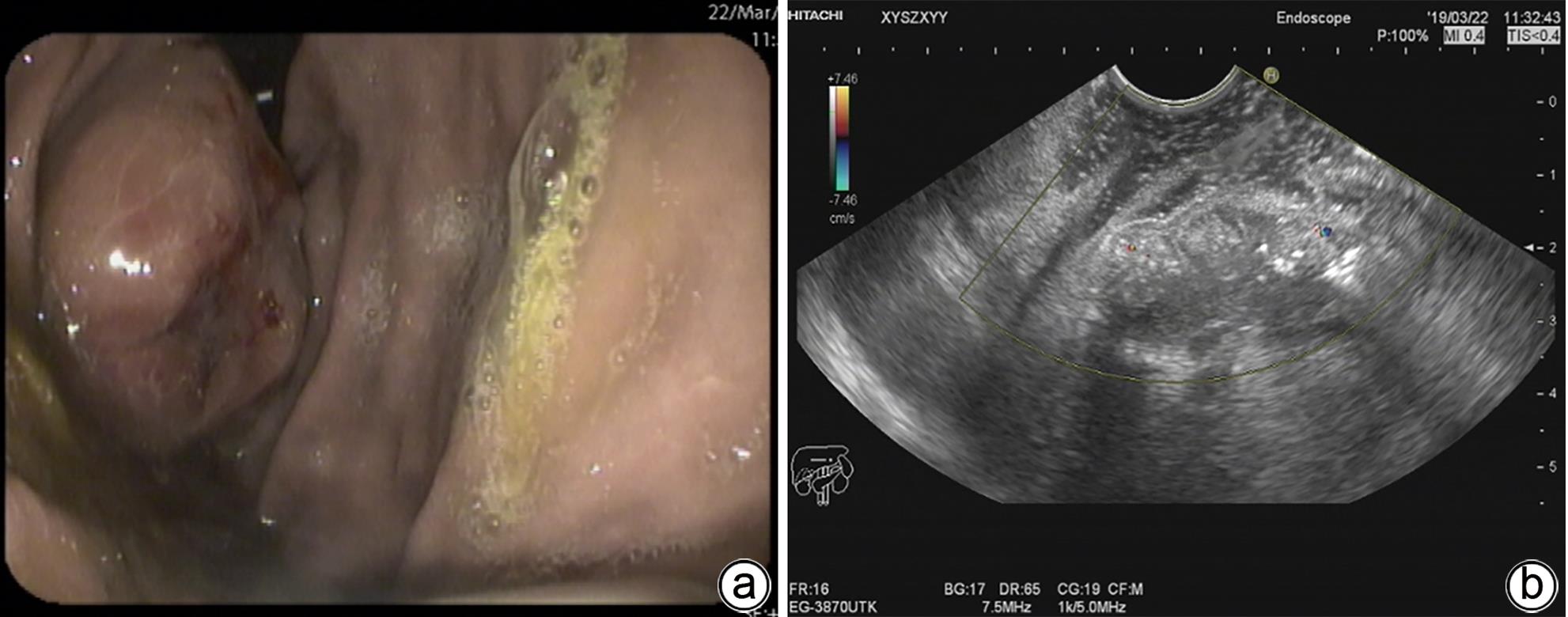
CHEN MK, DING Z, XIAO Y, et al. Preliminary study on the treatment of obvious splenorenal shunt with huge gastric varices by ultrasonic endoscope combined with gastroscope[J]. Chin J Dig Endosc, 2016, 33( 10): 707- 710. DOI: 10.3760/cma.j.issn.1007-5232.2016.10.013. |
| [11] |
MCCARTY TR, BAZARBASHI AN, HATHORN KE, et al. Combination therapy versus monotherapy for EUS-guided management of gastric varices: A systematic review and meta-analysis[J]. Endosc Ultrasound, 2020, 9( 1): 6- 15. DOI: 10.4103/eus.eus_37_19. |
| [12] |
Endoscopic Diagnosis and Treatment of Esophagogastric Varices Group of Chinese Society of Digestive Endoscopology. Chinese expert consensus on endoscopic cyanoacrylate injection for gastrointestinal varices with portal hypertension induced by liver cirrhosis(2022, Changsha)[J]. Chin J Dig Endosc, 2023, 40( 1): 12- 23. DOI: 10.3760/cma.j.cn321463-20221016-00530. |
| [13] |
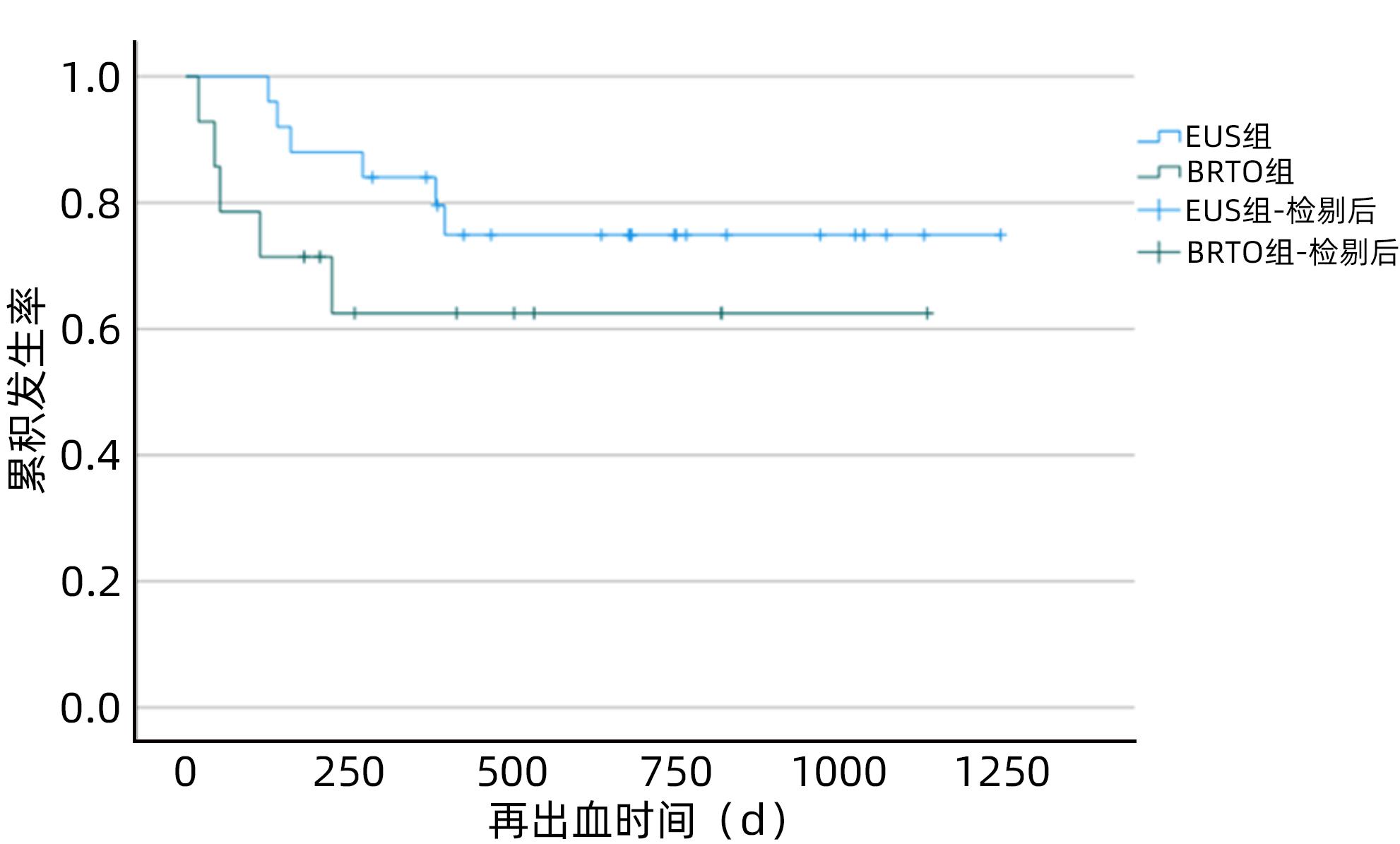
HUANG ZY, ZHANG WH, LV FJ, et al. Efficacy and safety of EUS-guided coil embolization combined with endoscopic cyanoacrylate injection versus balloon-occluded retrograde transvenous obliteration for gastric varices with high-risk ectopic embolism: A multicenter and retrospective cohort study[J]. Endosc Ultrasound, 2023, 12( 1): 74- 83. DOI: 10.4103/EUS-D-21-00260. |
| [14] |
KIM DJ, DARCY MD, MANI NB, et al. Modified balloon-occluded retrograde transvenous obliteration(BRTO) techniques for the treatment of gastric varices: Vascular plug-assisted retrograde transvenous obliteration(PARTO)/coil-assisted retrograde transvenous obliteration(CARTO)/balloon-occluded antegrade transvenous obliteration(BATO)[J]. Cardiovasc Intervent Radiol, 2018, 41( 6): 835- 847. DOI: 10.1007/s00270-018-1896-1. |
| [15] |
ROBLES-MEDRANDA C, VALERO M, NEBEL JA, et al. Endoscopic-ultrasound-guided coil and cyanoacrylate embolization for gastric varices and the roles of endoscopic Doppler and endosonographic varicealography in vascular targeting[J]. Dig Endosc, 2019, 31( 3): 283- 290. DOI: 10.1111/den.13305. |
| [16] |
TANG L, LI X, CUI J, et al. EUS-guided coil placement and cyanoacrylate glue injection for gastric variceal bleeding with obvious spontaneous portosystemic shunts[J]. Endosc Ultrasound, 2023, 12( 1): 84- 89. DOI: 10.4103/EUS-D-22-00006. |
| [17] |
NAKAMURA K, OKAMOTO T, SHIRATORI Y, et al. Endoscopic ultrasound-guided coil deployment with sclerotherapy for gastric varices[J]. Clin J Gastroenterol, 2021, 14( 1): 76- 83. DOI: 10.1007/s12328-020-01259-5. |
| [18] |
WANG XM, YU S, CHEN X, et al. Endoscopic ultrasound-guided injection of coils and cyanoacrylate glue for the treatment of gastric fundal varices with abnormal shunts: A series of case reports[J]. J Int Med Res, 2019, 47( 4): 1802- 1809. DOI: 10.1177/0300060519830207. |
| [19] |
ZHANG J, ZHU LR, YAO LW, et al. Deep learning-based pancreas segmentation and station recognition system in EUS: Development and validation of a useful training tool(with video)[J]. Gastrointest Endosc, 2020, 92( 4): 874- 885.e3. DOI: 10.1016/j.gie.2020.04.071. |
| [20] |
BAYANI A, HOSSEINI A, ASADI F, et al. Identifying predictors of varices grading in patients with cirrhosis using ensemble learning[J]. Clin Chem Lab Med, 2022, 60( 12): 1938- 1945. DOI: 10.1515/cclm-2022-0508. |
| [21] |
LEE CM, LEE SS, CHOI WM, et al. An index based on deep learning-measured spleen volume on CT for the assessment of high-risk varix in B-viral compensated cirrhosis[J]. Eur Radiol, 2021, 31( 5): 3355- 3365. DOI: 10.1007/s00330-020-07430-3. |








 DownLoad:
DownLoad: