| [1] |
BRAY F, FERLAY J, SOERJOMATARAM I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2018, 68(6): 394-424. DOI: 10.3322/caac.21492. |
| [2] |
|
| [3] |
AHMED RL, SCHMITZ KH, ANDERSON KE, et al. The metabolic syndrome and risk of incident colorectal cancer[J]. Cancer, 2006, 107(1): 28-36. DOI: 10.1002/cncr.21950. |
| [4] |
TAVANI A, BRAVI F, BOSETTI C, et al. Diabetes mellitus and subsite-specific colorectal cancer risks in the Iowa Women's Health Study[J]. Cancer Epidemiol Biomarkers Prev, 2005, 14(9): 2277. DOI: 10.1158/1055-9965.EPI-05-0331. |
| [5] |
|
| [6] |
LONARDO A, NASCIMBENI F, MANTOVANI A, et al. Hypertension, diabetes, atherosclerosis and NASH: Cause or consequence?[J]. J Hepatol, 2018, 68(2): 335-352. DOI: 10.1016/j.jhep.2017.09.021. |
| [7] |
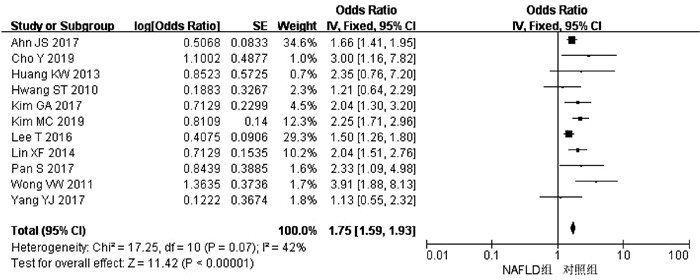
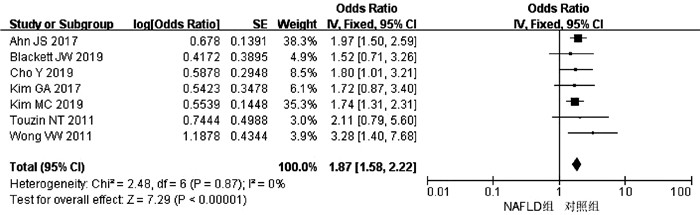
CHO Y, LIM SK, JOO SK, et al. Nonalcoholic steatohepatitis is associated with a higher risk of advanced colorectal neoplasm[J]. Liver Int, 2019, 39(9): 1722-1731. DOI: 10.1111/liv.14163. |
| [8] |
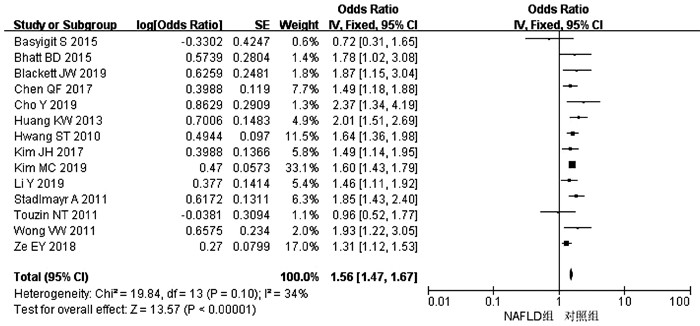
BASYIGIT S, UZMAN M, KEFELI A, et al. Absence of non-alcoholic fatty liver disease in the presence of insulin resistance is a strong predictor for colorectal carcinoma[J]. Int J Clin Exp Med, 2015, 8(10): 18601-18610. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4694373/ |
| [9] |
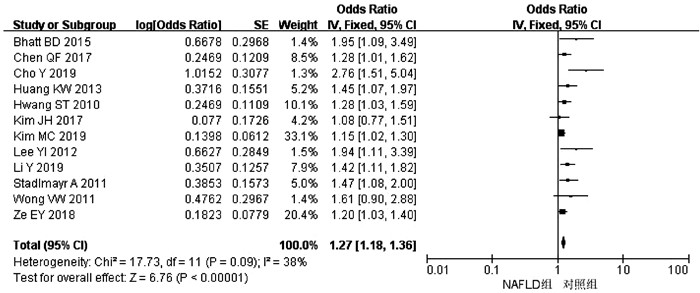
HWANG ST, CHO YK, PARK JH, et al. Relationship of non-alcoholic fatty liver disease to colorectal adenomatous polyps[J]. J Gastroenterol Hepatol, 2010, 25(3): 562-567. DOI: 10.1111/j.1440-1746.2009.06117.x. |
| [10] |
STADLMAYR A, AIGNER E, STEGER B, et al. Nonalcoholic fatty liver disease: An independent risk factor for colorectal neoplasia[J]. J Intern Med, 2011, 270(1): 41-49. DOI: 10.1111/j.1365-2796.2011.02377.x. |
| [11] |
TOUZIN NT, BUSH KN, WILLIAMS CD, et al. Prevalence of colonic adenomas in patients with nonalcoholic fatty liver disease[J]. Therap Adv Gastroenterol, 2011, 4(3): 169-176. DOI: 10.1177/1756283X11402118. |
| [12] |
WONG VW, WONG GL, TSANG SW, et al. High prevalence of colorectal neoplasm in patients with non-alcoholic steatohepatitis[J]. Gut, 2011, 60(6): 829-836. DOI: 10.1136/gut.2011.237974. |
| [13] |
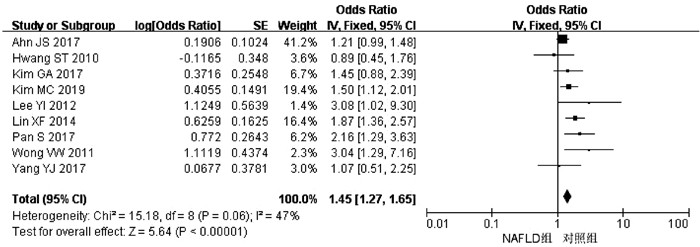
LEE YI, LIM YS, PARK HS. Colorectal neoplasms in relation to non-alcoholic fatty liver disease in Korean women: A retrospective cohort study[J]. J Gastroenterol Hepatol, 2012, 27(1): 91-95. DOI: 10.1111/j.1440-1746.2011.06816.x. |
| [14] |
HUANG KW, LEU HB, WANG YJ, et al. Patients with nonalcoholic fatty liver disease have higher risk of colorectal adenoma after negative baseline colonoscopy[J]. Colorectal Dis, 2013, 15(7): 830-835. DOI: 10.1111/codi.12172. |
| [15] |
LIN XF, SHI KQ, YOU J, et al. Increased risk of colorectal malignant neoplasm in patients with nonalcoholic fatty liver disease: A large study[J]. Mol Biol Rep, 2014, 41(5): 2989-2997. DOI: 10.1007/s11033-014-3157-y. |
| [16] |
BHATT BD, LUKOSE T, SIEGEL AB, et al. Increased risk of colorectal polyps in patients with non-alcoholic fatty liver disease undergoing liver transplant evaluation[J]. J Gastrointest Oncol, 2015, 6(5): 459-468. DOI: 10.3978/j.issn.2078-6891.2015.050. |
| [17] |
CHEN QF, ZHOU XD, SUN YJ, et al. Sex-influenced association of non-alcoholic fatty liver disease with colorectal adenomatous and hyperplastic polyps[J]. World J Gastroenterol, 2017, 23(28): 5206-5215. DOI: 10.3748/wjg.v23.i28.5206. |
| [18] |
KIM JH, CHO KI, KIM YA, et al. Elevated neutrophil-to-lymphocyte ratio in metabolic syndrome is associated with increased risk of colorectal adenoma[J]. Metab Syndr Relat Disord, 2017, 15(8): 393-399. DOI: 10.1089/met.2017.0041. |
| [19] |
ZE EY, KIM BJ, JUN DH, et al. The fatty liver index: A simple and accurate predictor of colorectal adenoma in an average-risk population[J]. Dis Colon Rectum, 2018, 61(1): 36-42. DOI: 10.1097/DCR.0000000000000973. |
| [20] |
BLACKETT JW, VERNA EC, LEBWOHL B. Increased prevalence of colorectal adenomas in patients with nonalcoholic fatty liver disease: A cross-sectional study[J]. Dig Dis, 2020, 38(3): 222-230. DOI: 10.1159/000502684. |
| [21] |
KIM MC, PARK JG, JANG BI, et al. Liver fibrosis is associated with risk for colorectal adenoma in patients with nonalcoholic fatty liver disease[J]. Medicine (Baltimore), 2019, 98(6): e14139. DOI: 10.1097/MD.0000000000014139. |
| [22] |
LI Y, LIU S, GAO Y, et al. Association between NAFLD and risk of colorectal adenoma in Chinese han population[J]. J Clin Transl Hepatol, 2019, 7(2): 99-105. DOI: 10.14218/JCTH.2019.00010. |
| [23] |
AHN JS, SINN DH, MIN YW, et al. Non-alcoholic fatty liver diseases and risk of colorectal neoplasia[J]. Aliment Pharmacol Ther, 2017, 45(2): 345-353. DOI: 10.1111/apt.13866. |
| [24] |
LEE T, YUN KE, CHANG Y, et al. Risk of colorectal neoplasia according to fatty liver severity and presence of gall bladder polyps[J]. Dig Dis Sci, 2016, 61(1): 317-324. DOI: 10.1007/s10620-015-3873-8. |
| [25] |
YANG YJ, BANG CS, SHIN SP, et al. Clinical impact of non-alcoholic fatty liver disease on the occurrence of colorectal neoplasm: Propensity score matching analysis[J]. PLoS One, 2017, 12(8): e0182014. DOI: 10.1371/journal.pone.0182014. |
| [26] |
PAN S, HONG W, WU W, et al. The relationship of nonalcoholic fatty liver disease and metabolic syndrome for colonoscopy colorectal neoplasm[J]. Medicine (Baltimore), 2017, 96(2): e5809. DOI: 10.1097/MD.0000000000005809. |
| [27] |
KIM GA, LEE HC, CHOE J, et al. Association between non-alcoholic fatty liver disease and cancer incidence rate[J]. J Hepatol, 2017. DOI: 10.1016/j.jhep.2017.09.012. |
| [28] |
KANG HW, KIM D, KIM HJ, et al. Visceral obesity and insulin resistance as risk factors for colorectal adenoma: A cross-sectional, case-control study[J]. Am J Gastroenterol, 2010, 105(1): 178-187. DOI: 10.1038/ajg.2009.541. |
| [29] |
CUSI K. Role of insulin resistance and lipotoxicity in non-alcoholic steatohepatitis[J]. Clin Liver Dis, 2009, 13(4): 545-563. DOI: 10.1016/j.cld.2009.07.009. |
| [30] |
WEI EK, GIOVANNUCCI E, FUCHS CS, et al. Low plasma adiponectin levels and risk of colorectal cancer in men: a prospective study[J]. J Natl Cancer Inst, 2005, 97(22): 1688-1694. DOI: 10.1093/jnci/dji376. |
| [31] |
BUZZETTI E, PINZANI M, TSOCHATZIS EA. The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD)[J]. Metabolism, 2016, 65(8): 1038-1048. DOI: 10.1016/j.metabol.2015.12.012. |
| [32] |
HYOGO H, YAMAGISHI S, IWAMOTO K, et al. Elevated levels of serum advanced glycation end products in patients with non-alcoholic steatohepatitis[J]. J Gastroenterol Hepatol, 2007, 22(7): 1112-1119. DOI: 10.1111/j.1440-1746.2007.04943.x. |
| [33] |
ABIRU S, MIGITA K, MAEDA Y, et al. Serum cytokine and soluble cytokine receptor levels in patients with non-alcoholic steatohepatitis[J]. Liver Int, 2006, 26(1): 39-45. DOI: 10.1111/j.1478-3231.2005.01191.x. |







 DownLoad:
DownLoad: