| [1] |
SEYEDIAN SS, NOKHOSTIN F, MALAMIR MD. A review of the diagnosis, prevention, and treatment methods of inflammatory bowel disease[J]. J Med Life, 2019, 12( 2): 113- 122. DOI: 10.25122/jml-2018-0075. |
| [2] |
BRUNER LP, WHITE AM, PROKSELL S. Inflammatory bowel disease[J]. Prim Care Clin Off Pract, 2023, 50( 3): 411- 427. DOI: 10.1016/j.pop.2023.03.009. |
| [3] |
YU ZQ, RUAN GC, BAI XY, et al. Growing burden of inflammatory bowel disease in China: Findings from the Global Burden of Disease Study 2021 and predictions to 2035[J]. Chin Med J(Engl), 2024, 137( 23): 2851- 2859. DOI: 10.1097/CM9.0000000000003345. |
| [4] |
VAVRICKA SR, SCHOEPFER A, SCHARL M, et al. Extraintestinal manifestations of inflammatory bowel disease[J]. Inflamm Bowel Dis, 2015, 21( 8): 1982- 1992. DOI: 10.1097/MIB.0000000000000392. |
| [5] |
GORDON H, BURISCH J, ELLUL P, et al. ECCO guidelines on extraintestinal manifestations in inflammatory bowel disease[J]. J Crohns Colitis, 2024, 18( 1): 1- 37. DOI: 10.1093/ecco-jcc/jjad108. |
| [6] |
MIELI-VERGANI G, VERGANI D, CZAJA AJ, et al. Autoimmune hepatitis[J]. Nat Rev Dis Primers, 2018, 4: 18017. DOI: 10.1038/nrdp.2018.17. |
| [7] |
LEUNG KK, DEEB M, HIRSCHFIELD GM. Review article: Pathophysiology and management of primary biliary cholangitis[J]. Aliment Pharmacol Ther, 2020, 52( 7): 1150- 1164. DOI: 10.1111/apt.16023. |
| [8] |
KARLSEN TH, FOLSERAAS T, THORBURN D, et al. Primary sclerosing cholangitis-a comprehensive review[J]. J Hepatol, 2017, 67( 6): 1298- 1323. DOI: 10.1016/j.jhep.2017.07.022. |
| [9] |
GERUSSI A, SCARAVAGLIO M, CRISTOFERI L, et al. Artificial intelligence for precision medicine in autoimmune liver disease[J]. Front Immunol, 2022, 13: 966329. DOI: 10.3389/fimmu.2022.966329. |
| [10] |
GHERSIN I, KHATEEB N, KATZ LH, et al. Comorbidities in adolescents with inflammatory bowel disease: Findings from a population-based cohort study[J]. Pediatr Res, 2020, 87( 7): 1256- 1262. DOI: 10.1038/s41390-019-0702-3. |
| [11] |
WEI SC, SHIEH MJ, CHANG MC, et al. Long-term follow-up of ulcerative colitis in Taiwan[J]. J Chin Med Assoc, 2012, 75( 4): 151- 155. DOI: 10.1016/j.jcma.2012.02.017. |
| [12] |
LUNDER AK, HOV JR, BORTHNE A, et al. Prevalence of sclerosing cholangitis detected by magnetic resonance cholangiography in patients with long-term inflammatory bowel disease[J]. Gastroenterology, 2016, 151( 4): 660- 669. e 4. DOI: 10.1053/j.gastro.2016.06.021. |
| [13] |
BRAMUZZO M, MARTELOSSI S, TORRE G, et al. Clinical features and risk factors of autoimmune liver involvement in pediatric inflammatory bowel disease[J]. J Pediatr Gastroenterol Nutr, 2016, 63( 2): 259- 264. DOI: 10.1097/mpg.0000000000001078. |
| [14] |
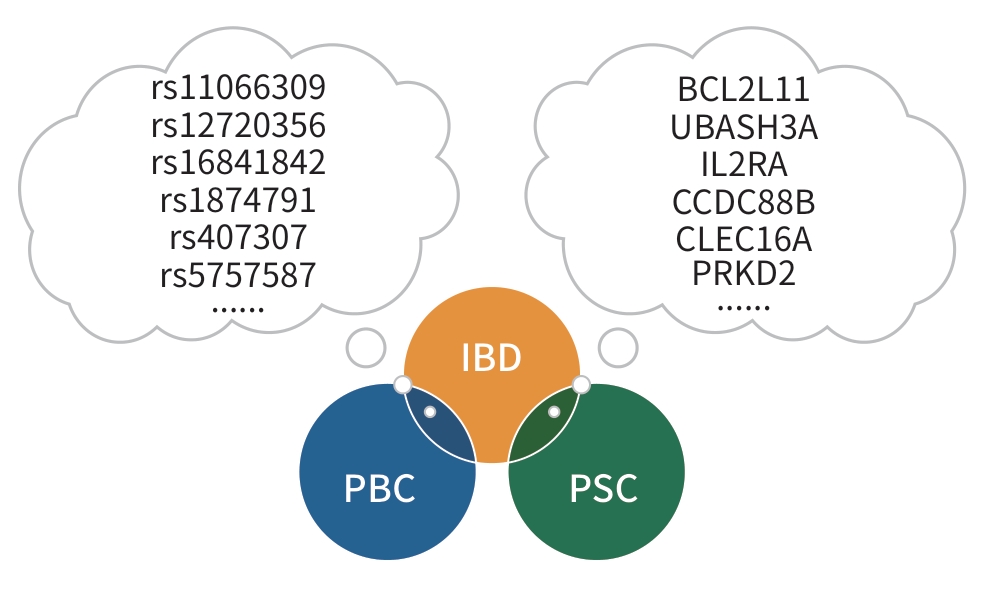
HUANG WT, JIANG R, LI ST, et al. Investigating shared genetic architecture between inflammatory bowel diseases and primary biliary cholangitis[J]. JHEP Rep, 2024, 6( 6): 101037. DOI: 10.1016/j.jhepr.2024.101037. |
| [15] |
ZHANG MY, XU TM, SUN YH, et al. Risk of comorbidity of autoimmune liver disease in patients with inflammatory bowel disease: A single-center case-control study in China[J]. J Dig Dis, 2024, 25( 9-10): 587- 593. DOI: 10.1111/1751-2980.13321. |
| [16] |
PONSIOEN CY. Diagnosis, differential diagnosis, and epidemiology of primary sclerosing cholangitis[J]. Dig Dis, 2015, Suppl 2: 134- 139. DOI: 10.1159/000440823. |
| [17] |
GREUTER T, VAVRICKA SR. Extraintestinal manifestations in inflammatory bowel disease-epidemiology, genetics, and pathogenesis[J]. Expert Rev Gastroenterol Hepatol, 2019, 13( 4): 307- 317. DOI: 10.1080/17474124.2019.1574569. |
| [18] |
SCHRUMPF E, FAUSA O, FØRRE O, et al. HLA antigens and immunoregulatory T cells in ulcerative colitis associated with hepatobiliary disease[J]. Scand J Gastroenterol, 1982, 17( 2): 187- 191. DOI: 10.3109/00365528209182038. |
| [19] |
JI SG, JURAN BD, MUCHA S, et al. Genome-wide association study of primary sclerosing cholangitis identifies new risk loci and quantifies the genetic relationship with inflammatory bowel disease[J]. Nat Genet, 2017, 49( 2): 269- 273. DOI: 10.1038/ng.3745. |
| [20] |
ZHANG HC, CHEN LL, FAN ZQ, et al. The causal effects of inflammatory bowel disease on primary biliary cholangitis: A bidirectional two-sample Mendelian randomization study[J]. Liver Int, 2023, 43( 8): 1741- 1748. DOI: 10.1111/liv.15616. |
| [21] |
HOV JR, KARLSEN TH. The microbiota and the gut-liver axis in primary sclerosing cholangitis[J]. Nat Rev Gastroenterol Hepatol, 2023, 20( 3): 135- 154. DOI: 10.1038/s41575-022-00690-y. |
| [22] |
SABINO J, VIEIRA-SILVA S, MACHIELS K, et al. Primary sclerosing cholangitis is characterised by intestinal dysbiosis independent from IBD[J]. Gut, 2016, 65( 10): 1681- 1689. DOI: 10.1136/gutjnl-2015-311004. |
| [23] |
KUMMEN M, HOLM K, ANMARKRUD JA, et al. The gut microbial profile in patients with primary sclerosing cholangitis is distinct from patients with ulcerative colitis without biliary disease and healthy controls[J]. Gut, 2017, 66( 4): 611- 619. DOI: 10.1136/gutjnl-2015-310500. |
| [24] |
LIWINSKI T, HEINEMANN M, SCHRAMM C. The intestinal and biliary microbiome in autoimmune liver disease-current evidence and concepts[J]. Semin Immunopathol, 2022, 44( 4): 485- 507. DOI: 10.1007/s00281-022-00936-6. |
| [25] |
BAJER L, KVERKA M, KOSTOVCIK M, et al. Distinct gut microbiota profiles in patients with primary sclerosing cholangitis and ulcerative colitis[J]. World J Gastroenterol, 2017, 23( 25): 4548- 4558. DOI: 10.3748/wjg.v23.i25.4548. |
| [26] |
NAKAMOTO N, SASAKI N, AOKI R, et al. Gut pathobionts underlie intestinal barrier dysfunction and liver T helper 17 cell immune response in primary sclerosing cholangitis[J]. Nat Microbiol, 2019, 4( 3): 492- 503. DOI: 10.1038/s41564-018-0333-1. |
| [27] |
TABIBIAN JH, TALWALKAR JA, LINDOR KD. Role of the microbiota and antibiotics in primary sclerosing cholangitis[J]. Biomed Res Int, 2013, 2013: 389537. DOI: 10.1155/2013/389537. |
| [28] |
HARADA K, NAKANUMA Y. Biliary innate immunity: Function and modulation[J]. Mediators Inflamm, 2010, 2010: 373878. DOI: 10.1155/2010/373878. |
| [29] |
YAN JB, LUO MM, CHEN ZY, et al. The function and role of the Th17/treg cell balance in inflammatory bowel disease[J]. J Immunol Res, 2020, 2020: 8813558. DOI: 10.1155/2020/8813558. |
| [30] |
JIANG P, ZHENG C, XIANG Y, et al. The involvement of TH17 cells in the pathogenesis of IBD[J]. Cytokine Growth Factor Rev, 2023, 69: 28- 42. DOI: 10.1016/j.cytogfr.2022.07.005. |
| [31] |
FENG TT, ZOU T, WANG X, et al. Clinical significance of changes in the Th17/Treg ratio in autoimmune liver disease[J]. World J Gastroenterol, 2017, 23( 21): 3832- 3838. DOI: 10.3748/wjg.v23.i21.3832. |
| [32] |
HOV JR, BOBERG KM, TARALDSRUD E, et al. Antineutrophil antibodies define clinical and genetic subgroups in primary sclerosing cholangitis[J]. Liver Int, 2017, 37( 3): 458- 465. DOI: 10.1111/liv.13238. |
| [33] |
KAWAMATA Y, FUJII R, HOSOYA M, et al. A G protein-coupled receptor responsive to bile acids[J]. J Biol Chem, 2003, 278( 11): 9435- 9440. DOI: 10.1074/jbc.m209706200. |
| [34] |
VAVASSORI P, MENCARELLI A, RENGA B, et al. The bile acid receptor FXR is a modulator of intestinal innate immunity[J]. J Immunol, 2009, 183( 10): 6251- 6261. DOI: 10.4049/jimmunol.0803978. |
| [35] |
HOV JR, KEITEL V, LAERDAHL JK, et al. Mutational characterization of the bile acid receptor TGR5 in primary sclerosing cholangitis[J]. PLoS One, 2010, 5( 8): e12403. DOI: 10.1371/journal.pone.0012403. |
| [36] |
DING LL, YANG L, WANG ZT, et al. Bile acid nuclear receptor FXR and digestive system diseases[J]. Acta Pharm Sin B, 2015, 5( 2): 135- 144. DOI: 10.1016/j.apsb.2015.01.004. |
| [37] |
GADALETA RM, van ERPECUM KJ, OLDENBURG B, et al. Farnesoid X receptor activation inhibits inflammation and preserves the intestinal barrier in inflammatory bowel disease[J]. Gut, 2011, 60( 4): 463- 472. DOI: 10.1136/gut.2010.212159. |
| [38] |
|
| [39] |
BRIDOUX-HENNO L, MAGGIORE G, JOHANET C, et al. Features and outcome of autoimmune hepatitis type 2 presenting with isolated positivity for anti-liver cytosol antibody[J]. Clin Gastroenterol Hepatol, 2004, 2( 9): 825- 830. DOI: 10.1016/s1542-3565(04)00354-4. |
| [40] |
HENNES EM, ZENIYA M, CZAJA AJ, et al. Simplified criteria for the diagnosis of autoimmune hepatitis[J]. Hepatology, 2008, 48( 1): 169- 176. DOI: 10.1002/hep.22322. |
| [41] |
BOBERG KM, CHAPMAN RW, HIRSCHFIELD GM, et al. Overlap syndromes: The International Autoimmune Hepatitis Group(IAIHG) position statement on a controversial issue[J]. J Hepatol, 2011, 54( 2): 374- 385. DOI: 10.1016/j.jhep.2010.09.002. |
| [42] |
DEFILIPPIS EM, KUMAR S. Clinical presentation and outcomes of autoimmune hepatitis in inflammatory bowel disease[J]. Dig Dis Sci, 2015, 60( 10): 2873- 2880. DOI: 10.1007/s10620-015-3699-4. |
| [43] |
VENKATESH SK, WELLE CL, MILLER FH, et al. Correction to: Reporting standards for primary sclerosing cholangitis using MRI and MR cholangiopancreatography: Guidelines from MR working group of the international primary sclerosing cholangitis study group[J]. Eur Radiol, 2022, 32( 4): 2860. DOI: 10.1007/s00330-021-08333-7. |
| [44] |
FRAGA M, FOURNIER N, SAFRONEEVA E, et al. Primary sclerosing cholangitis in the Swiss inflammatory bowel disease cohort study: Prevalence, risk factors, and long-term follow-up[J]. Eur J Gastroenterol Hepatol, 2017, 29( 1): 91- 97. DOI: 10.1097/MEG.0000000000000747. |
| [45] |
KIM YS, HURLEY EH, PARK Y, et al. Primary sclerosing cholangitis(PSC) and inflammatory bowel disease(IBD): A condition exemplifying the crosstalk of the gut-liver axis[J]. Exp Mol Med, 2023, 55( 7): 1380- 1387. DOI: 10.1038/s12276-023-01042-9. |
| [46] |
CHAPMAN MH, THORBURN D, HIRSCHFIELD GM, et al. British Society of Gastroenterology and UK-PSC guidelines for the diagnosis and management of primary sclerosing cholangitis[J]. Gut, 2019, 68( 8): 1356- 1378. DOI: 10.1136/gutjnl-2018-317993. |
| [47] |
LIBERAL R, GASPAR R, LOPES S, et al. Primary biliary cholangitis in patients with inflammatory bowel disease[J]. Clin Res Hepatol Gastroenterol, 2020, 44( 1): e5- e9. DOI: 10.1016/j.clinre.2019.05.002. |
| [48] |
VIERLING JM. Autoimmune hepatitis and overlap syndromes: Diagnosis and management[J]. Clin Gastroenterol Hepatol, 2015, 13( 12): 2088- 2108. DOI: 10.1016/j.cgh.2015.08.012. |
| [49] |
European Association for the Study of the Liver. EASL clinical practice guidelines: Autoimmune hepatitis[J]. J Hepatol, 2015, 63( 4): 971- 1004. DOI: 10.1016/j.jhep.2015.06.030. |
| [50] |
TRAUNER M, BOWLUS CL, GULAMHUSEIN A, et al. Safety and sustained efficacy of the farnesoid X receptor(FXR) agonist cilofexor over a 96-week open-label extension in patients with PSC[J]. Clin Gastroenterol Hepatol, 2023, 21( 6): 1552- 1560. e 2. DOI: 10.1016/j.cgh.2022.07.024. |
| [51] |
RICCIUTO A, LIU K, EL-MATARY W, et al. Oral vancomycin is associated with improved inflammatory bowel disease clinical outcomes in primary sclerosing cholangitis-associated inflammatory bowel disease(PSC-IBD): A matched analysis from the Paediatric PSC Consortium[J]. Aliment Pharmacol Ther, 2024, 59( 10): 1236- 1247. DOI: 10.1111/apt.17936. |






 DownLoad:
DownLoad: