| [1] |
SCHWÄRZLER J, GRABHERR F, GRANDER C, et al. The pathophysiology of MASLD: An immunometabolic perspective[J]. Expert Rev Clin Immunol, 2024, 20( 4): 375- 386. DOI: 10.1080/1744666X.2023.2294046. |
| [2] |
WONG VW, EKSTEDT M, WONG GL, et al. Changing epidemiology, global trends and implications for outcomes of NAFLD[J]. J Hepatol, 2023, 79( 3): 842- 852. DOI: 10.1016/j.jhep.2023.04.036. |
| [3] |
TARGHER G, BYRNE CD, TILG H. MASLD: A systemic metabolic disorder with cardiovascular and malignant complications[J]. Gut, 2024, 73( 4): 691- 702. DOI: 10.1136/gutjnl-2023-330595. |
| [4] |
LI F, LI MW, WANG YS. Therapeutic paradigms and potential therapies for nonalcoholic steatohepatitis[J]. J Clin Hepatol, 2024, 40( 10): 2082- 2086. DOI: 10.12449/JCH241025. 李凤, 李茂微, 王雨杉. 非酒精性脂肪肝病的治疗模式和潜在疗法[J]. 临床肝胆病杂志, 2024, 40( 10): 2082- 2086. DOI: 10.12449/JCH241025. |
| [5] |
YOUNOSSI ZM, STEPANOVA M, RACILA A, et al. Health-related quality of life(HRQL) assessments in a 52-week, double-blind, randomized, placebo-controlled phase 3 study of resmetirom(MGL-3196) in patients with metabolic dysfunction associated steatohepatitis(MASH) and fibrosis[J]. Hepatology, 2025, 81( 4): 1318- 1327. DOI: 10.1097/HEP. 0000000000001084.
|
| [6] |
SHIMOTOYODOME A, HARAMIZU S, INABA M, et al. Exercise and green tea extract stimulate fat oxidation and prevent obesity in mice[J]. Med Sci Sports Exerc, 2005, 37( 11): 1884- 1892. DOI: 10.1249/01.mss.0000178062.66981.a8. |
| [7] |
YE Q, LIU Y, CHEN JP, et al. Research progress on chemical constituents and pharmacological activities of green tea[J]. Drug Eval Res, 2021, 44( 12): 2711- 2719. DOI: 10.7501/j.issn.1674-6376.2021.12.026. |
| [8] |
SINGH BN, SHANKAR S, SRIVASTAVA RK. Green tea catechin, epigallocatechin-3-gallate(EGCG): Mechanisms, perspectives and clinical applications[J]. Biochem Pharmacol, 2011, 82( 12): 1807- 1821. DOI: 10.1016/j.bcp.2011.07.093. |
| [9] |
HE MJ, CHU TH, WANG ZT, et al. Inhibition of macrophages inflammasome activation via autophagic degradation of HMGB1 by EGCG ameliorates HBV-induced liver injury and fibrosis[J]. Front Immunol, 2023, 14: 1147379. DOI: 10.3389/fimmu.2023.1147379. |
| [10] |
CZECH TY, SEKI E. Kupffer cell TLR2/3 signaling: A pathway for EGCG amelioration of ethanol-induced hepatic injury[J]. Cell Mol Gastroenterol Hepatol, 2020, 9( 1): 187- 188. DOI: 10.1016/j.jcmgh.2019.10.001. |
| [11] |
LIN YX, HUANG J, GAO TF, et al. Preliminary study on hepatoprotective effect and mechanism of(-)-epigallocatechin-3-gallate against acetaminophen-induced liver injury in rats[J]. Iran J Pharm Res, 2021, 20( 3): 46- 56. DOI: 10.22037/ijpr.2020.112727.13918. |
| [12] |
TANG GY, XU Y, ZHANG C, et al. Green tea and epigallocatechin gallate(EGCG) for the management of nonalcoholic fatty liver diseases(NAFLD): Insights into the role of oxidative stress and antioxidant mechanism[J]. Antioxidants(Basel), 2021, 10( 7): 1076. DOI: 10.3390/antiox10071076. |
| [13] |
KLEINER DE, BRUNT EM, van NATTA M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease[J]. Hepatology, 2005, 41( 6): 1313- 1321. DOI: 10.1002/hep.20701. |
| [14] |
OHISHI T, GOTO S, MONIRA P, et al. Anti-inflammatory action of green tea[J]. Antiinflamm Antiallergy Agents Med Chem, 2016, 15( 2): 74- 90. DOI: 10.2174/1871523015666160915154443. |
| [15] |
ALAM M, ALI S, ASHRAF GM, et al. Epigallocatechin 3-gallate: From green tea to cancer therapeutics[J]. Food Chem, 2022, 379: 132135. DOI: 10.1016/j.foodchem.2022.132135. |
| [16] |
MASTERJOHN C, BRUNO RS. Therapeutic potential of green tea in nonalcoholic fatty liver disease[J]. Nutr Rev, 2012, 70( 1): 41- 56. DOI: 10.1111/j.1753-4887.2011.00440.x. |
| [17] |
DING Y, SUN X, CHEN YN, et al. Epigallocatechin gallate attenuated non-alcoholic steatohepatitis induced by methionine- and choline-deficient diet[J]. Eur J Pharmacol, 2015, 761: 405- 412. DOI: 10.1016/j.ejphar.2015.05.005. |
| [18] |
LIU JJ, SUN JY, YU JK, et al. Gut microbiome determines therapeutic effects of OCA on NAFLD by modulating bile acid metabolism[J]. NPJ Biofilms Microbiomes, 2023, 9( 1): 29. DOI: 10.1038/s41522-023-00399-z. |
| [19] |
YOUNOSSI ZM, RATZIU V, LOOMBA R, et al. Obeticholic acid for the treatment of non-alcoholic steatohepatitis: Interim analysis from a multicentre, randomised, placebo-controlled phase 3 trial[J]. Lancet, 2019, 394( 10215): 2184- 2196. DOI: 10.1016/S0140-6736(19)33041-7. |
| [20] |
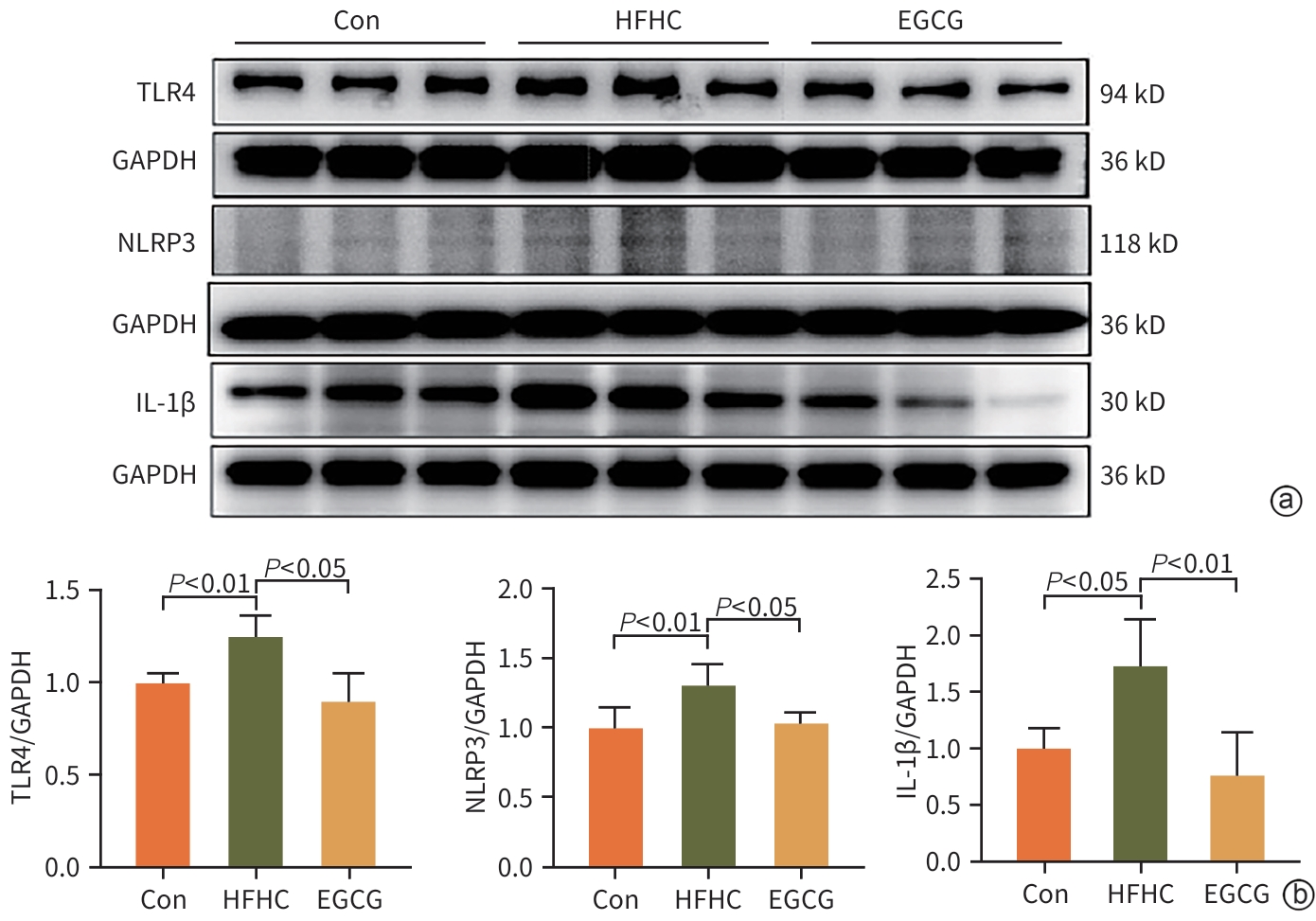
HOU HM, YANG WL, BAO SQ, et al. Epigallocatechin gallate suppresses inflammatory responses by inhibiting toll-like receptor 4 signaling and alleviates insulin resistance in the livers of high-fat-diet rats[J]. J Oleo Sci, 2020, 69( 5): 479- 486. DOI: 10.5650/jos.ess19303. |
| [21] |
XIAO J, HO CT, LIONG EC, et al. Epigallocatechin gallate attenuates fibrosis, oxidative stress, and inflammation in non-alcoholic fatty liver disease rat model through TGF/SMAD, PI3K/Akt/FoxO1, and NF-kappa B pathways[J]. Eur J Nutr, 2014, 53( 1): 187- 199. DOI: 10.1007/s00394-013-0516-8. |
| [22] |
LIN QW, ZHANG S, LU WQ. Research progress of NOD-like signaling pathways and the relationship between NOD and tumor[J]. China Oncol, 2019, 29( 3): 223- 228. DOI: 10.19401/j.cnki.1007-3639.2019.03.011. |
| [23] |
BAUER S, HEZINGER L, REXHEPI F, et al. NOD-like receptors-emerging links to obesity and associated morbidities[J]. Int J Mol Sci, 2023, 24( 10): 8595. DOI: 10.3390/ijms24108595. |
| [24] |
LI HX, CAO ZQ, WANG LL, et al. Chronic high-fat diet induces galectin-3 and TLR4 to activate NLRP3 inflammasome in NASH[J]. J Nutr Biochem, 2023, 112: 109217. DOI: 10.1016/j.jnutbio.2022.109217. |
| [25] |
ZHENG D, KERN L, ELINAV E. The NLRP6 inflammasome[J]. Immunology, 2021, 162( 3): 281- 289. DOI: 10.1111/imm.13293. |
| [26] |
HUANG CY, LIU QH, TANG Q, et al. Hepatocyte-specific deletion of Nlrp6 in mice exacerbates the development of non-alcoholic steatohepatitis[J]. Free Radic Biol Med, 2021, 169: 110- 121. DOI: 10.1016/j.freeradbiomed.2021.04.008. |
| [27] |
HASEGAWA M, FUJIMOTO Y, LUCAS PC, et al. A critical role of RICK/RIP2 polyubiquitination in Nod-induced NF-kappaB activation[J]. EMBO J, 2008, 27( 2): 373- 383. DOI: 10.1038/sj.emboj.7601962. |







 DownLoad:
DownLoad: