| [1] |
KERKAR N, CHAN A. Autoimmune hepatitis, sclerosing cholangitis, and autoimmune sclerosing cholangitis or overlap syndrome[J]. Clin Liver Dis, 2018, 22( 4): 689- 702. DOI: 10.1016/j.cld.2018.06.005. |
| [2] |
VOLK ML, REAU N. Diagnosis and management of autoimmune hepatitis in adults and children: A patient-friendly summary of the 2019 AASLD guidelines[J]. Clin Liver Dis(Hoboken), 2021, 17( 2): 85- 89. DOI: 10.1002/cld.1080. |
| [3] |
LOHSE AW, SEBODE M, JØRGENSEN MH, et al. Second-line and third-line therapy for autoimmune hepatitis: A position statement from the European Reference Network on Hepatological Diseases and the International Autoimmune Hepatitis Group[J]. J Hepatol, 2020, 73( 6): 1496- 1506. DOI: 10.1016/j.jhep.2020.07.023. |
| [4] |
|
| [5] |
NOORT WA, KRUISSELBRINK AB, IN'T ANKER PS, et al. Mesenchymal stem cells promote engraftment of human umbilical cord blood-derived CD34 + cells in NOD/SCID mice[J]. Exp Hematol, 2002, 30( 8): 870- 878. DOI: 10.1016/S0301-472X(02)00820-2. |
| [6] |
di NICOLA M, CARLO-STELLA C, MAGNI M, et al. Human bone marrow stromal cells suppress T-lymphocyte proliferation induced by cellular or nonspecific mitogenic stimuli[J]. Blood, 2002, 99( 10): 3838- 3843. DOI: 10.1182/blood.v99.10.3838. |
| [7] |
TSE WT, PENDLETON JD, BEYER WM, et al. Suppression of allogeneic T-cell proliferation by human marrow stromal cells: Implications in transplantation[J]. Transplantation, 2003, 75( 3): 389- 397. DOI: 10.1097/01.TP.0000045055.63901.A9. |
| [8] |
CORCIONE A, BENVENUTO F, FERRETTI E, et al. Human mesenchymal stem cells modulate B-cell functions[J]. Blood, 2006, 107( 1): 367- 372. DOI: 10.1182/blood-2005-07-2657. |
| [9] |
JIANG XX, ZHANG Y, LIU B, et al. Human mesenchymal stem cells inhibit differentiation and function of monocyte-derived dendritic cells[J]. Blood, 2005, 105( 10): 4120- 4126. DOI: 10.1182/blood-2004-02-0586. |
| [10] |
ENGLISH K, BARRY FP, MAHON BP. Murine mesenchymal stem cells suppress dendritic cell migration, maturation and antigen presentation[J]. Immunol Lett, 2008, 115( 1): 50- 58. DOI: 10.1016/j.imlet.2007.10.002. |
| [11] |
SPAGGIARI GM, CAPOBIANCO A, BECCHETTI S, et al. Mesenchymal stem cell-natural killer cell interactions: Evidence that activated NK cells are capable of killing MSCs, whereas MSCs can inhibit IL-2-induced NK-cell proliferation[J]. Blood, 2006, 107( 4): 1484- 1490. DOI: 10.1182/blood-2005-07-2775. |
| [12] |
SHI YF, WANG Y, LI Q, et al. Immunoregulatory mechanisms of mesenchymal stem and stromal cells in inflammatory diseases[J]. Nat Rev Nephrol, 2018, 14( 8): 493- 507. DOI: 10.1038/s41581-018-0023-5. |
| [13] |
STEFAŃSKA K, VOLPONI AA, KULUS M, et al. Dental pulp stem cells-A basic research and future application in regenerative medicine[J]. Biomed Pharmacother, 2024, 178: 116990. DOI: 10.1016/j.biopha.2024.116990. |
| [14] |
|
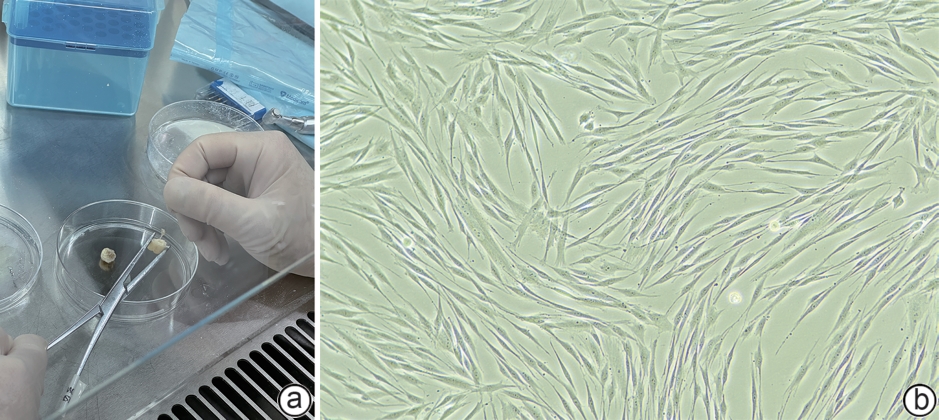
| [15] |
TAŞLı PN, TAPŞıN S, DEMIREL S, et al. Isolation and characterization of dental pulp stem cells from a patient with Papillon-Lefèvre syndrome[J]. J Endod, 2013, 39( 1): 31- 38. DOI: 10.1016/j.joen.2012.09.024. |
| [16] |
RODAS-JUNCO BA, VILLICAÑA C. Dental pulp stem cells: Current advances in isolation, expansion and preservation[J]. Tissue Eng Regen Med, 2017, 14( 4): 333- 347. DOI: 10.1007/s13770-017-0036-3. |
| [17] |
LAN XY, SUN ZW, CHU CY, et al. Dental pulp stem cells: An attractive alternative for cell therapy in ischemic stroke[J]. Front Neurol, 2019, 10: 824. DOI: 10.3389/fneur.2019.00824. |
| [18] |
MATSUBARA K, MATSUSHITA Y, SAKAI K, et al. Secreted ectodomain of sialic acid-binding Ig-like lectin-9 and monocyte chemoattractant protein-1 promote recovery after rat spinal cord injury by altering macrophage polarity[J]. J Neurosci, 2015, 35( 6): 2452- 2464. DOI: 10.1523/JNEUROSCI.4088-14.2015. |
| [19] |
LI FY, WANG XX, SHI J, et al. Anti-inflammatory effect of dental pulp stem cells[J]. Front Immunol, 2023, 14: 1284868. DOI: 10.3389/fimmu.2023.1284868. |
| [20] |
DEMIRCAN PC, SARIBOYACI AE, UNAL ZS, et al. Immunoregulatory effects of human dental pulp-derived stem cells on T cells: Comparison of transwell co-culture and mixed lymphocyte reaction systems[J]. Cytotherapy, 2011, 13( 10): 1205- 1220. DOI: 10.3109/14653249.2011.605351. |
| [21] |
CHEN PX, LIN YC, LIN WB, et al. Human dental pulp stem cells have comparable abilities to umbilical cord mesenchymal stem/stromal cells in regulating inflammation and ameliorating hepatic fibrosis[J]. Hum Cell, 2024, 37( 1): 204- 213. DOI: 10.1007/s13577-023-01004-3. |
| [22] |
IWANAKA T, YAMAZA T, SONODA S, et al. A model study for the manufacture and validation of clinical-grade deciduous dental pulp stem cells for chronic liver fibrosis treatment[J]. Stem Cell Res Ther, 2020, 11( 1): 134. DOI: 10.1186/s13287-020-01630-w. |
| [23] |
LI Y, SONG GY, JIANG Y, et al. Single-cell transcriptome analysis of stem cells from human exfoliated deciduous teeth investigating functional heterogeneity in immunomodulation[J]. Sci Rep, 2024, 14( 1): 31279. DOI: 10.1038/s41598-024-82734-8. |






 DownLoad:
DownLoad: