| [1] |
National Center for Clinical Research of Infectious Diseases. Expert consensus on the diagnosis and treatment of intrahepatic cholestasis(2021 edition)[J]. Chin J Clin Infect Dis, 2021, 14( 6): 401- 412. DOI: 10.3760/cma.j.issn.1674-2397.2021.06.001. |
| [2] |
CIFUENTES-SILVA E, CABELLO-VERRUGIO C. Bile acids as signaling molecules: Role of ursodeoxycholic acid in cholestatic liver disease[J]. Curr Protein Pept Sci, 2024, 25( 3): 206- 214. DOI: 10.2174/1389203724-666230818092800. |
| [3] |
SUN XL, HU X, ZHANG YT. Clinical application of ursodeoxycholic acid[J]. Chin J Pharmacovigil, 2022, 19( 10): 1149- 1153. DOI: 10.19803/j.1672-8629.20210604. |
| [4] |
|
| [5] |
HO PTB, CLARK IM, LE LTT. MicroRNA-based diagnosis and therapy[J]. Int J Mol Sci, 2022, 23( 13): 7167. DOI: 10.3390/ijms23137167. |
| [6] |
SEARLES CD. MicroRNAs and cardiovascular disease risk[J]. Curr Cardiol Rep, 2024, 26( 2): 51- 60. DOI: 10.1007/s11886-023-02014-1. |
| [7] |
VAGHF A, KHANSARINEJAD B, GHAZNAVI-RAD E, et al. The role of microRNAs in diseases and related signaling pathways[J]. Mol Biol Rep, 2022, 49( 7): 6789- 6801. DOI: 10.1007/s11033-021-06725-y. |
| [8] |
KAGAWA T, SHIRAI Y, ODA S, et al. Identification of specific microRNA biomarkers in early stages of hepatocellular injury, cholestasis, and steatosis in rats[J]. Toxicol Sci, 2018, 166( 1): 228- 239. DOI: 10.1093/toxsci/kfy200. |
| [9] |
MARIN JJG, BUJANDA L, BANALES JM. MicroRNAs and cholestatic liver diseases[J]. Curr Opin Gastroenterol, 2014, 30( 3): 303- 309. DOI: 10.1097/MOG.0000000000000051. |
| [10] |
YOKODA RT, RODRIGUEZ EA. Review: Pathogenesis of cholestatic liver diseases[J]. World J Hepatol, 2020, 12( 8): 423- 435. DOI: 10.4254/wjh.v12.i8.423. |
| [11] |
FUCHS CD, TRAUNER M. Role of bile acids and their receptors in gastrointestinal and hepatic pathophysiology[J]. Nat Rev Gastroenterol Hepatol, 2022, 19( 7): 432- 450. DOI: 10.1038/s41575-021-00566-7. |
| [12] |
GHANBARINEJAD V, OMMATI MM, JIA ZP, et al. Disturbed mitochondrial redox state and tissue energy charge in cholestasis[J]. J Biochem Mol Toxicol, 2021, 35( 9): e22846. DOI: 10.1002/jbt.22846. |
| [13] |
CHEN J, ZHANG SJ. The role of inflammation in cholestatic liver injury[J]. J Inflamm Res, 2023, 16: 4527- 4540. DOI: 10.2147/JIR.S430730. |
| [14] |
YU LL, LIU YR, WANG SH, et al. Cholestasis: Exploring the triangular relationship of gut microbiota-bile acid-cholestasis and the potential probiotic strategies[J]. Gut Microbes, 2023, 15( 1): 2181930. DOI: 10.1080/19490976.2023.2181930. |
| [15] |
ERICE O, MUNOZ-GARRIDO P, VAQUERO J, et al. MicroRNA-506 promotes primary biliary cholangitis-like features in cholangiocytes and immune activation[J]. Hepatology, 2018, 67( 4): 1420- 1440. DOI: 10.1002/hep.29533. |
| [16] |
HONG L, ZHU XL, HANG C, et al. The diagnostic value of CG, LAP and miR-155 in intrahepatic cholestasis of pregnancy and relationship with disease severity[J]. Chin J Integr Tradit West Med Liver Dis, 2023, 33( 12): 1069- 1072, 1077. DOI: 10.3969/j.issn.1005-0264.2023.012.004. |
| [17] |
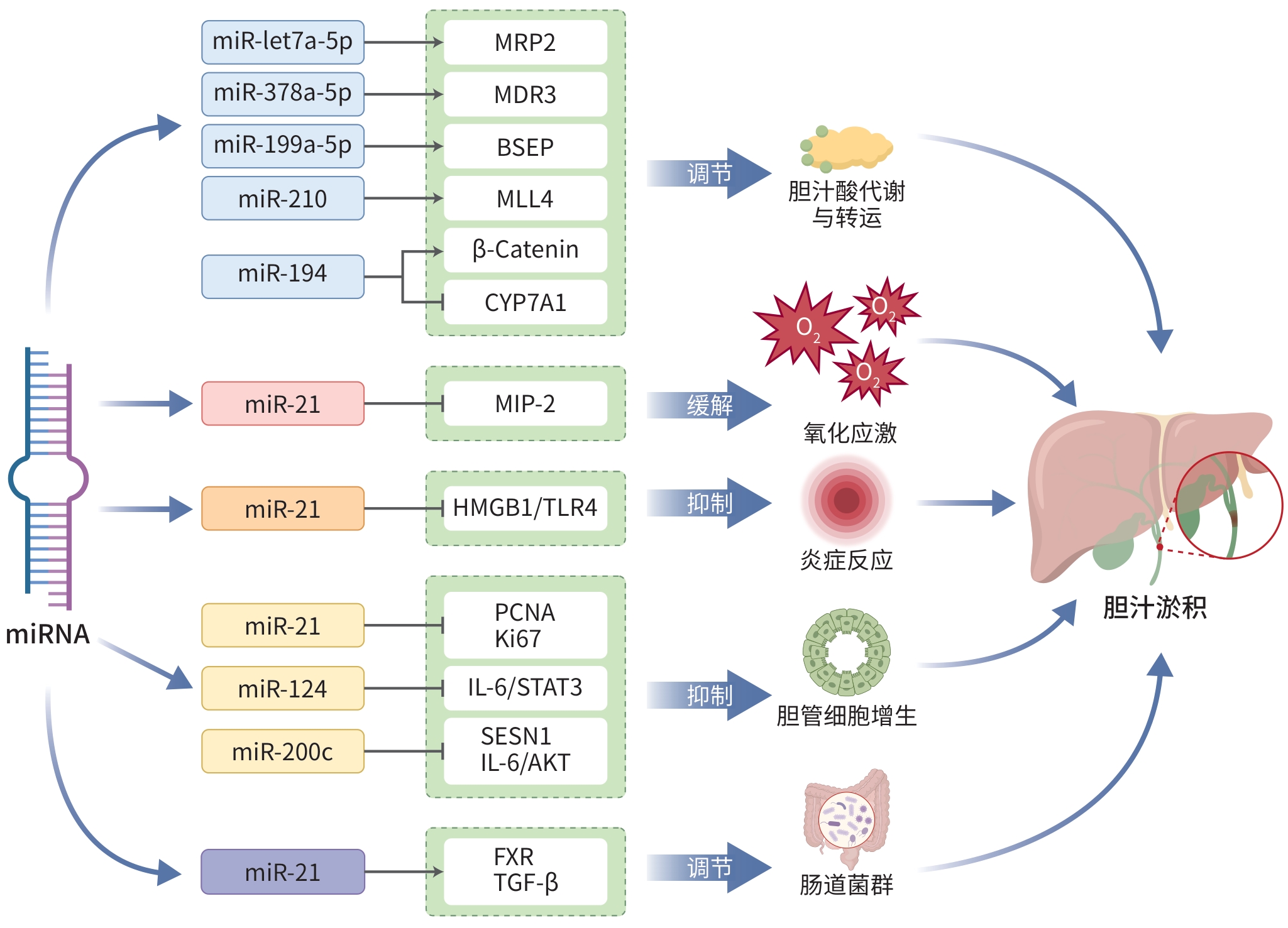
BALASUBRAMANIYAN N, DEVEREAUX MW, ORLICKY DJ, et al. Up-regulation of miR-let7a-5p leads to decreased expression of ABCC2 in obstructive cholestasis[J]. Hepatol Commun, 2019, 3( 12): 1674- 1686. DOI: 10.1002/hep4.1433. |
| [18] |
SONG CW, QIU W, ZHOU XQ, et al. Elevated hepatic MDR3/ABCB4 is directly mediated by miR-378a-5p in human obstructive cholestasis[J]. Eur Rev Med Pharmacol Sci, 2019, 23( 6): 2539- 2547. DOI: 10.26355/eurrev_201903_17402. |
| [19] |
BALASUBRAMANIYAN N, DEVEREAUX MW, ORLICKY DJ, et al. miR-199a-5p inhibits the expression of ABCB11 in obstructive cholestasis[J]. J Biol Chem, 2021, 297( 6): 101400. DOI: 10.1016/j.jbc.2021.101400. |
| [20] |
KIM YC, JUNG H, SEOK S, et al. MicroRNA-210 promotes bile acid-induced cholestatic liver injury by targeting mixed-lineage leukemia-4 methyltransferase in mice[J]. Hepatology, 2020, 71( 6): 2118- 2134. DOI: 10.1002/hep.30966. |
| [21] |
CHEN PC, HSU CP, WANG SY, et al. miR-194 up-regulates cholesterol 7 alpha-hydroxylase expression via β-catenin signaling and aggravates cholestatic liver diseases[J]. Am J Pathol, 2023, 193( 6): 755- 768. DOI: 10.1016/j.ajpath.2023.02.007. |
| [22] |
AFONSO MB, RODRIGUES PM, SIMÃO AL, et al. miRNA-21 ablation protects against liver injury and necroptosis in cholestasis[J]. Cell Death Differ, 2018, 25( 5): 857- 872. DOI: 10.1038/s41418-017-0019-x. |
| [23] |
NABIH ES, EL-KHARASHI OA. Targeting HMGB1/TLR4 axis and miR-21 by rosuvastatin: Role in alleviating cholestatic liver injury in a rat model of bile duct ligation[J]. Naunyn Schmiedebergs Arch Pharmacol, 2019, 392( 1): 37- 43. DOI: 10.1007/s00210-018-1560-y. |
| [24] |
KENNEDY LL, MENG FY, VENTER JK, et al. Knockout of microRNA-21 reduces biliary hyperplasia and liver fibrosis in cholestatic bile duct ligated mice[J]. Lab Invest, 2016, 96( 12): 1256- 1267. DOI: 10.1038/labinvest.2016.112. |
| [25] |
XIAO YT, WANG J, YAN WH, et al. Dysregulated miR-124 and miR-200 expression contribute to cholangiocyte proliferation in the cholestatic liver by targeting IL-6/STAT3 signalling[J]. J Hepatol, 2015, 62( 4): 889- 896. DOI: 10.1016/j.jhep.2014.10.033. |
| [26] |
SONG YF, TRAN M, WANG L, et al. miR-200c-3p targets SESN1 and represses the IL-6/AKT loop to prevent cholangiocyte activation and cholestatic liver fibrosis[J]. Lab Invest, 2022, 102( 5): 485- 493. DOI: 10.1038/s41374-021-00710-6. |
| [27] |
SANTOS AA, AFONSO MB, RAMIRO RS, et al. Host miRNA-21 promotes liver dysfunction by targeting small intestinal Lactobacillus in mice[J]. Gut Microbes, 2020, 12( 1): 1- 18. DOI: 10.1080/19490976.2020.1840766. |
| [28] |
CHIANG JYL. Bile acid metabolism and signaling[J]. Compr Physiol, 2013, 3( 3): 1191- 1212. DOI: 10.1002/cphy.c120023. |
| [29] |
VITALE G, MATTIACCIO A, CONTI A, et al. Molecular and clinical links between drug-induced cholestasis and familial intrahepatic cholestasis[J]. Int J Mol Sci, 2023, 24( 6): 5823. DOI: 10.3390/ijms24065823. |
| [30] |
STÄTTERMAYER AF, HALILBASIC E, WRBA F, et al. Variants in ABCB4(MDR3) across the spectrum of cholestatic liver diseases in adults[J]. J Hepatol, 2020, 73( 3): 651- 663. DOI: 10.1016/j.jhep.2020.04.036. |
| [31] |
NAYAGAM JS, WILLIAMSON C, JOSHI D, et al. Review article: Liver disease in adults with variants in the cholestasis-related genes ABCB11, ABCB4 and ATP8B1[J]. Aliment Pharmacol Ther, 2020, 52( 11-12): 1628- 1639. DOI: 10.1111/apt.16118. |
| [32] |
LIU HT, IROBALIEVA RN, KOWAL J, et al. Structural basis of bile salt extrusion and small-molecule inhibition in human BSEP[J]. Nat Commun, 2023, 14( 1): 7296. DOI: 10.1038/s41467-023-43109-1. |
| [33] |
WANG K, ZHANG YC, WANG GJ, et al. FXR agonists for MASH therapy: Lessons and perspectives from obeticholic acid[J]. Med Res Rev, 2024, 44( 2): 568- 586. DOI: 10.1002/med.21991. |
| [34] |
ANANTHANARAYANAN M, LI YF, SURAPUREDDI S, et al. Histone H3K4 trimethylation by MLL3 as part of ASCOM complex is critical for NR activation of bile acid transporter genes and is downregulated in cholestasis[J]. Am J Physiol Gastrointest Liver Physiol, 2011, 300( 5): G771- G781. DOI: 10.1152/ajpgi.00499.2010. |
| [35] |
XU D, YIN MJ, WANG YM, et al. Research progress on the regulation of FXR-CYP7A1 axis in cholestatic liver disease[J]. Chin J Integr Tradit West Med Liver Dis, 2021, 31( 5): 470- 473. DOI: 10.3969/j.issn.1005-0264.2021.05.025. |
| [36] |
|
| [37] |
HEIDARI R, NIKNAHAD H. The role and study of mitochondrial impairment and oxidative stress in cholestasis[J]. Methods Mol Biol, 2019, 1981: 117- 132. DOI: 10.1007/978-1-4939-9420-5_8. |
| [38] |
YANG HJ, LUO FY, WEI Y, et al. TGR5 protects against cholestatic liver disease via suppressing the NF-κB pathway and activating the Nrf2/HO-1 pathway[J]. Ann Transl Med, 2021, 9( 14): 1158. DOI: 10.21037/atm-21-2631. |
| [39] |
O’BRIEN KM, ALLEN KM, ROCKWELL CE, et al. IL-17A synergistically enhances bile acid-induced inflammation during obstructive cholestasis[J]. Am J Pathol, 2013, 183( 5): 1498- 1507. DOI: 10.1016/j.ajpath.2013.07.019. |
| [40] |
DAS K, RAO LVM. The role of microRNAs in inflammation[J]. Int J Mol Sci, 2022, 23( 24): 15479. DOI: 10.3390/ijms232415479. |
| [41] |
ZHANG YD, LIU Y, HUO W, et al. The role of miRNA and long noncoding RNA in cholestatic liver diseases[J]. Am J Pathol, 2024, 194( 6): 879- 893. DOI: 10.1016/j.ajpath.2024.02.006. |
| [42] |
ABDELFATTAH AM, MAHMOUD SS, EL-WAFAEY DI, et al. Diacerein ameliorates cholestasis-induced liver fibrosis in rat via modulating HMGB1/RAGE/NF-κB/JNK pathway and endoplasmic reticulum stress[J]. Sci Rep, 2023, 13( 1): 11455. DOI: 10.1038/s41598-023-38375-4. |
| [43] |
SALAS-SILVA S, SIMONI-NIEVES A, CHÁVEZ-RODRÍGUEZ L, et al. Mechanism of cholangiocellular damage and repair during cholestasis[J]. Ann Hepatol, 2021, 26: 100530. DOI: 10.1016/j.aohep.2021.100530. |
| [44] |
WOOLBRIGHT BL, JAESCHKE H. Inflammation and cell death during cholestasis: The evolving role of bile acids[J]. Gene Expr, 2019, 19( 3): 215- 228. DOI: 10.3727/105221619X15614873062730. |
| [45] |
DENG DJ, LI L, WANG CT, et al. Effect and mechanism of osthole on proliferation and apoptosis in human intrahepatic cholangiocarcinoma HuCCT1 cells[J]. Chin J Exp Tradit Med Formulae, 2023, 29( 20): 54- 60. DOI: 10.13422/j.cnki.syfjx.20222423. |
| [46] |
WANG JZ, LI WX, HUANG JF, et al. Expression of pan-TRK protein in intrahepatic cholangiocarcinoma and its correlation with Ki67[J]. Guangdong Med J, 2023, 44( 10): 1250- 1253. DOI: 10.13820/j.cnki.gdyx.20231879. |
| [47] |
ABE M, YOSHIDA T, AKIBA J, et al. STAT3 deficiency prevents hepatocarcinogenesis and promotes biliary proliferation in thioacetamide-induced liver injury[J]. World J Gastroenterol, 2017, 23( 37): 6833- 6844. DOI: 10.3748/wjg.v23.i37.6833. |
| [48] |
HAIDUROV A, ZHELTUKHIN AO, SNEZHKINA AV, et al. p53-regulated SESN1 and SESN2 regulate cell proliferation and cell death through control of STAT3[J]. Cell Commun Signal, 2025, 23( 1): 105. DOI: 10.1186/s12964-025-02104-3. |
| [49] |
ALPINI G, GLASER S, ALVARO D, et al. Bile acid depletion and repletion regulate cholangiocyte growth and secretion by a phosphatidylinositol 3-kinase-dependent pathway in rats[J]. Gastroenterology, 2002, 123( 4): 1226- 1237. DOI: 10.1053/gast.2002.36055. |
| [50] |
KAUR S, BANSAL Y, KUMAR R, et al. A panoramic review of IL-6: Structure, pathophysiological roles and inhibitors[J]. Bioorg Med Chem, 2020, 28( 5): 115327. DOI: 10.1016/j.bmc.2020.115327. |
| [51] |
FARDI F, KHASRAGHI LB, SHAHBAKHTI N, et al. An interplay between non-coding RNAs and gut microbiota in human health[J]. Diabetes Res Clin Pract, 2023, 201: 110739. DOI: 10.1016/j.diabres.2023.110739. |
| [52] |
LIU LS, WANG YL, YU SC, et al. Transforming growth factor beta promotes inflammation and tumorigenesis in Smad4-deficient intestinal epithelium in a YAP-dependent manner[J]. Adv Sci(Weinh), 2023, 10( 23): e2300708. DOI: 10.1002/advs.202300708. |
| [53] |
JIAN YP, YANG G, ZHANG LH, et al. Lactobacillus plantarum alleviates irradiation-induced intestinal injury by activation of FXR-FGF15 signaling in intestinal epithelia[J]. J Cell Physiol, 2022, 237( 3): 1845- 1856. DOI: 10.1002/jcp.30651. |
| [54] |
XU BL, CHENG Y, WEI Y. The role of competitive endogenous RNA in the development of cholangiocarcinoma[J]. J Clin Hepatol, 2022, 38( 11): 2659- 2662. DOI: 10.3969/j.issn.1001-5256.2022.11.044. |
| [55] |
SHI Y, PAN H. The expression and correlation of microRNA-221, microRNA-34a and microRNA-3614-5p in intrahepatic cholestasis of pregnancy[J]. Matern Child Health Care China, 2023, 38( 12): 2272- 2275. DOI: 10.19829/j.zgfybj.issn.1001-4411.2023.12.036. |






 DownLoad:
DownLoad: