铜死亡的发生机制及在肝脏疾病中的作用
DOI: 10.12449/JCH241131
-
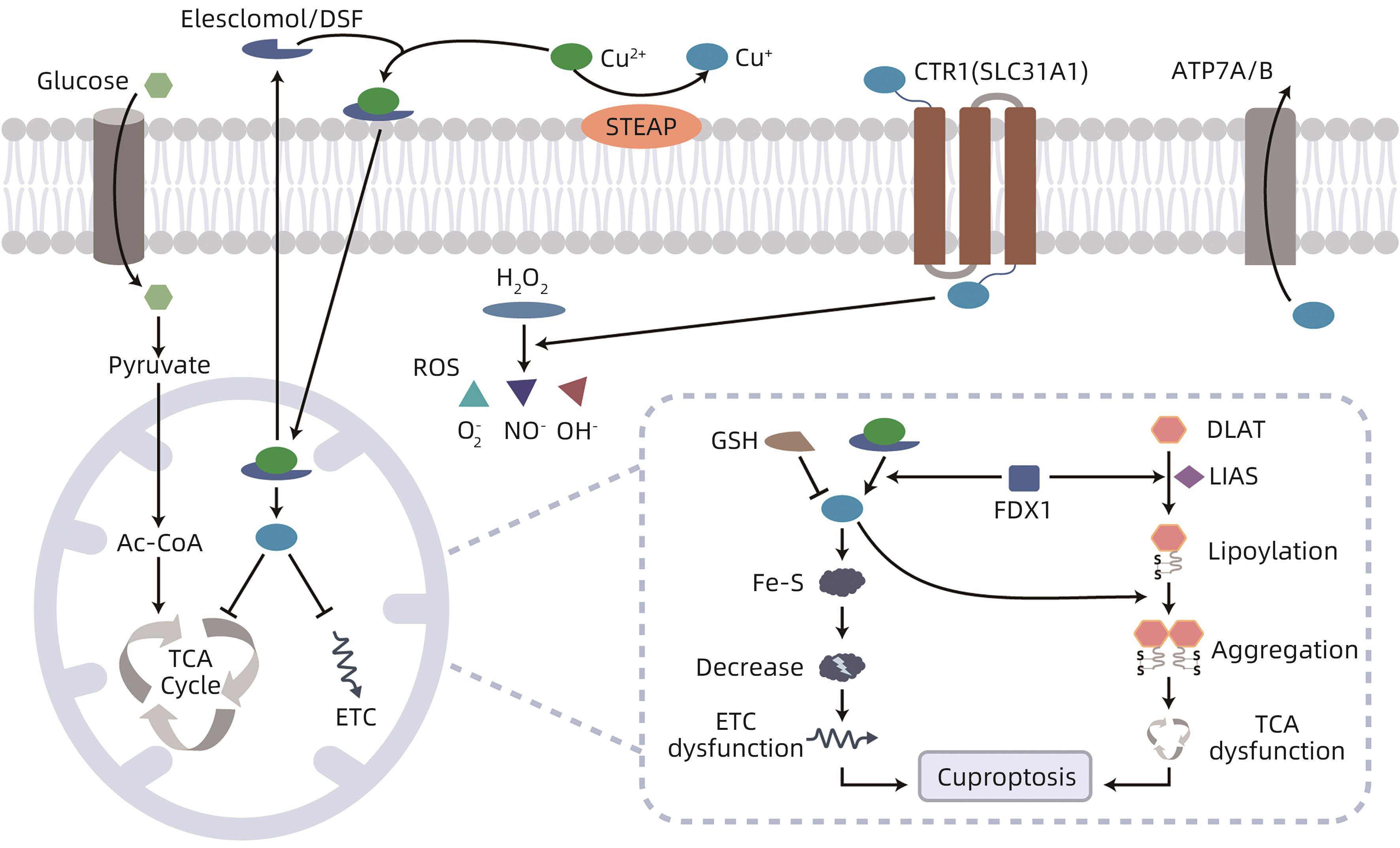
摘要: 铜死亡是依赖于细胞内铜积累触发线粒体脂酰化蛋白的聚集和铁硫簇蛋白不稳定的新型细胞死亡方式,其作用机制不同于自噬、铁死亡、细胞焦亡、坏死性凋亡等。铜死亡与肝癌发生及抗肿瘤药物耐药、遗传性肝脏疾病、非酒精性脂肪性肝病、病毒性肝炎和肝硬化等多种肝脏疾病的进展密切相关。本文总结了铜死亡的发生机制及在肝脏疾病中的作用和进展,旨在为肝脏疾病的进一步研究与治疗提供参考。Abstract: Cuproptosis is a new type of cell death that depends on intracellular copper accumulation to trigger the aggregation of mitochondrial lipoacylated protein and the degradation of iron-sulfur cluster protein, with a different mechanism of action from autophagy, ferroptosis, pyroptosis, and necroptosis. Cuproptosis is closely association with the development of liver cancer and resistance to antitumor drugs, as well as the progression of various liver diseases such as hereditary liver diseases, nonalcoholic fatty liver disease, viral hepatitis, and liver cirrhosis. This article summarizes the mechanism of cuproptosis and its role in liver diseases, in order to provide a reference for further research and treatment of liver diseases.
-
Key words:
- Copper /
- Cell Death /
- Liver Diseases
-
注: Glucose,葡萄糖;Pyruvate,丙酮酸;Ac-CoA,乙酰辅酶A;TCA Cycle,三羧酸循环;ETC,电子呼吸链;Elesclomol,伊利司莫;DSF,双硫仑;STEAP,前列腺六段跨膜上皮抗原;CTR1,铜转运蛋白1;ATP7A/B,铜转运ATP酶7A/B;H2O2,过氧化氢;ROS,活性氧;GSH,谷胱甘肽;Fe-S,Fe-S簇蛋白;FDX1,铁氧还蛋白1;DLAT,二氢硫辛酰S-乙酰转移酶;LIAS,硫辛酸合成酶;Lipoylation,脂酰化;Aggregation,寡聚化;Decrease,降解;ETC dys function,电子呼吸链紊乱。
图 1 铜死亡的分子机制
Figure 1. Schematic diagram of cuproptosis mechanism
-
[1] RUIZ LM, LIBEDINSKY A, ELORZA AA. Role of copper on mitochondrial function and metabolism[J]. Front Mol Biosci, 2021, 8: 711227. DOI: 10.3389/fmolb.2021.711227. [2] MICHNIEWICZ F, SALETTA F, ROUAEN JRC, et al. Copper: An intracellular Achilles’ heel allowing the targeting of epigenetics, kinase pathways, and cell metabolism in cancer therapeutics[J]. ChemMedChem, 2021, 16( 15): 2315- 2329. DOI: 10.1002/cmdc.202100172. [3] TSVETKOV P, COY S, PETROVA B, et al. Copper induces cell death by targeting lipoylated TCA cycle proteins[J]. Science, 2022, 375( 6586): 1254- 1261. DOI: 10.1126/science.abf0529. [4] SALEH SAK, ADLY HM, ABDELKHALIQ AA, et al. Serum levels of selenium, zinc, copper, manganese, and iron in prostate cancer patients[J]. Curr Urol, 2020, 14( 1): 44- 49. DOI: 10.1159/000499261. [5] CHEN J, JIANG YH, SHI H, et al. The molecular mechanisms of copper metabolism and its roles in human diseases[J]. Pflugers Arch, 2020, 472( 10): 1415- 1429. DOI: 10.1007/s00424-020-02412-2. [6] BRADY DC, CROWE MS, TURSKI ML, et al. Copper is required for oncogenic BRAF signalling and tumorigenesis[J]. Nature, 2014, 509( 7501): 492- 496. DOI: 10.1038/nature13180. [7] TURSKI ML, BRADY DC, KIM HJ, et al. A novel role for copper in Ras/mitogen-activated protein kinase signaling[J]. Mol Cell Biol, 2012, 32( 7): 1284- 1295. DOI: 10.1128/MCB.05722-11. [8] XU WJ, BARRIENTOS T, ANDREWS NC. Iron and copper in mitochondrial diseases[J]. Cell Metab, 2013, 17( 3): 319- 328. DOI: 10.1016/j.cmet.2013.02.004. [9] LILL R, FREIBERT SA. Mechanisms of mitochondrial iron-sulfur protein biogenesis[J]. Annu Rev Biochem, 2020, 89: 471- 499. DOI: 10.1146/annurev-biochem-013118-111540. [10] TANG DL, CHEN X, KROEMER G. Cuproptosis: A copper-triggered modality of mitochondrial cell death[J]. Cell Res, 2022, 32( 5): 417- 418. DOI: 10.1038/s41422-022-00653-7. [11] LI SR, BU LL, CAI LL. Cuproptosis: Lipoylated TCA cycle proteins-mediated novel cell death pathway[J]. Signal Transduct Target Ther, 2022, 7( 1): 158. DOI: 10.1038/s41392-022-01014-x. [12] FESTA RA, THIELE DJ. Copper: An essential metal in biology[J]. Curr Biol, 2011, 21( 21): R877- R883. DOI: 10.1016/j.cub.2011.09.040. [13] SAPORITO-MAGRIÑÁ CM, MUSACCO-SEBIO RN, ANDRIEUX G, et al. Copper-induced cell death and the protective role of glutathione: The implication of impaired protein folding rather than oxidative stress[J]. Metallomics, 2018, 10( 12): 1743- 1754. DOI: 10.1039/c8mt00182k. [14] XU JJ, JI L, RUAN YL, et al. UBQLN1 mediates sorafenib resistance through regulating mitochondrial biogenesis and ROS homeostasis by targeting PGC1β in hepatocellular carcinoma[J]. Signal Transduct Target Ther, 2021, 6( 1): 190. DOI: 10.1038/s41392-021-00594-4. [15] LELIÈVRE P, SANCEY L, COLL JL, et al. The multifaceted roles of copper in cancer: A trace metal element with dysregulated metabolism, but also a target or a bullet for therapy[J]. Cancers, 2020, 12( 12): 3594. DOI: 10.3390/cancers12123594. [16] LIAN WB, YANG PD, LI LQ, et al. A ceRNA network-mediated over-expression of cuproptosis-related gene SLC31A1 correlates with poor prognosis and positive immune infiltration in breast cancer[J]. Front Med, 2023, 10: 1194046. DOI: 10.3389/fmed.2023.1194046. [17] SHANBHAG VC, GUDEKAR N, JASMER K, et al. Copper metabolism as a unique vulnerability in cancer[J]. Biochim Biophys Acta Mol Cell Res, 2021, 1868( 2): 118893. DOI: 10.1016/j.bbamcr.2020.118893. [18] OLIVERI V. Selective targeting of cancer cells by copper ionophores: An overview[J]. Front Mol Biosci, 2022, 9: 841814. DOI: 10.3389/fmolb.2022.841814. [19] HUNSAKER EW, FRANZ KJ. Emerging opportunities to manipulate metal trafficking for therapeutic benefit[J]. Inorg Chem, 2019, 58( 20): 13528- 13545. DOI: 10.1021/acs.inorgchem.9b01029. [20] KANNAPPAN V, ALI MS, SMALL B, et al. Recent advances in repurposing disulfiram and disulfiram derivatives as copper-dependent anticancer agents[J]. Front Mol Biosci, 2021, 8: 741316. DOI: 10.3389/fmolb.2021.741316. [21] SKROTT Z, MISTRIK M, ANDERSEN KK, et al. Alcohol-abuse drug disulfiram targets cancer via p97 segregase adaptor NPL4[J]. Nature, 2017, 552( 7684): 194- 199. DOI: 10.1038/nature25016. [22] CHEN LY, MIN JX, WANG FD. Copper homeostasis and cuproptosis in health and disease[J]. Signal Transduct Target Ther, 2022, 7( 1): 378. DOI: 10.1038/s41392-022-01229-y. [23] BALDARI S, di ROCCO G, TOIETTA G. Current biomedical use of copper chelation therapy[J]. Int J Mol Sci, 2020, 21( 3): 1069. DOI: 10.3390/ijms21031069. [24] WANG YX, ZHU W, JIAO Y, et al. Research progress in regulatory effect of copper transporters on radiation injury and its mechanism[J]. J Jilin Univ Med Ed, 2023, 49( 4): 1076- 1082. DOI: 10.13481/j.1671-587X.20230432.王议贤, 朱巍, 焦旸, 等. 铜离子转运蛋白参与辐射损伤的调控作用及其机制的研究进展[J]. 吉林大学学报(医学版), 2023, 49( 4): 1076- 1082. DOI: 10.13481/j.1671-587X.20230432. [25] SCHILSKY ML. Wilson disease: Diagnosis, treatment, and follow-up[J]. Clin Liver Dis, 2017, 21( 4): 755- 767. DOI: 10.1016/j.cld.2017.06.011. [26] CHEN LJ, LIU DL, TAN YY. Research progress in cuproptosis in liver cancer[J]. J Cent South Univ Med Sci, 2023, 48( 9): 1368- 1376. DOI: 10.11817/j.issn.1672-7347.2023.230083.陈蕾洁, 刘德良, 谭玉勇. 铜死亡在肝癌中的研究进展[J]. 中南大学学报(医学版), 2023, 48( 9): 1368- 1376. DOI: 10.11817/j.issn.1672-7347.2023.230083. [27] SHAO SQ, SI JX, SHEN YQ. Copper as the target for anticancer nanomedicine[J]. Adv Ther, 2019, 2( 5): 1800147. DOI: 10.1002/adtp.201800147. [28] DAVIS CI, GU XX, KIEFER RM, et al. Altered copper homeostasis underlies sensitivity of hepatocellular carcinoma to copper chelation[J]. Metallomics, 2020, 12( 12): 1995- 2008. DOI: 10.1039/d0mt00156b. [29] GE EJ, BUSH AI, CASINI A, et al. Connecting copper and cancer: From transition metal signalling to metalloplasia[J]. Nat Rev Cancer, 2022, 22( 2): 102- 113. DOI: 10.1038/s41568-021-00417-2. [30] LI J. The molecular mechanism of Disulfiram/Copper complex(CuET) inhibiting proliferation and inducing apoptosis in hepatocellular carcinoma cells[D]. Chongqing: Army Medical University, 2021.黎婕. 双硫仑/铜复合物(CuET)抑制肝癌细胞增殖诱导细胞凋亡的分子机制研究[D]. 重庆: 中国人民解放军陆军军医大学, 2021. [31] LI Y, WANG LH, ZHANG HT, et al. Disulfiram combined with copper inhibits metastasis and epithelial-mesenchymal transition in hepatocellular carcinoma through the NF-κB and TGF-β pathways[J]. J Cell Mol Med, 2018, 22( 1): 439- 451. DOI: 10.1111/jcmm.13334. [32] CHIBA T, SUZUKI E, YUKI K, et al. Disulfiram eradicates tumor-initiating hepatocellular carcinoma cells in ROS-p38 MAPK pathway-dependent and-independent manners[J]. PLoS One, 2014, 9( 1): e84807. DOI: 10.1371/journal.pone.0084807. [33] REN XY, LI YC, ZHOU Y, et al. Overcoming the compensatory elevation of NRF2 renders hepatocellular carcinoma cells more vulnerable to disulfiram/copper-induced ferroptosis[J]. Redox Biol, 2021, 46: 102122. DOI: 10.1016/j.redox.2021.102122. [34] YANG M, WU XX, HU JL, et al. COMMD10 inhibits HIF1α/CP loop to enhance ferroptosis and radiosensitivity by disrupting Cu-Fe balance in hepatocellular carcinoma[J]. J Hepatol, 2022, 76( 5): 1138- 1150. DOI: 10.1016/j.jhep.2022.01.009. [35] GUTTMANN S, CHANDHOK G, GROBA SR, et al. Organic cation transporter 3 mediates cisplatin and copper cross-resistance in hepatoma cells[J]. Oncotarget, 2018, 9( 1): 743- 754. DOI: 10.18632/oncotarget.23142. [36] KELLAND L. The resurgence of platinum-based cancer chemotherapy[J]. Nat Rev Cancer, 2007, 7( 8): 573- 584. DOI: 10.1038/nrc2167. [37] SHANG YX, LUO MY, YAO FP, et al. Ceruloplasmin suppresses ferroptosis by regulating iron homeostasis in hepatocellular carcinoma cells[J]. Cell Signal, 2020, 72: 109633. DOI: 10.1016/j.cellsig.2020.109633. [38] SHAO JJ, LI MM, GUO ZJ, et al. TPP-related mitochondrial targeting copper(II) complex induces p53-dependent apoptosis in hepatoma cells through ROS-mediated activation of Drp1[J]. Cell Commun Signal, 2019, 17( 1): 149. DOI: 10.1186/s12964-019-0468-6. [39] JIN C, LI YJ, SU Y, et al. Novel copper complex CTB regulates methionine cycle induced TERT hypomethylation to promote HCC cells senescence via mitochondrial SLC25A26[J]. Cell Death Dis, 2020, 11( 10): 844. DOI: 10.1038/s41419-020-03048-x. [40] MENG Y, DONG BL, DONG XH, et al. Expressions of cuproptosis-related genes in hepatocellular carcinoma and their clinical significance[J]. Chin J Gen Surg, 2023, 32( 1): 74- 86. DOI: 10.7659/j.issn.1005-6947.2023.01.006.孟云, 董保龙, 董晓骅, 等. 铜死亡相关基因在肝细胞癌中的表达及其临床意义[J]. 中国普通外科杂志, 2023, 32( 1): 74- 86. DOI: 10.7659/j.issn.1005-6947.2023.01.006. [41] MA JJ, XIONG YQ, WANG B, et al. Construction and evaluation of prognostic model with cuproptosis-related lncRNA in hepatocellular carcinoma[J]. J Evid Based Med, 2023, 23( 3): 156- 168. DOI: 10.12019/j.issn.1671-5144.2023.03.004.马健钧, 熊永强, 王博, 等. 肝细胞癌铜死亡相关lncRNA预后模型的构建及评估[J]. 循证医学, 2023, 23( 3): 156- 168. DOI: 10.12019/j.issn.1671-5144.2023.03.004. [42] SHRIBMAN S, MARJOT T, SHARIF A, et al. Investigation and management of Wilson's disease: A practical guide from the British Association for the Study of the Liver[J]. Lancet Gastroenterol Hepatol, 2022, 7( 6): 560- 575. DOI: 10.1016/S2468-1253(22)00004-8. [43] GEROSA C, FANNI D, CONGIU T, et al. Liver pathology in Wilson’s disease: From copper overload to cirrhosis[J]. J Inorg Biochem, 2019, 193: 106- 111. DOI: 10.1016/j.jinorgbio.2019.01.008. [44] SANDAHL TD, LAURSEN TL, MUNK DE, et al. The prevalence of Wilson’s disease: An update[J]. Hepatology, 2020, 71( 2): 722- 732. DOI: 10.1002/hep.30911. [45] GUNJAN D, SHALIMAR, NADDA N, et al. Hepatocellular carcinoma: An unusual complication of longstanding Wilson disease[J]. J Clin Exp Hepatol, 2017, 7( 2): 152- 154. DOI: 10.1016/j.jceh.2016.09.012. [46] GU M, COOPER JM, BUTLER P, et al. Oxidative-phosphorylation defects in liver of patients with Wilson's disease[J]. Lancet, 2000, 356( 9228): 469- 474. DOI: 10.1016/s0140-6736(00)02556-3. [47] CHEN Y, JIANG YP. Metabolism of ceruloplasmin and clinical manifestation of hypoceruloplasminemia[J]. Chin J Clin Neurosci, 2006, 14( 1): 86- 89. DOI: 10.3969/j.issn.1008-0678.2006.01.020.陈嬿, 蒋雨平. 铜蓝蛋白的代谢和低铜蓝蛋白血症的临床表现[J]. 中国临床神经科学, 2006, 14( 1): 86- 89. DOI: 10.3969/j.issn.1008-0678.2006.01.020. [48] CHEN SR, CHONG YT, LI XH. Pathogenic mechanism and clinical diagnosis of hereditary abnormal copper metabolism[J]. J Clin Hepatol, 2019, 35( 8): 1667- 1672. DOI: 10.3969/j.issn.1001-5256.2019.08.003.陈淑如, 崇雨田, 李新华. 遗传性铜代谢异常的致病机制及临床诊断[J]. 临床肝胆病杂志, 2019, 35( 8): 1667- 1672. DOI: 10.3969/j.issn.1001-5256.2019.08.003. [49] OKAMOTO N, WADA S, OGA T, et al. Hereditary ceruloplasmin deficiency with hemosiderosis[J]. Hum Genet, 1996, 97( 6): 755- 758. DOI: 10.1007/BF02346185. [50] AIGNER E, STRASSER M, HAUFE H, et al. A role for low hepatic copper concentrations in nonalcoholic fatty liver disease[J]. Am J Gastroenterol, 2010, 105( 9): 1978- 1985. DOI: 10.1038/ajg.2010.170. [51] LIU T, LIU YL, ZHANG FY, et al. Association of copper metabolism disorder with cell damage and liver diseases[J]. J Clin Hepatol, 2023, 39( 9): 2244- 2251. DOI: 10.3969/j.issn.1001-5256.2023.09.032.柳涛, 刘雅丽, 张飞宇, 等. 铜代谢失调与细胞损伤及肝病的关系[J]. 临床肝胆病杂志, 2023, 39( 9): 2244- 2251. DOI: 10.3969/j.issn.1001-5256.2023.09.032. [52] ZHANG CY, YANG M. Current options and future directions for NAFLD and NASH treatment[J]. Int J Mol Sci, 2021, 22( 14): 7571. DOI: 10.3390/ijms22147571. [53] DEV S, MUCHENDITSI A, GOTTLIEB A, et al. Oxysterol misbalance critically contributes to Wilson disease pathogenesis[J]. Sci Adv, 2022, 8( 42): eadc9022. DOI: 10.1126/sciadv.adc9022. [54] TOSCO A, FONTANELLA B, DANISE R, et al. Molecular bases of copper and iron deficiency-associated dyslipidemia: A microarray analysis of the rat intestinal transcriptome[J]. Genes Nutr, 2010, 5( 1): 1- 8. DOI: 10.1007/s12263-009-0153-2. [55] LAN YQ, WU SL, WANG YH, et al. Association between blood copper and nonalcoholic fatty liver disease according to sex[J]. Clin Nutr, 2021, 40( 4): 2045- 2052. DOI: 10.1016/j.clnu.2020.09.026. [56] WU CT, LIU XX, ZHONG LX, et al. Identification of cuproptosis-related genes in nonalcoholic fatty liver disease[J]. Oxid Med Cell Longev, 2023, 2023: 9245667. DOI: 10.1155/2023/9245667. [57] MERAM I, SIRMATEL F, AHI S, et al. Plasma copper and zinc levels in chronic viral hepatitis[J]. Saudi Med J, 2004, 25( 8): 1066- 1069. [58] CESUR S, CEBECI SA, KAVAS GO, et al. Serum copper and zinc concentrations in patients with chronic hepatitis B[J]. J Infect, 2005, 51( 1): 38- 40. DOI: 10.1016/j.jinf.2004.08.012. [59] POZNAŃSKI J, SOŁDACKI D, CZARKOWSKA-PĄCZEK B, et al. Cirrhotic liver of liver transplant recipients accumulate silver and co-accumulate copper[J]. Int J Mol Sci, 2021, 22( 4): 1782. DOI: 10.3390/ijms22041782. [60] DASTYCH M, HUSOVÁ L, AIGLOVÁ K, et al. Manganese and copper levels in patients with primary biliary cirrhosis and primary sclerosing cholangitis[J]. Scand J Clin Lab Invest, 2021, 81( 2): 116- 120. DOI: 10.1080/00365513.2020.1864835. [61] WANG YQ, ZHOU Q, SHAO JG, et al. Bioinformatics analysis of Acute-on-chronic liver failure based on the expression of cuproptosis-related genes[J]. Mod Dig Interv, 2023, 28( 1): 50- 56. DOI: 10.3969/j.issn.1672-2159.2023.01.011.王艳秋, 周倩, 邵建国, 等. 基于铜死亡相关基因的慢加急性肝衰竭的机制研究[J]. 现代消化及介入诊疗, 2023, 28( 1): 50- 56. DOI: 10.3969/j.issn.1672-2159.2023.01.011. -



 PDF下载 ( 1108 KB)
PDF下载 ( 1108 KB)

 下载:
下载:


