全身炎症反应指数对慢加急性肝衰竭合并感染患者预后的预测价值
DOI: 10.12449/JCH250822
Clinical value of systemic inflammatory response index in patients with acute-on-chronic liver failure and co-infection
-
摘要:
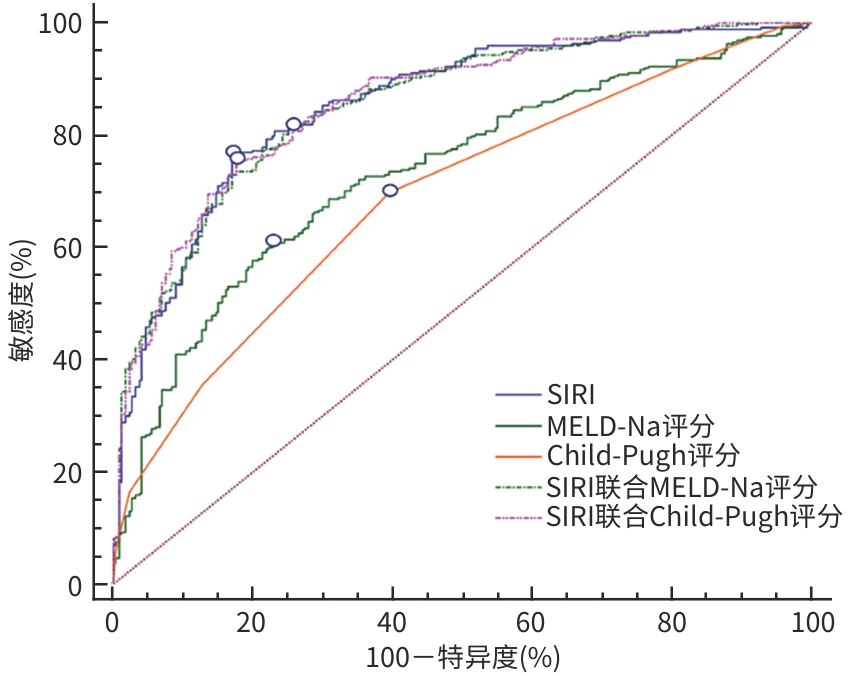
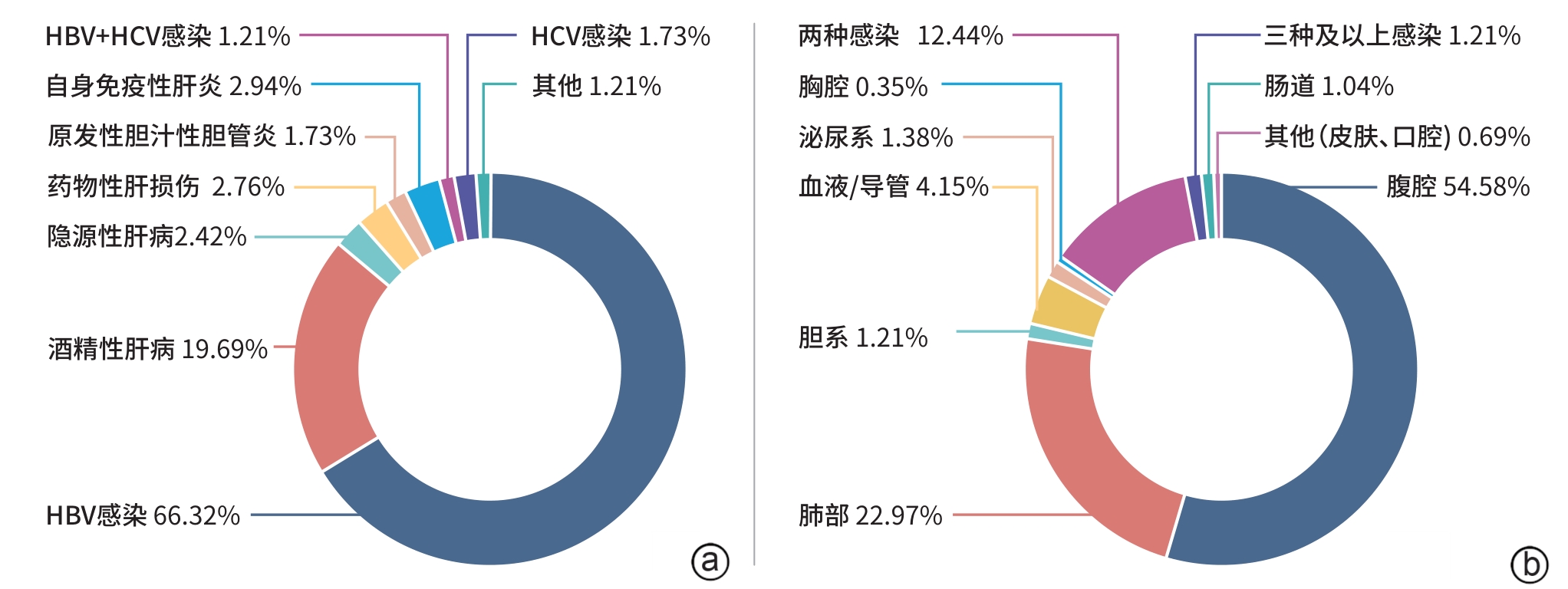
目的 探讨慢加急性肝衰竭(ACLF)合并感染患者的全身炎症反应指数(SIRI)指标在临床中的应用价值。 方法 回顾性分析2014年1月—2016年3月在中国人民解放军第五医学中心住院诊疗的579例ACLF合并感染患者的人口学特征、实验室指标、并发症等临床资料,计算SIRI值及MELD评分、MELD-Na评分和Child-Pugh评分,根据随访90 d的结果分为生存组(n=210)和死亡组(n=369)。符合正态分布的计量资料两组间比较采用成组t检验;非正态分布的计量资料两组间比较采用Mann-Whitney U秩和检验。计数资料两组间比较使用χ2检验。用二分类变量Logistic回归分析90 d死亡的独立危险因素。利用受试者操作特征曲线(ROC曲线)及ROC曲线下面积(AUC)分析SIRI、MELD-Na评分、Child-Pugh评分对ACLF合并感染患者预后的预测效能。根据SIRI的最佳截断值进行Kaplan-Meier生存分析。 结果 纳入的579例ACLF合并感染患者中,主要为HBV相关ACLF(384例,66.32%)和酒精性相关ACLF(114例,19.69%);腹腔(316例,54.58%)和肺部(133例,22.97%)为主要感染部位,90 d病死率为63.73%。多因素Logistic分析结果显示,SIRI(OR=1.177,95%CI:1.117~1.239)、血氨(OR=1.009,95%CI:1.001~1.018)、MELD-Na评分(OR=1.047,95%CI:1.016~1.080)、Child-Pugh评分(OR=1.351,95%CI:1.054~1.730)、年龄(OR=1.045,95%CI:1.021~1.070)、合并肝性脑病(OR=2.269,95%CI:1.305~3.946)、合并急性肾损伤(OR=1.730,95%CI:0.990~3.023)是ACLF合并感染患者90 d死亡的独立危险因素(P值均<0.05)。Pearson相关性分析显示,SIRI与MELD-Na评分(r=0.282)、Child-Pugh评分(r=0.168)均呈正相关(P值均<0.001)。SIRI、MELD-Na评分、Child-Pugh评分预测患者90 d死亡的ROC曲线下面积(AUC)分别为0.855、0.734、0.690,SIRI的预测效能高于MELD-Na评分、Child-Pugh评分(Z值分别为4.922、6.289,P值均<0.001),SIRI的敏感度为76.7%、特异度为82.9%。在SIRI联合MELD-Na评分、Child-Pugh评分后分别提高了MELD-Na评分(0.854 vs 0.734,Z=6.899,P<0.001)、Child-Pugh评分(0.858 vs 0.690,Z=8.725,P<0.001)的预测效能。高SIRI组(SIRI≥4.08)患者90 d生存率为11.29%(36/319),明显低于低SIRI组(SIRI<4.08)患者(χ2=225.24,P<0.001)。 结论 SIRI是ACLF合并感染患者死亡的独立危险因素,具有良好的临床预后预测价值,能更方便、经济实惠地应用于临床。 Abstract:Objective To investigate the application value of systemic inflammatory response index (SIRI) in patients with acute-on-chronic liver failure (ACLF) and co-infection. Methods A retrospective analysis was performed for the clinical data of 579 ACLF patients with co-infection who were diagnosed and treated in The Fifth Medical Center of Chinese PLA General Hospital from January 2014 to March 2016, including demographic features, laboratory markers, and complications, and SIRI, Model for End-Stage Liver Disease (MELD) score, MELD combined with serum sodium concentration (MELD-Na) score, and Child-Pugh score were calculated. According to the results of follow-up on day 90, the patients were divided into survival group with 210 patients and death group with 369 patients. The independent-samples t test was used for comparison of normally distributed continuous data between two groups; the Mann-Whitney U rank sum test was used for comparison of non-normally distributed continuous data between two groups; the chi-square test were used for comparison of categorical data between two groups. The binary logistic regression analysis was used to investigate the independent risk factors for 90-day death. The receiver operating characteristic (ROC) curve and the area under the ROC curve (AUC) were used to assess the performance of SIRI, MELD-Na score, and Child-Pugh score in predicting the prognosis of ACLF patients with co-infection. The Kaplan-Meier survival analysis was performed based on the optimal cut-off value of SIRI. Results Among the 597 ACLF patients with co-infection, 384 (66.32%) had HBV-related ACLF and 114 (19.69%) had alcohol-related ACLF; as for the main infection sites, 316 (54.58%) had abdominal infection and 133 (22.97%) had pulmonary infection; the 90-day mortality rate was 63.73%. The multivariate logistic regression analysis showed that SIRI (odds ratio [OR]=1.177, 95% confidence interval [CI]: 1.117 — 1.239, P<0.05), blood ammonia (OR=1.009, 95%CI: 1.001 — 1.018, P<0.05), MELD-Na score (OR=1.047, 95%CI: 1.016 — 1.080, P<0.05), Child-Pugh score (OR=1.351, 95%CI: 1.054 — 1.730, P<0.05), age (OR=1.045, 95%CI: 1.021 — 1.070, P<0.05), comorbidity with hepatic encephalopathy (OR=2.269, 95%CI: 1.305 — 3.946, P<0.05), and comorbidity with acute kidney injury (OR=1.730, 95%CI: 0.990 — 3.023, P<0.05) were independent risk factors for 90-day death in ACLF patients with co-infection. The Pearson correlation analysis showed that SIRI was positively correlated with MELD-Na score (r=0.282, P<0.001) and Child-Pugh score (r=0.168, P<0.001). SIRI, MELD-Na score, and Child-Pugh score had an AUC of 0.855, 0.734, and 0.690, respectively, in predicting 90-day death, and SIRI had a higher predictive efficiency than MELD-Na score and Child-Pugh score (Z=4.922 and 6.289, both P<0.001), with a sensitivity of 76.7% and a specificity of 82.9%. In addition, SIRI combined with MELD-Na score or Child-Pugh score improved the predictive efficiency of MELD-Na score (0.854 vs 0.734, Z=6.899, P<0.001) and Child-Pugh score (0.858 vs 0.690, Z=8.725, P<0.001). The patients with high SIRI (≥4.08) had a 90-day survival rate of 11.29% (36/319), which was significantly lower than that in the patients with low SIRI (<4.08) (χ2 =225.24, P<0.001). Conclusion SIRI is an independent risk factor for death in ACLF patients with co-infection and has a good clinical value in predicting prognosis, with the advantages of convenience and low costs. -
表 1 ACLF合并感染患者临床资料比较
Table 1. Comparison of clinical data of patients with ACLF co-infection
指标 总例数(n=579) 生存组(n=210) 死亡组(n=369) 统计值 P值 年龄(岁) 47.13±11.51 44.24±10.73 48.78±11.63 t=4.645 <0.001 男[例(%)] 476(82.21) 178(84.76) 298(80.76) χ2=1.466 0.226 病因[例(%)] χ2=4.182 0.124 HBV 384(66.32) 149(70.95) 235(63.69) 酒精性 114(19.69) 39(18.57) 75(20.33) 其他 81(13.99) 22(10.48) 59(15.99) 肝硬化[例(%)] 510(88.08) 186(88.57) 324(87.80) χ2=0.075 0.784 WBC(×109/L) 9.47(6.20~14.69) 7.06(5.06~11.04) 11.30(7.28~16.70) Z=-7.654 <0.001 NEU(×109/L) 7.25(4.36~12.05) 5.05(3.38~8.00) 9.01(5.65~14.19) Z=-8.515 <0.001 MON(×109/L) 0.70(0.43~1.13) 0.46(0.23~0.72) 0.91(0.60~1.34) Z=-11.312 <0.001 LYM(×109/L) 1.06(0.58~1.58) 1.37(0.87~1.90) 0.84(0.51~1.38) Z=-6.814 <0.001 Hb(g/L) 105.54±25.00 106.85±24.28 104.79±25.40 t=-0.954 0.341 PLT(×109/L) 69.00(43.00~102.00) 74.50(48.75~106.00) 66.00(40.00~101.00) Z=-1.882 0.060 Alb(g/L) 27.22±5.02 27.56±4.55 27.02±5.27 t=-1.234 0.218 TBil(μmol/L) 335.30±141.47 293.54±121.04 359.06±146.81 t=5.788 <0.001 ALT(U/L) 76.00(35.00~173.00) 60.00(29.00~121.75) 87.00(39.00~211.50) Z=-4.014 <0.001 AST(U/L) 118.50(68.00~227.25) 98.50(60.00~169.00) 134.50(78.25~284.75) Z=-4.784 <0.001 ALP(U/L) 146.00(114.00~187.00) 148.00(120.25~189.00) 143.00(110.25~187.75) Z=-0.944 0.345 GGT(U/L) 55.00(35.00~94.75) 50.50(36.25~93.25) 55.00(35.00~95.75) Z=-0.057 0.955 Cr(μmol/L) 100.00(80.00~145.00) 91.00(76.75~110.00) 112.00(85.00~176.50) Z=-6.476 <0.001 Na(mmol/L) 133.00(130.00~136.00) 134.00(131.00~136.00) 132.00(128.00~136.00) Z=-3.531 <0.001 GLU(mmol/L) 5.20(4.00~7.40) 4.80(3.70~6.10) 5.60(4.10~8.10) Z=-4.521 <0.001 BA(μmol/L) 133.00(130.00~136.00) 42.00(28.90~66.60) 64.35(41.92~103.23) Z=-7.062 <0.001 INR 1.99(1.69~2.44) 1.79(1.58~2.06) 2.16(1.79~2.82) Z=-8.831 <0.001 CRP(mg/L) 19.00(11.20~40.33) 18.50(10.73~36.73) 19.52(12.00~42.42) Z=-1.538 0.124 PCT(ng/mL) 0.97(0.51~1.92) 0.71(0.42~1.31) 1.17(0.57~2.50) Z=-5.493 <0.001 SIRI(×109/L) 5.60(1.89~13.55) 1.75(0.80~3.47) 9.52(4.41~20.27) Z=-14.197 <0.001 Child-Pugh评分(分) 11.00(10.00~12.00) 10.00(10.00~11.00) 11.00(10.00~12.00) Z=-7.868 <0.001 MELD评分(分) 25.66(21.67~30.62) 22.91(19.42~25.96) 28.46(23.42~33.55) Z=-9.575 <0.001 MELD-Na评分(分) 30.32(23.93~38.58) 25.34(21.21~30.73) 34.13(26.82~42.81) Z=-9.354 <0.001 感染后合并症 HE[例(%)] 277(47.84) 53(25.23) 224(60.70) χ2=67.464 <0.001 AKI[例(%)] 283(48.88) 53(25.23) 230(62.33) χ2=73.692 <0.001 上消化道出血[例(%)] 77(13.30) 12(5.71) 65(17.62) χ2=16.440 <0.001 表 2 ACLF合并感染患者Logistic多因素分析
Table 2. Multiple Logistic analysis of patients with ACLF co-infection
因素 B值 Wald P值 OR 95%CI SIRI 0.163 37.799 <0.001 1.177 1.117~1.239 PCT -0.012 0.344 0.558 0.988 0.949~1.028 ALT 0.000 0.004 0.951 1.000 0.999~1.001 AST 0.000 0.443 0.506 1.000 0.999~1.001 GLU 0.042 1.174 0.279 1.043 0.967~1.125 BA 0.009 4.363 0.037 1.009 1.001~1.018 MELD-Na评分 0.046 8.682 0.003 1.047 1.016~1.080 Child-Pugh评分 0.301 5.661 0.017 1.351 1.054~1.730 合并HE 0.819 8.427 0.004 2.269 1.305~3.946 合并AKI 0.548 3.702 0.012 1.730 0.990~3.023 合并上消化道出血 0.494 1.141 0.285 1.639 0.662~4.057 年龄 0.044 13.465 <0.001 1.045 1.021~1.070 表 3 不同评分模型对患者90 d死亡的预测效能比较
Table 3. Comparison of predictive performance of different scoring models for 90-day mortality in patients
指标 AUC(95%CI) 敏感度(%) 特异度(%) 截断值 SIRI 0.855(0.823~0.886) 76.7 82.9 4.08 MELD-Na评分 0.734(0.692~0.778) 61.0 77.1 30.98 Child-Pugh评分 0.690(0.645~0.734) 69.9 60.5 10.5 SIRI联合MELD-Na评分 0.854(0.823~0.885) 81.8 74.3 0.51 SIRI联合Child-Pugh评分 0.858(0.826~0.885) 75.6 82.4 0.57 -
[1] CASULLERAS M, ZHANG IW, LÓPEZ-VICARIO C, et al. Leukocytes, systemic inflammation and immunopathology in acute-on-chronic liver failure[J]. Cells, 2020, 9( 12): 2632. DOI: 10.3390/cells9122632. [2] LASHEN SA, SALEM P, IBRAHIM E, et al. Hematological ratios in patients with acute decompensation and acute-on-chronic liver failure: Prognostic factors[J]. Eur J Gastroenterol Hepatol, 2024, 36( 7): 952- 960. DOI: 10.1097/MEG.0000000000002782. [3] XI YM, LV CZ. Clinical study on the early prognosis of the systemic inflammatory response index in patients with sepsis[J]. Pract J Clin Med, 2024, 21( 3): 68- 72.习佑民, 吕传柱. 全身炎症反应指数对脓毒症患者早期预后的临床研究[J]. 实用医院临床杂志, 2024, 21( 3): 68- 72. [4] QI Q, ZHUANG LP, SHEN YH, et al. A novel systemic inflammation response index(SIRI) for predicting the survival of patients with pancreatic cancer after chemotherapy[J]. Cancer, 2016, 122( 14): 2158- 2167. DOI: 10.1002/cncr.30057. [5] CHAO B, JU XL, ZHANG LR, et al. A novel prognostic marker systemic inflammation response index(SIRI) for operable cervical cancer patients[J]. Front Oncol, 2020, 10: 766. DOI: 10.3389/fonc.2020.00766. [6] SUN W, FANG Y, ZHOU B, et al. The association of systemic inflammatory biomarkers with non-alcoholic fatty liver disease: A large population-based cross-sectional study[J]. Prev Med Rep, 2023, 37: 102536. DOI: 10.1016/j.pmedr.2023.102536. [7] YIN YF, ZHU WJ, XU QL. The systemic inflammation response index as a risk factor for hepatic fibrosis and long-term mortality among individuals with metabolic dysfunction-associated steatotic liver disease[J]. Nutr Metab Cardiovasc Dis, 2024, 34( 8): 1922- 1931. DOI: 10.1016/j.numecd.2024.04.018. [8] ZHANG SH, TANG ZN. Prognostic and clinicopathological significance of systemic inflammation response index in patients with hepatocellular carcinoma: A systematic review and meta-analysis[J]. Front Immunol, 2024, 15: 1291840. DOI: 10.3389/fimmu.2024.1291840. [9] CUI SP, CAO S, CHEN Q, et al. Preoperative systemic inflammatory response index predicts the prognosis of patients with hepatocellular carcinoma after liver transplantation[J]. Front Immunol, 2023, 14: 1118053. DOI: 10.3389/fimmu.2023.1118053. [10] Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, Chinese Medical Association; Severe Liver Disease and Artificial Liver Group, Chinese Society of Hepatology, Chinese Medical Association. Guideline for diagnosis and treatment of liver failure(2018)[J]. J Clin Hepatol, 2019, 35( 1): 38- 44. DOI: 10.3969/j.issn.1001-5256.2019.01.007.中华医学会感染病学分会肝衰竭与人工肝学组, 中华医学会肝病学分会重型肝病与人工肝学组. 肝衰竭诊治指南(2018年版)[J]. 临床肝胆病杂志, 2019, 35( 1): 38- 44. DOI: 10.3969/j.issn.1001-5256.2019.01.007. [11] Chinese Expert Consensus Compilation Group on Diagnosis and Treatment of Urinary Tract Infections. Chinese expert consensus on diagnosis and treatment of urinary tract infection(2015)[J]. Chin J Uro, 2015, 36( 4): 241- 248. DOI: 10.3760/cma.j.issn.1000-6702.2015.04.001.尿路感染诊断与治疗中国专家共识编写组. 尿路感染诊断与治疗中国专家共识(2015版)[J]. 中华泌尿外科杂志, 2015, 36( 4): 241- 248. DOI: 10.3760/cma.j.issn.1000-6702.2015.04.001. [12] Biliary Surgery Group, Surgery Branch of Chinese Medical Association. Diagnosis and treatment guidelines for acute biliary infection(2011 edition)[J]. Chin J Surg, 2011, 10( 1): 9- 13. DOI: 10.3760/cma.j.issn.1673-9752.2011.01.004.中华医学会外科学分会胆道外科学组. 急性胆道系统感染的诊断和治疗指南(2011版)[J]. 中华消化外科杂志, 2011, 10( 1): 9- 13. DOI: 10.3760/cma.j.issn.1673-9752.2011.01.004. [13] WONG F, PIANO S, SINGH V, et al. Clinical features and evolution of bacterial infection-related acute-on-chronic liver failure[J]. J Hepatol, 2021, 74( 2): 330- 339. DOI: 10.1016/j.jhep.2020.07.046. [14] LI H, SU HB, WANG YG, et al. Clinical predictive value of lactate on prognosis of patients with acute-on-chronic liver failure complicated with infection[J]. Chin J Hepatol, 2023, 31( 3): 300- 306. DOI: 10.3760/cma.j.cn501113-20230224-00077.李会, 苏海滨, 王永刚, 等. 乳酸对慢加急性肝衰竭合并感染患者预后的临床预测价值分析[J]. 中华肝脏病杂志, 2023, 31( 3): 300- 306. DOI: 10.3760/cma.j.cn501113-20230224-00077. [15] XUE R, YANG J, WU J, et al. Novel prognostic models for predicting the 180-day outcome for patients with hepatitis-B virus-related acute-on-chronic liver failure[J]. J Clin Transl Hepatol, 2021, 9( 4): 514- 520. DOI: 10.14218/JCTH.2021.00028. [16] LI JN, SUN MY, LI H, et al. Value of the monocyte-to-lymphocyte ratio in the prognostic evaluation of hepatitis B-related acute-on-chronic liver failure[J]. Chin J Hepatol, 2022, 30( 6): 644- 648. DOI: 10.3760/cma.j.cn501113-20210726-00361.李嘉妮, 孙梦滢, 李浩, 等. 单核细胞-淋巴细胞比率在乙型肝炎相关慢加急性肝衰竭预后评估中的价值[J]. 中华肝脏病杂志, 2022, 30( 6): 644- 648. DOI: 10.3760/cma.j.cn501113-20210726-00361. [17] SUN J, GUO HY, YU XP, et al. A neutrophil-to-lymphocyte ratio-based prognostic model to predict mortality in patients with HBV-related acute-on-chronic liver failure[J]. BMC Gastroenterol, 2021, 21( 1): 422. DOI: 10.1186/s12876-021-02007-w. [18] CHIRIAC S, STANCIU C, SINGEAP AM, et al. Prognostic value of neutrophil-to-lymphocyte ratio in cirrhotic patients with acute-on-chronic liver failure[J]. Turk J Gastroenterol, 2020, 31( 12): 868- 876. DOI: 10.5152/tjg.2020.19838. [19] LIU H, ZHANG H, WAN G, et al. Neutrophil-lymphocyte ratio: A novel predictor for short-term prognosis in acute-on-chronic hepatitis B liver failure[J]. J Viral Hepat, 2014, 21( 7): 499- 507. DOI: 10.1111/jvh.12160. [20] CAI JJ, WANG K, HAN T, et al. Evaluation of prognostic values of inflammation-based makers in patients with HBV-related acute-on-chronic liver failure[J]. Medicine(Baltimore), 2018, 97( 46): e13324. DOI: 10.1097/MD.0000000000013324. [21] BERNSMEIER C, CAVAZZA A, FATOUROU EM, et al. Leucocyte ratios are biomarkers of mortality in patients with acute decompensation of cirrhosis and acute-on-chronic liver failure[J]. Aliment Pharmacol Ther, 2020, 52( 5): 855- 865. DOI: 10.1111/apt.15932. -



 PDF下载 ( 1360 KB)
PDF下载 ( 1360 KB)

 下载:
下载: