不确定期慢性HBV感染者发生显著肝组织病理学损伤的危险因素分析
DOI: 10.12449/JCH251110
High-risk factors for significant liver histopathological damage in patients with indeterminate phase of chronic HBV infection
-
摘要:
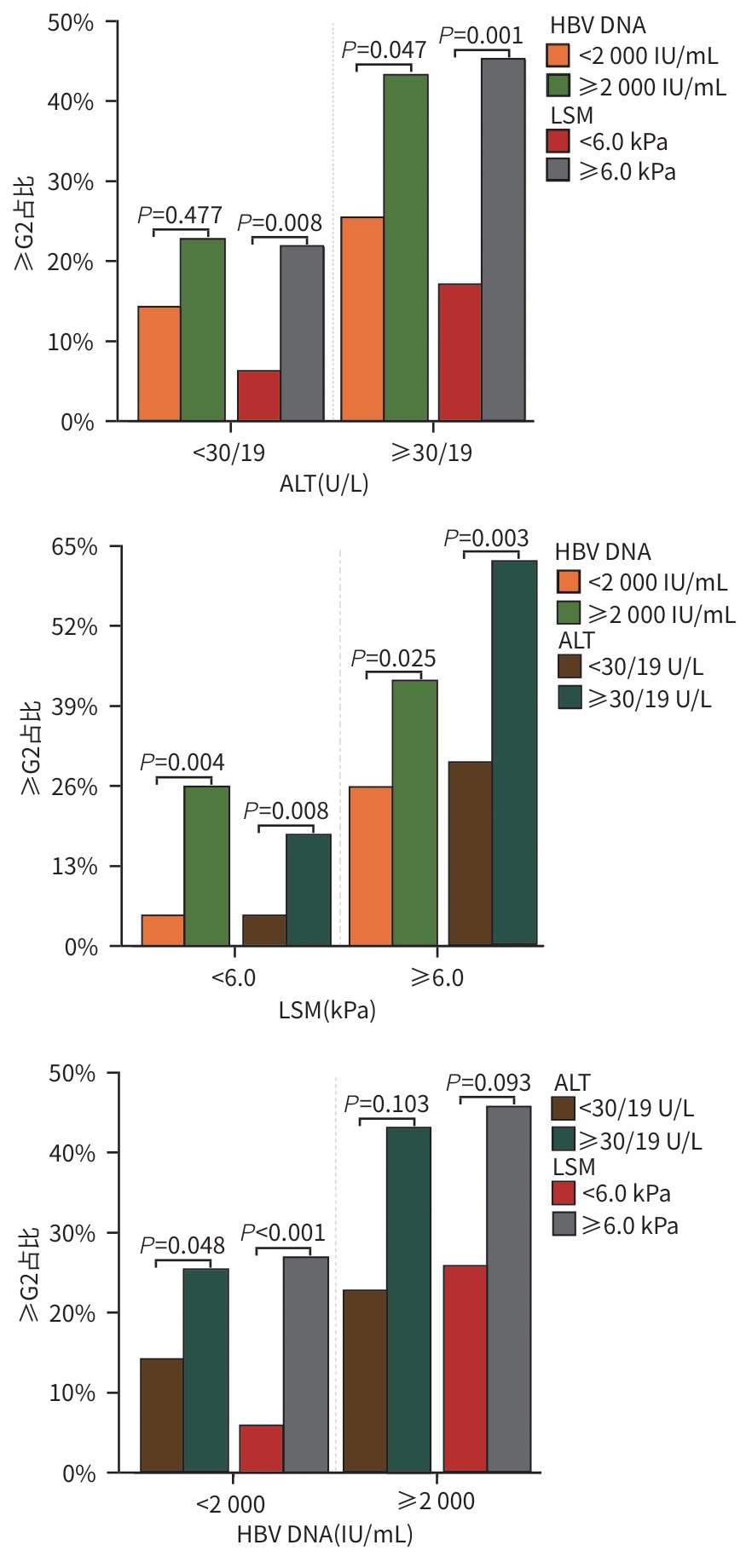
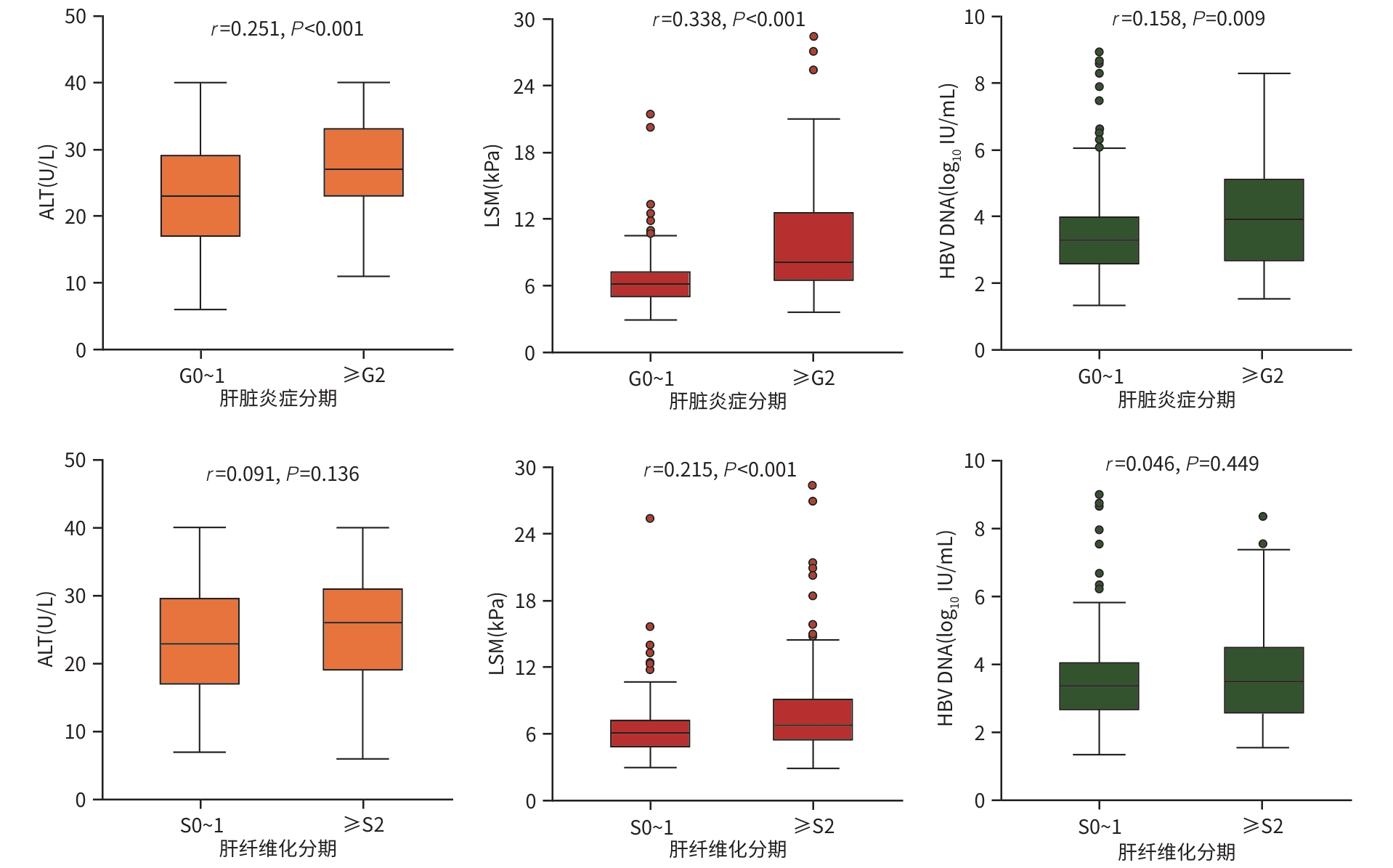
目的 分析不确定期慢性HBV感染者肝组织病理学损伤特点,探讨此类患者启动抗病毒治疗的时机。 方法 回顾性筛选2018年3月—2022年4月在中国人民解放军总医院第五医学中心住院并接受肝活检的慢性HBV感染者,纳入其中符合《慢性乙型肝炎防治指南(2022年版)》定义的不确定期者,收集其临床资料。肝组织病理学分期基于Scheuer标准,将炎症程度(G)分为0~4期,纤维化程度(S)分为0~4期,按照存在显著炎症(≥G2)及存在显著纤维化(≥S2)分别进行分组。正态分布的计量资料2组间比较采用成组t检验;非正态分布计量资料2组间比较采用Mann-Whitney U 检验;计数资料2组间比较采用χ2检验或Fisher确切概率法。采用Spearman秩相关分析探讨肝组织病理学与临床因素之间的关联,通过Logistic回归模型筛选显著炎症和肝纤维化的独立影响因素。 结果 共纳入271例不确定期慢性HBV感染者,61例(22.5%)存在显著炎症,124例(45.8%)存在显著肝纤维化。Logistic回归分析显示,ALT≥30/19 U/L(男/女)(OR=2.69, 95%CI:1.39~5.21,P=0.003)、HBV DNA≥2 000 IU/mL(OR=2.75, 95%CI:1.38~5.48,P=0.004)以及LSM≥6.0 kPa(OR=4.57, 95%CI:2.17~9.62,P<0.001)是显著炎症的独立风险因素。HBV DNA≥2 000 IU/mL(OR=1.82, 95%CI:1.01~3.32, P=0.049)以及LSM≥6.0 kPa(OR=2.06, 95%CI:1.23~3.43, P=0.006)是显著肝纤维化的独立影响因素。 结论 不确定期慢性HBV感染者中有较高比例的患者具有显著肝组织病理学改变,具有高危因素的患者需要及时启动抗病毒治疗。 Abstract:Objective To investigate the features of liver histopathological damage in patients with indeterminate phase of chronic HBV infection, as well as the timing for initiating antiviral therapy in such patients. Methods A retrospective screening was performed for the patients with chronic HBV infection who were hospitalized in The Fifth Medical Center of Chinese PLA General Hospital and underwent liver biopsy from March 2018 to April 2022, among whom the patients who met the criteria for indeterminate phase defined in Chinese guidelines for chronic hepatitis B prevention and treatment (2022 edition) were enrolled, and their clinical data were collected. Liver histopathological stage was determined using the Scheuer scoring system, with stages 0 — 4 for inflammation grade (G) and stages 0 — 4 for fibrosis degree (S), and the patients were divided into groups based on the presence of significant necroinflammation (≥G2) and significant liver fibrosis (≥S2). The independent samples t-test was used for comparison of normally distributed continuous data between two groups, and the Mann-Whitney U test was used for comparison of non-normally distributed continuous data between two groups; the chi-square test or the Fisher’s exact test was used for comparison of categorical data between two groups. A Spearman’s rank correlation analysis was used to investigate the correlation between liver histopathology and clinical factors, and the Logistic regression model was used to identify the independent influencing factors for significant necroinflammation and liver fibrosis. Results A total of 271 patients with indeterminate phase of chronic HBV infection were enrolled, among whom 61 (22.5%) had significant necroinflammation (≥G2) and 124 (45.8%) had significant liver fibrosis (≥S2). The Logistic regression analysis showed that alanine aminotransferase ≥30 U/L (for male patients) or ≥19 U/L (for female patients) (odds ratio [OR]=2.69, 95% confidence interval [CI]: 1.39 — 5.21, P=0.003), HBV DNA ≥2 000 IU/mL (OR=2.75, 95%CI: 1.38 — 5.48, P=0.004), and liver stiffness measurement (LSM) ≥6.0 kPa (OR=4.57, 95%CI: 2.17 — 9.62, P<0.001) were independent risk factors for significant inflammation. HBV DNA ≥2 000 IU/mL (OR=1.82, 95%CI: 1.01 — 3.32, P=0.049) and LSM ≥6.0 kPa (OR=2.06, 95%CI: 1.23 — 3.43, P=0.006) were independent influencing factors for significant liver fibrosis. Conclusion Among the patients with indeterminate phase of chronic HBV infection, a substantial proportion of patients have significant liver histopathological damage. Antiviral therapy should be initiated in a timely manner for patients with high-risk factors. -
Key words:
- Hepatitis B Virus /
- Inflammation /
- Hepatic Fibrosis /
- Indeterminate Phase
-
表 1 纳入患者按照肝脏炎症程度分组的一般特征
Table 1. General characteristics of enrolled patients grouped by the degree of hepatic inflammation
指标 总计(n=271) G0~1(n=210) ≥G2(n=61) 统计值 P值 男[例(%)] 171(63.1) 131(62.4) 40(65.6) χ2=0.21 0.649 年龄(岁) 41.0±10.6 41.3±10.1 39.8±12.2 t=0.90 0.371 HBV DNA(log10 IU/mL) 3.7±1.4 3.5±1.4 4.1±1.6 t=2.33 0.022 LSM (kPa) 6.2(5.1~8.0) 6.1(5.1~7.2) 8.1(6.5~12.5) Z=5.70 <0.001 ALT (U/L) 24.3±8.2 23.3±8.2 27.8±7.3 t=3.93 <0.001 AST (U/L) 24.7±7.9 22.9±5.9 30.9±10.4 t=5.74 <0.001 Alb (g/L) 41.2±2.7 41.4±2.6 41.0±3.0 t=0.89 0.377 PLT (×109/L) 178.5±56.3 182.6±54.3 164.2±61.1 t=2.27 0.024 表 2 纳入患者按照肝纤维化程度分组的一般特征
Table 2. General characteristics of the enrolled patients grouped by the degree of hepatic fibrosis
指标 S0~1(n=147) ≥S2(n=124) 统计值 P值 男[例(%)] 90(61.2) 81(65.3) χ2=0.49 0.486 年龄(岁) 40.8±10.1 41.2±11.1 t=0.30 0.765 HBV DNA(log10 IU/mL) 3.6±1.4 3.8±1.5 t=1.05 0.294 LSM (kPa) 6.1(4.9~7.3) 6.8(5.5~9.1) Z=3.53 <0.001 ALT (U/L) 23.7±8.3 25.0±8.0 t=1.34 0.181 AST (U/L) 24.3±8.5 25.2±7.1 t=0.99 0.323 Alb (g/L) 41.3±2.7 41.2±2.8 t=0.35 0.727 PLT (×109/L) 196.2±53.1 157.4±53.0 t=5.99 <0.001 表 3 显著肝组织病理学改变的单因素分析
Table 3. Univariate analysis of significant hepatic histopathological alterations
项目 肝脏显著炎症 显著肝纤维化 OR (95%CI) P值 OR(95%CI) P值 年龄 <30岁 1.00 1.00 30~39岁 0.51(0.22~1.18) 0.116 0.72(0.35~1.50) 0.386 ≥40岁 0.59(0.29~1.19) 0.142 1.05(0.56~1.99) 0.874 性别(男) 1.15(0.63~2.09) 0.649 1.17(0.68~2.01) 0.561 ALT(≥30/19 U/L) 2.61(1.45~4.68) 0.001 1.23(0.76~1.99) 0.405 HBV DNA(≥2 000 IU/mL) 2.59(1.40~4.80) 0.002 1.73(0.99~3.03) 0.055 LSM(≥6.0 kPa) 3.71(1.87~7.38) <0.001 2.02(1.23~3.31) 0.006 表 4 显著肝组织病理学改变的多因素分析
Table 4. Multivariate analysis of significant hepatic histopathological alterations
项目 肝脏显著炎症 显著肝纤维化 OR(95%CI) P值 OR(95%CI) P值 年龄 <30岁 1.00 1.00 30~39岁 0.50(0.20~1.24) 0.134 0.74(0.35~1.57) 0.435 ≥40岁 0.51(0.23~1.12) 0.095 1.07(0.55~2.06) 0.848 性别(男) 1.14(0.62~2.48) 0.538 1.17(0.68~2.01) 0.561 ALT(≥30/19 U/L) 2.69(1.39~5.21) 0.003 1.13(0.66~1.91) 0.663 HBV DNA(≥2 000 IU/mL) 2.75(1.38~5.48) 0.004 1.82(1.01~3.32) 0.049 LSM(≥6.0 kPa) 4.57(2.17~9.62) <0.001 2.06(1.23~3.43) 0.006 -
[1] JENG WJ, PAPATHEODORIDIS GV, LOK ASF. Hepatitis B[J]. Lancet, 2023, 401( 10381): 1039- 1052. DOI: 10.1016/S0140-6736(22)01468-4. [2] HUI CK, LEUNG N, YUEN ST, et al. Natural history and disease progression in Chinese chronic hepatitis B patients in immune-tolerant phase[J]. Hepatology, 2007, 46( 2): 395- 401. DOI: 10.1002/hep.21724. [3] European Association for the Study of the Liver. EASL 2017 clinical practice guidelines on the management of hepatitis B virus infection[J]. J Hepatol, 2017, 67( 2): 370- 398. DOI: 10.1016/j.jhep.2017.03.021. [4] WANG CY, YANG WC, TAN WH, et al. Value of a nomogram model in predicting significant liver injury in patients with immune-tolerant phase chronic hepatitis B[J]. J Clin Hepatol, 2021, 37( 7): 1529- 1533. DOI: 10.3969/j.issn.1001-5256.2021.07.010.王春艳, 杨武才, 谭文辉, 等. 慢性乙型肝炎免疫耐受期患者显著肝损伤的列线图模型及其预测价值分析[J]. 临床肝胆病杂志, 2021, 37( 7): 1529- 1533. DOI: 10.3969/j.issn.1001-5256.2021.07.010. [5] GAN QY, WANG JX, QIAN F, et al. Clinical and histological features of patients with chronic hepatitis B virus infection in the grey zone[J]. J Viral Hepat, 2023, 30( 10): 803- 809. DOI: 10.1111/jvh.13873. [6] ZHUANG H. Further discussion on the antiviral treatment of chronic hepatitis B patients with indeterminate phase[J]. J Clin Hepatol, 2023, 39( 10): 2273- 2276. DOI: 10.3969/j.issn.1001-5256.2023.10.001.庄辉. 不确定期慢性乙型肝炎抗病毒治疗再探讨[J]. 临床肝胆病杂志, 2023, 39( 10): 2273- 2276. DOI: 10.3969/j.issn.1001-5256.2023.10.001. [7] BRAVO AA, SHETH SG, CHOPRA S. Liver biopsy[J]. N Engl J Med, 2001, 344( 7): 495- 500. DOI: 10.1056/nejm200102153440706. [8] Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Infectious Diseases, Chinese Medical Association. Guidelines for the prevention and treatment of chronic hepatitis B[J]. Infect Dis Info, 2023, 36( 1): 1- 17. DOI: 10.3969/j.issn.1007-8134.2023.01.01.中华医学会肝病学分会, 中华医学会感染病学分会. 慢性乙型肝炎防治指南(2022年版)[J]. 传染病信息, 2023, 36( 1): 1- 17. DOI: 10.3969/j.issn.1007-8134.2023.01.01. [9] WONG GL, LEMOINE M. The 2024 updated WHO guidelines for the prevention and management of chronic hepatitis B: Main changes and potential implications for the next major liver society clinical practice guidelines[J]. J Hepatol, 2025, 82( 5): 918- 925. DOI: 10.1016/j.jhep.2024.12.004. [10] Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Gastroenterology, Chinese Medical Association; Chinese Society of Infectious Diseases, Chinese Medical Association. Consensus on the diagnosis and therapy of hepatic fibrosis(2019)[J]. J Clin Hepatol, 2019, 35( 10): 2163- 2172. DOI: 10.3969/j.issn.1001-5256.2019.10.007.中华医学会肝病学分会, 中华医学会消化病学分会, 中华医学会感染病学分会. 肝纤维化诊断及治疗共识(2019年)[J]. 临床肝胆病杂志, 2019, 35( 10): 2163- 2172. DOI: 10.3969/j.issn.1001-5256.2019.10.007. [11] Chinese Society of Hepatology and Chinese Society of Infectious Diseases, Chinese Medical Association. The guideline of prevention and treatment for chronic hepatitis B: a 2015 update[J]. J Clin Hepatol, 2015, 31( 12): 1941- 1960. DOI: 10.3969/j.issn.1001-5256.2015.12.002.中华医学会肝病学分会, 中华医学会感染病学分会. 慢性乙型肝炎防治指南(2015年更新版)[J]. 临床肝胆病杂志, 2015, 31( 12): 1941- 1960. DOI: 10.3969/j.issn.1001-5256.2015.12.002. [12] Chinese Foundation for Hepatitis Prevention and Control; Chinese Society of Infectious Disease and Chinese Society of Hepatology, Chinese Medical Association; Liver Disease Committee of Chinese Research Hospital Association. Consensus on clinical application of transient elastography detecting liver fibrosis: A 2018 update[J]. Chin J Hepatol, 2019, 27( 3): 182- 191. DOI: 10.3760/cma.j.issn.1007-3418.2019.03.004.中国肝炎防治基金会, 中华医学会感染病学分会, 中华医学会肝病学分会和中国研究型医院学会肝病专业委员会. 瞬时弹性成像技术诊断肝纤维化专家共识(2018年更新版)[J]. 中华肝脏病杂志, 2019, 27( 3): 182- 191. DOI: 10.3760/cma.j.issn.1007-3418.2019.03.004. [13] WANG H, RU GQ, YAN R, et al. Histologic disease in Chinese chronic hepatitis B patients with low viral loads and persistently normal alanine aminotransferase levels[J]. J Clin Gastroenterol, 2016, 50( 9): 790- 796. DOI: 10.1097/mcg.0000000000000544. [14] DUAN MH, CHI XL, XIAO HM, et al. High-normal alanine aminotransferase is an indicator for liver histopathology in HBeAg-negative chronic hepatitis B[J]. Hepatol Int, 2021, 15( 2): 318- 327. DOI: 10.1007/s12072-021-10153-2. [15] HUANG DQ, TRAN A, YEH ML, et al. Antiviral therapy substantially reduces HCC risk in patients with chronic hepatitis B infection in the indeterminate phase[J]. Hepatology, 2023, 78( 5): 1558- 1568. DOI: 10.1097/hep.0000000000000459. [16] ZENG Z, HAO HX, BI XY, et al. Study on liver histopathology of chronic HBV infected patients with different normal ALT values[J]. Front Immunol, 2022, 13: 1069752. DOI: 10.3389/fimmu.2022.1069752. [17] SONNEVELD MJ, BROUWER WP, HANSEN BE, et al. Very low probability of significant liver inflammation in chronic hepatitis B patients with low ALT levels in the absence of liver fibrosis[J]. Aliment Pharmacol Ther, 2020, 52( 8): 1399- 1406. DOI: 10.1111/apt.16067. [18] JUNG KS, KIM SU, AHN SH, et al. Risk assessment of hepatitis B virus–related hepatocellular carcinoma development using liver stiffness measurement(FibroScan)[J]. Hepatology, 2011, 53( 3): 885- 894. DOI: 10.1002/hep.24121. [19] TAN YW, YE Y, ZHOU XB, et al. Age as a predictor of significant fibrosis features in HBeAg-negative chronic hepatitis B virus infection with persistently normal alanine aminotransferase[J]. PLoS One, 2015, 10( 4): e0123452. DOI: 10.1371/journal.pone.0123452. [20] XU Y, LIU H, WANG Y, et al. The next step in controlling HBV in China[J]. BMJ, 2013, 347(jul16 1): f4503. DOI: 10.1136/bmj.f4503. [21] INDOLFI G, EASTERBROOK P, DUSHEIKO G, et al. Hepatitis B virus infection in children and adolescents[J]. Lancet Gastroenterol Hepatol, 2019, 4( 6): 466- 476. DOI: 10.1016/S2468-1253(19)30042-1. [22] LIAW YF, LAU GKK, KAO JH, et al. Hepatitis B e antigen seroconversion: A critical event in chronic hepatitis B virus infection[J]. Dig Dis Sci, 2010, 55( 10): 2727- 2734. DOI: 10.1007/s10620-010-1179-4. [23] ISOGAWA M, TANAKA Y. Immunobiology of hepatitis B virus infection[J]. Hepatol Res, 2015, 45( 2): 179- 189. DOI: 10.1111/hepr.12439. [24] WANG SH, CHEN PJ, YEH SH. Gender disparity in chronic hepatitis B: Mechanisms of sex hormones[J]. J Gastroenterol Hepatol, 2015, 30( 8): 1237- 1245. DOI: 10.1111/jgh.12934. [25] WU JF, SONG SH, LEE CS, et al. Clinical predictors of liver fibrosis in patients with chronic hepatitis B virus infection from children to adults[J]. J Infect Dis, 2018, 217( 9): 1408- 1416. DOI: 10.1093/infdis/jiy048. -



 PDF下载 ( 850 KB)
PDF下载 ( 850 KB)

 下载:
下载: