前白蛋白与总胆红素比值对HBV相关慢加急性肝衰竭患者短期预后的预测价值
DOI: 10.12449/JCH251112
Value of prealbumin-to-total bilirubin ratio in predicting the short-term prognosis of patients with HBV-related acute-on-chronic liver failure
-
摘要:
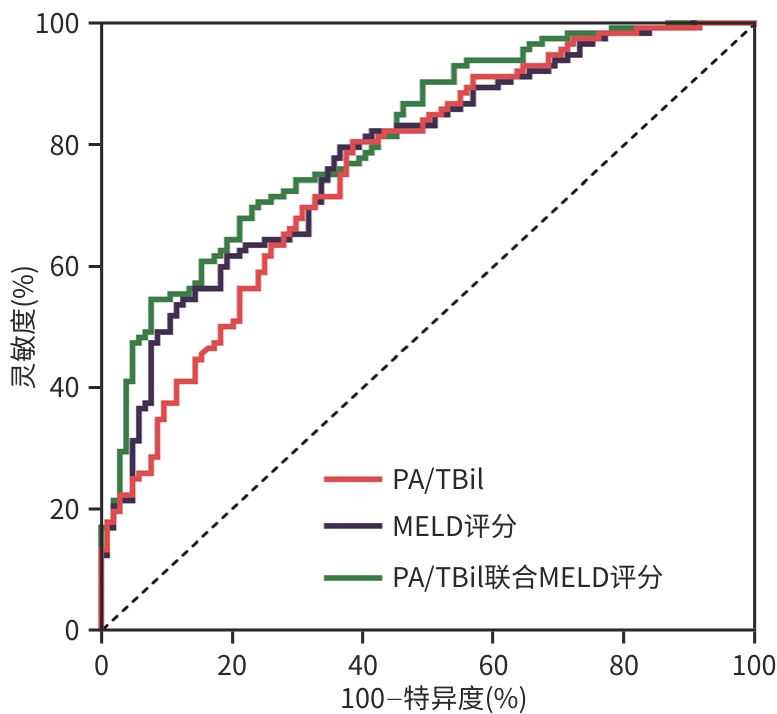
目的 评估入院时前白蛋白与总胆红素比值(PA/TBil)对HBV相关慢加急性肝衰竭(HBV-ACLF)患者90天死亡或肝移植的预测价值,并分析其与MELD评分联合后对短期预后预测效能的影响。 方法 回顾性分析2020年4月—2025年5月苏州大学附属第一医院感染病科收住入院的216例HBV-ACLF患者的临床资料,对患者随访3个月,根据结局将患者分为生存组(n=104)和死亡/移植组(n=112)。采用Kolmogorov-Smirnov检验分析计量资料是否符合正态分布,符合正态分布的计量资料两组间比较采用成组t检验,偏态资料两组间比较采用Mann-Whitney U检验;计数资料两组间比较采用χ2检验;采用单因素及多因素二元Logistic回归分析影响预后的因素;采用受试者操作特征曲线分析各指标对ACLF预后的预测效能,计算曲线下面积(AUC),并使用Delong检验对AUC进行比较。 结果 216例患者90天生存率为48.15%(104/216),生存组PLT、淋巴细胞计数、Alb、PA/TBil水平均显著高于死亡/移植组(P值均<0.05);年龄、WBC、中性粒细胞计数、PT、国际标准化比值、AST、TBil、肌酐、MELD评分均显著低于死亡/移植组(P值均<0.05)。多因素Logistic回归分析显示,年龄(OR=1.05,95%CI:1.02~1.09,P<0.001)、PA/TBil(OR=0.16,95%CI:0.05~0.46,P<0.001)、MELD评分(OR=1.09,95%CI:1.01~1.17,P=0.024)是HBV-ACLF患者90天预后的独立影响因素。PA/TBil、MELD评分及二者联合预测HBV-ACLF患者预后的AUC分别为0.760、0.779、0.811;PA/TBil联合MELD评分预测的AUC优于单一指标AUC(Z值分别为-2.058、2.017,P值均<0.05)。 结论 血清PA/TBil、MELD评分均可以有效预测HBV-ACLF患者的预后,二者联合对患者的预后预测效果明显优于单独使用MELD评分,这为临床风险分层管理和及时干预提供了重要参考。 Abstract:Objective To investigate the value of prealbumin-to-total bilirubin (PA/TBil) ratio on admission in predicting 90-day mortality or liver transplantation in patients with HBV-related acute-on-chronic liver failure (HBV-ACLF), as well as the effect of its combination with Model for End-Stage Liver Disease (MELD) score on the predictive performance for short-term prognosis. Methods A retrospective analysis was performed for the clinical data of 216 HBV-ACLF patients who were admitted to Department of Infectious Diseases in the First Affiliated Hospital of Soochow University from April 2020 to May 2025, and the patients were followed up for 3 months. According to the outcome, the patients were divided into survival group with 104 patients and death/transplantation group with 112 patients. The Kolmogorov-Smirnov test was used to check whether the continuous data was in accordance with the normal distribution; the two-independent-samples t test was used for comparison of normally distributed continuous data between two groups, while the Mann-Whitney U test was used for comparison of continuous data with skewed distribution between two groups. The chi-square test was used for comparison of categorical data between two groups. Univariate and multivariate binary Logistic regression analyses were used to investigate the influencing factors for prognosis, and the receiver operating characteristic (ROC) curve was used to analyze the performance of each indicator in predicting the prognosis of ACLF. The area under the ROC curve (AUC) was calculated, and the Delong test was used for comparison of AUC. Results A total of 216 patients were enrolled in this study, with a 90-day survival rate of 48.15% (104/216). Compared with the death/transplantation group, the survival group had significantly higher platelet count, lymphocyte count, albumin, and PA/TBil ratio (all P<0.05) and significantly lower age, white blood cell count, neutrophil count, prothrombin time, international normalized ratio, aspartate aminotransferase, total bilirubin, creatinine, and MELD score (all P<0.05). The multivariate Logistic regression analysis showed that age (odds ratio [OR]=1.05, 95% confidence interval [CI]: 1.02 — 1.09, P<0.001), PA/TBil ratio (OR=0.16, 95%CI: 0.05 — 0.46, P<0.001), and MELD score (OR=1.09, 95%CI: 1.01 — 1.17, P=0.024) were independent influencing factors for 90-day prognosis in HBV-ACLF patients. PA/TBil ratio and MELD score used alone or in combination had an AUC of 0.760, 0.779, and 0.811, respectively, in predicting the prognosis of HBV-ACLF patients, and PA/TBil ratio combined with MELD score had a better AUC than PA/TBil ratio or MELD score used alone (Z=-2.058 and 2.017, both P<0.05). Conclusion Both serum PA/TBil ratio and MELD score can effectively predict the prognosis of patients with HBV-ACLF, and a combination of the two indicators had a better predictive performance than MELD score alone, which provides an important reference for clinical risk stratification management and timely intervention. -
Key words:
- Hepatitis B Virus /
- Acute-on-Chronic Liver Failure /
- Prognosis /
- Prealbumin /
- Bilirubin /
- MELD Score
-
表 1 生存组和死亡/移植组HBV-ACLF患者的临床指标比较
Table 1. Comparison of clinical indicators between survival and death groups in HBV-ACLF patients
变量 合计(n=216) 生存组(n=104) 死亡/移植组(n=112) 统计值 P值 年龄(岁) 55.0(49.0~64.0) 53.0(45.5~61.0) 58.0(51.0~67.0) Z=-3.07 0.002 性别(男/女,例) 174/42 83/21 91/21 χ²=0.07 0.789 WBC(×109/L) 7.75(4.92~11.33) 7.31(4.77~9.29) 8.34(5.33~12.68) Z=-2.20 0.028 淋巴细胞计数(×109/L) 0.84(0.54~1.19) 0.93(0.75~1.29) 0.67(0.46~1.15) Z=-3.71 <0.001 中性粒细胞计数(×109/L) 5.95(3.56~9.20) 5.16(3.33~7.61) 7.09(3.79~10.84) Z=-3.07 0.002 PLT(×109/L) 76.50(48.75~131.00) 89.50(56.75~135.75) 66.50(38.75~107.75) Z=-2.97 0.003 Hb(g/L) 111.24±25.10 113.98±26.73 108.69±23.32 t=1.55 0.122 PT(s) 19.00(16.20~24.30) 18.10(15.85~21.68) 21.55(16.78~28.40) Z=-3.99 <0.001 INR 1.68(1.40~2.22) 1.59(1.36~1.89) 1.92(1.46~2.61) Z=-4.21 <0.001 ALT(U/L) 115.65(42.30~222.73) 99.20(34.83~306.50) 117.55(49.90~218.73) Z=-0.52 0.603 AST(U/L) 119.40(62.60~263.32) 88.50(55.08~216.90) 133.75(81.15~308.57) Z=-2.43 0.015 TBil(μmol/L) 194.95(86.97~365.97) 121.75(71.25~232.62) 284.65(147.75~439.70) Z=-6.06 <0.001 Alb(g/L) 30.01±5.33 31.41±5.15 28.72±5.19 t=3.83 <0.001 Cr(μmol/L) 65.05(52.70~88.00) 58.35(49.65~73.90) 76.05(56.10~99.80) Z=-4.29 <0.001 PA/TBil 0.19(0.09~0.45) 0.33(0.16~0.96) 0.13(0.05~0.24) Z=-6.59 <0.001 MELD评分(分) 13.17(7.80~18.61) 9.96(4.76~13.83) 16.31(12.50~22.74) Z=-7.09 <0.001 表 2 HBV-ACLF患者90天预后相关Logistic回归分析
Table 2. Logistic regression analysis of 90-day prognosis in HBV-ACLF patients
变量 单因素分析 多因素分析 β值 OR(95%CI) P值 β值 OR(95%CI) P值 年龄(岁) 0.04 1.04(1.01~1.06) 0.002 0.05 1.05(1.02~1.09) <0.001 WBC(×109/L) 0.06 1.06(1.01~1.12) 0.019 0.01 1.01(0.90~1.13) 0.877 淋巴细胞计数(×109/L) 0.02 1.02(0.91~1.14) 0.788 中性粒细胞计数(×109/L) 0.09 1.09(1.03~1.16) 0.005 0.04 1.04(0.92~1.18) 0.512 PLT(×109/L) -0.01 0.99(0.99~0.99) 0.018 0.00 1.00(0.99~1.00) 0.755 PT(s) 0.10 1.11(1.05~1.16) <0.001 -0.20 0.82(0.62~1.10) 0.189 INR 1.06 2.89(1.74~4.81) <0.001 2.04 7.72(0.45~131.90) 0.158 AST(U/L) 0.00 1.00(1.00~1.00) 0.620 TBil(μmol/L) 0.01 1.01(1.01~1.01) <0.001 Alb(g/L) -0.10 0.90(0.85~0.95) <0.001 -0.02 0.98(0.92~1.05) 0.640 Cr(μmol/L) 0.01 1.01(1.01~1.02) 0.001 PA/TBil -2.35 0.10(0.04~0.25) <0.001 -1.84 0.16(0.05~0.46) <0.001 MELD评分(分) 0.15 1.17(1.11~1.23) <0.001 0.08 1.09(1.01~1.17) 0.024 表 3 PA/TBil、MELD评分、PA/TBil联合MELD评分对90天预后的预测价值
Table 3. Comparison of predictive value for 90-day prognosis among PA/TBil, MELD score, and PA/TBil combined with MELD score
模型 AUC 95%CI 灵敏度(%) 特异度(%) Youden指数 Cut-off值 P值 PA/TBil 0.760 0.697~0.823 61.5 80.4 0.419 0.266 <0.001 MELD评分 0.779 0.719~0.840 79.5 63.5 0.430 12.000 <0.001 PA/TBil-MELD评分 0.811 0.755~0.867 67.9 79.8 0.477 0.596 <0.001 -
[1] ARROYO V, MOREAU R, JALAN R. Acute-on-chronic liver failure[J]. N Engl J Med, 2020, 382( 22): 2137- 2145. DOI: 10.1056/nejmra1914900. [2] PERRICONE G, ARTZNER T, de MARTIN E, et al. Intensive care management of acute-on-chronic liver failure[J]. Intensive Care Med, 2023, 49( 8): 903- 921. DOI: 10.1007/s00134-023-07149-x. [3] ZACCHERINI G, WEISS E, MOREAU R. Acute-on-chronic liver failure: Definitions, pathophysiology and principles of treatment[J]. JHEP Rep, 2021, 3( 1): 100176. DOI: 10.1016/j.jhepr.2020.100176. [4] SHI K, ZHANG Y, LI YQ, et al. High-density lipoprotein cholesterol as a prognostic marker for 90-day transplant-free mortality in hepatitis B virus-related acute-on-chronic liver failure[J]. Front Cell Infect Microbiol, 2024, 14: 1458818. DOI: 10.3389/fcimb.2024.1458818. [5] CAI Q, WANG H, ZHU MY, et al. Construction of a novel prognostic scoring model for HBV-ACLF liver failure based on dynamic data[J]. Sci Rep, 2024, 14( 1): 15198. DOI: 10.1038/s41598-024-63900-4. [6] HUANG ZW, ZHANG G, LIU J, et al. LRFNet: A deep learning model for the assessment of liver reserve function based on Child‐Pugh score and CT image[J]. Comput Meth Programs Biomed, 2022, 223: 106993. DOI: 10.1016/j.cmpb.2022.106993. [7] RUF A, DIRCHWOLF M, FREEMAN RB. From Child-Pugh to MELD score and beyond: Taking a walk down memory lane[J]. Ann Hepatol, 2022, 27( 1): 100535. DOI: 10.1016/j.aohep.2021.100535. [8] JOHNSON PJ, BERHANE S, KAGEBAYASHI C, et al. Assessment of liver function in patients with hepatocellular carcinoma: A new evidence-based approach-the ALBI grade[J]. J Clin Oncol, 2015, 33( 6): 550- 558. DOI: 10.1200/JCO.2014.57.9151. [9] LIAO YY, TENG CL, PENG NF, et al. Serum prealbumin is negatively associated with survival in hepatocellular carcinoma patients after hepatic resection[J]. J Cancer, 2019, 10( 13): 3006- 3011. DOI: 10.7150/jca.30903. [10] HUO RR, LIU HT, DENG ZJ, et al. Dose-response between serum prealbumin and all-cause mortality after hepatectomy in patients with hepatocellular carcinoma[J]. Front Oncol, 2020, 10: 596691. DOI: 10.3389/fonc.2020.596691. [11] YIN Y, CHENG JW, CHEN FY, et al. A novel preoperative predictive model of 90-day mortality after liver resection for huge hepatocellular carcinoma[J]. Ann Transl Med, 2021, 9( 9): 774. DOI: 10.21037/atm-20-7842. [12] DUAN RX, LIU L, WANG Y, et al. Prognostic value of combined detection of alpha-fetoprotein, plasma prothrombin activity, and serum prealbumin in acute-on-chronic liver failure[J]. World J Gastrointest Surg, 2025, 17( 2): 99531. DOI: 10.4240/wjgs.v17.i2.99531. [13] FAN WH, LIAO W, LUO YP, et al. Clinical prediction for outcomes of patients with acute-on-chronic liver failure associated with HBV infection: A new model establishment[J]. Open Med, 2020, 15( 1): 714- 722. DOI: 10.1515/med-2020-0207. [14] Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, Chinese Medical Association; Severe Liver Disease and Artificial Liver Group, Chinese Society of Hepatology, Chinese Medical Association. Guideline for diagnosis and treatment of liver failure(2018)[J]. J Clin Hepatol, 2019, 35( 1): 38- 44. DOI: 10.3969/j.issn.1001-5256.2019.01.007.中华医学会感染病学分会肝衰竭与人工肝学组, 中华医学会肝病学分会重型肝病与人工肝学组. 肝衰竭诊治指南(2018年版)[J]. 临床肝胆病杂志, 2019, 35( 1): 38- 44. DOI: 10.3969/j.issn.1001-5256.2019.01.007. [15] YE QX, HUANG JF, XU ZJ, et al. Short-term prognostic factors for hepatitis B virus-related acute-on-chronic liver failure[J]. World J Clin Cases, 2022, 10( 23): 8186- 8195. DOI: 10.12998/wjcc.v10.i23.8186. [16] KIM WR, MANNALITHARA A, HEIMBACH JK, et al. MELD 3.0: The model for end-stage liver disease updated for the modern era[J]. Gastroenterology, 2021, 161( 6): 1887- 1895. e 4. DOI: 10.1053/j.gastro.2021.08.050. [17] ARTRU F, TROVATO F, MORRISON M, et al. Liver transplantation for acute-on-chronic liver failure[J]. Lancet Gastroenterol Hepatol, 2024, 9( 6): 564- 576. DOI: 10.1016/S2468-1253(23)00363-1. [18] LAI M, XU MM, WANG X, et al. Prognostic evaluation of liver transplantation for acute-on-chronic liver failure[J]. Ogran Transplant, 2025, 16( 3): 482- 488. DOI: 10.12464/j.issn.1674-7445.2025002.赖曼, 徐曼曼, 王鑫, 等. 慢加急性肝衰竭肝移植预后评估[J]. 器官移植, 2025, 16( 3): 482- 488. DOI: 10.12464/j.issn.1674-7445.2025002. [19] ZHAO ZY, AN XQ, SHI L, et al. Prognostic value of serum prealbumin/total bilirubin ratio in patients with liver failure[J]. China J Mod Med, 2017, 27( 21): 75- 78. DOI: 10.3969/j.issn.1005-8982.2017.21.014.赵紫烟, 安雪青, 史丽, 等. 血清前白蛋白/总胆红素比值对肝衰竭患者预后的预测价值[J]. 中国现代医学杂志, 2017, 27( 21): 75- 78. DOI: 10.3969/j.issn.1005-8982.2017.21.014. [20] KURATA Y, MURAKI S, HIROTA T, et al. Effect of liver cirrhosis on theophylline trough concentrations: A comparative analysis of organ impairment using Child-Pugh and MELD scores[J]. Br J Clin Pharmacol, 2022, 88( 8): 3819- 3828. DOI: 10.1111/bcp.15333. [21] SHI JD, WANG PH, QI Z, et al. Expression of long non-coding RNA HOTAIR in acute liver injury and its intervention on cell ferroptosis and inflammation[J]. China Med, 2023, 18( 8): 1200- 1204. DOI: 10.3760/j.issn.1673-4777.2023.08.017.史敬东, 王鹏辉, 齐中, 等. 长链非编码RNA HOTAIR在急性肝损伤中的表达及其对细胞铁死亡及炎症发生的干预作用[J]. 中国医药, 2023, 18( 8): 1200- 1204. DOI: 10.3760/j.issn.1673-4777.2023.08.017. [22] GUO GY, YANG WT, LI J, et al. The development and appraisal of MELD 3.0 in liver diseases: Good things never come easy[J]. J Clin Transl Hepatol, 2025, 13( 1): 62- 68. DOI: 10.14218/JCTH.2024.00303. [23] CUI DG, XIAO LY, LIU YF, et al. The predictive value of CTP-MELD scores combined with serum M30 and M65 levels for the short-term prognosis of patients with hepatitis B-related acute-on-chronic liver failure[J]. Chin Hepatol, 2022, 27( 1): 58- 62. DOI: 10.14000/j.cnki.issn.1008-1704.2022.01.016.崔大广, 肖玲燕, 刘永福, 等. CTP-MELD评分联合血清M30和M65预测乙型肝炎相关慢加急性肝衰竭短期预后的价值[J]. 肝脏, 2022, 27( 1): 58- 62. DOI: 10.14000/j.cnki.issn.1008-1704.2022.01.016. [24] CHEN YQ, LI CY, TANG SH. Value of Δtotal bilirubin-alpha-fetoprotein scoring model in predicting the short-term prognosis of patients with hepatitis B virus-related acute-on-chronic liver failure[J]. J Clin Hepatol, 2024, 40( 12): 2399- 2405. DOI: 10.12449/JCH241209.陈雨琪, 李春燕, 汤善宏. Δ总胆红素-甲胎蛋白评分模型对HBV相关慢加急性肝衰竭短期预后的预测价值[J]. 临床肝胆病杂志, 2024, 40( 12): 2399- 2405. DOI: 10.12449/JCH241209. [25] LI WD, LIU WS, RONG YH, et al. Development and validation of a new prognostic model for predicting survival outcomes in patients with acute-on-chronic liver failure[J]. J Clin Transl Hepatol, 2024, 12( 10): 834- 844. DOI: 10.14218/jcth.2024.00316. [26] GAN YX, OUYANG LY, PAN YX, et al. Predictive value of ICGR15 and ALBI score for post-hepatectomy liver failure and prognosis of hepatocellular carcinoma patients after hepatic arterial infusion chemotherapy[J/OL]. Chin J Hepat Surg(Electronic Edition), 2025, 14( 3): 395- 401. DOI: 10.3877/cma.j.issn.2095-3232.2025.03.010.甘翌翔, 欧阳俐颖, 潘扬勋, 等. ICGR15和ALBI评分对肝动脉灌注化疗后肝癌肝切除术后肝衰竭和预后的预测价值[J/OL]. 中华肝脏外科手术学电子杂志, 2025, 14( 3): 395- 401. DOI: 10.3877/cma.j.issn.2095-3232.2025.03.010. [27] ZHANG H, YANG K, WANG Q, et al. Prealbumin as a predictor of short-term prognosis in patients with HBV-related acute-on-chronic liver failure[J]. Infect Drug Resist, 2023, 16: 2611- 2623. DOI: 10.2147/idr.s402585. [28] European Association for the Study of the Liver. EASL clinical practice guidelines on acute-on-chronic liver failure[J]. J Hepatol, 2023, 79( 2): 461- 491. DOI: 10.1016/j.jhep.2023.04.021. [29] CHEN XY, GAO FQ, PAN QL, et al. aCCI-HBV-ACLF: A novel predictive model for hepatitis B virus-related acute-on-chronic liver failure[J]. Aliment Pharmacol Ther, 2025, 61( 2): 286- 298. DOI: 10.1111/apt.18347. [30] LI C, WANG MD, SUN XD, et al. Development and validation of prealbumin-bilirubin score(preALBI score) for predicting long-term survival after hepatectomy for hepatocellular carcinoma: A multicenter analysis versus ALBI score[J]. Am J Surg, 2024, 232: 87- 94. DOI: 10.1016/j.amjsurg.2024.01.009. [31] TREBICKA J, HERNAEZ R, SHAWCROSS DL, et al. Recent advances in the prevention and treatment of decompensated cirrhosis and acute-on-chronic liver failure(ACLF) and the role of biomarkers[J]. Gut, 2024, 73( 6): 1015- 1024. DOI: 10.1136/gutjnl-2023-330584. [32] CHEN MJ, LI X, TANG SH. Research progress on multidimensional evaluation of liver function in the prognosis of liver failure patients[J]. Clin J Med Offic, 2023, 51( 9): 901- 903, 907. DOI: 10.16680/j.1671-3826.2023.09.05.陈美娟, 李雪, 汤善宏. 多维度评估肝功能在肝衰竭患者预后中研究进展[J]. 临床军医杂志, 2023, 51( 9): 901- 903, 907. DOI: 10.16680/j.1671-3826.2023.09.05. -



 PDF下载 ( 783 KB)
PDF下载 ( 783 KB)

 下载:
下载:


