基于倾向性评分匹配分析腹腔镜胆总管探查术后胆管不同引流方式对高龄胆总管结石患者的治疗效果
DOI: 10.12449/JCH251124
Therapeutic effect of different biliary drainage methods after laparoscopic common bile duct exploration in elderly patients with choledocholithiasis: An analysis based on propensity score matching
-
摘要:
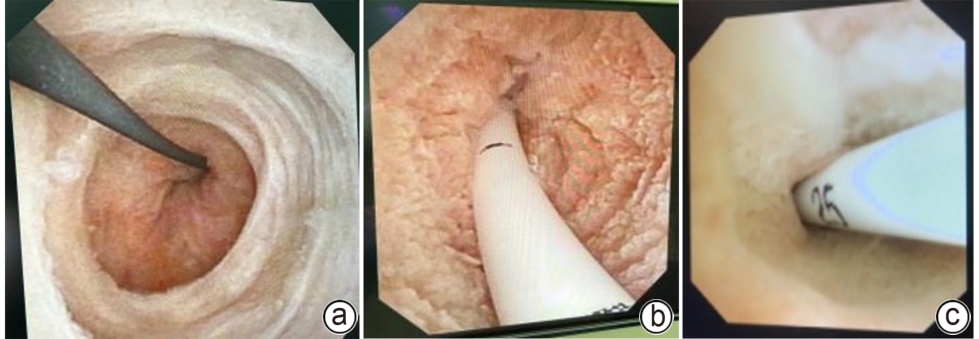
目的 评估腹腔镜胆总管探查术后留置胆道内引流管在高龄胆总管结石患者中的安全性、可行性,以期为临床治疗高龄胆总管结石病提供更多的术式选择。 方法 回顾性分析2021年11月—2024年10月大连医科大学附属大连市友谊医院肝胆外科收治的52例高龄胆总管结石患者的临床资料,根据术后胆管引流方式不同将患者分为留置内引流管组(n=24)和留置T管引流组(n=28),经倾向性评分匹配后两组各19例;比较两组围手术期指标和术后并发症之间的差异。计量资料两组间比较采用Wilcoxon秩和检验,计数资料两组间比较采用χ2检验或Fisher确切概率法。 结果 留置内引流管组术后住院时间短于留置T管引流组,胆汁丢失量少于留置T管引流组,差异均有统计学意义(Z值分别为-2.845,-5.633,P值均<0.05),两组在手术时间、术中出血量、引流管拔除时间方面,差异均无统计学意义(P值均>0.05)。两组在胆漏、结石残留、结石复发、胆管狭窄、引流管相关并发症发生率方面,差异均无统计学意义(P值均>0.05),但留置内引流管组的总并发症比例低于T管引流组(5.3%vs 36.8%),差异有统计学意义(P<0.05)。 结论 腹腔镜胆总管探查术后留置胆道内引流管在高龄胆总管结石患者中的应用,具有缩短术后住院时间、减少胆汁丢失、降低术后并发症发生率的趋势,可能有助于加快术后恢复。 Abstract:Objective To investigate the safety and feasibility of intra-biliary drainage tube placement after laparoscopic common bile duct exploration in elderly patients with choledocholithiasis, and to provide more options for surgical procedures in the clinical management of elderly patients with choledocholithiasis. Methods A retrospective analysis was performed for the clinical data of 52 elderly patients with choledocholithiasis who were admitted to Department of Hepatobiliary Surgery, Affiliated Dalian Friendship Hospital of Dalian Medical University, from November 2021 to October 2024. According to the biliary drainage method after surgery, the patients were divided into internal drainage group with 24 patients and T-tube drainage group with 28 patients, and there were 19 patients in each group after propensity score matching. The two groups were compared in terms of perioperative parameters and postoperative complications. The Wilcoxon rank-sum test was used for comparison of continuous data between two groups, and the chi-square test or the Fisher’s exact test was used for comparison of categorical data between two groups. Results Compared with the T-tube drainage group, the internal drainage group had a significantly shorter length of postoperative hospital stay and a significantly lower volume of postoperative bile loss (Z=-2.845 and -5.633, both P<0.05), while there were no significant differences between the two groups in time of operation, intraoperative blood loss, and drainage tube indwelling time (all P>0.05). There were no significant differences between the two groups in postoperative bile leak, stone recurrence, biliary stricture, and drainage tube-related complications, and the internal drainage group had a significantly lower total complication rate than the T-tube drainage group [1 (5.3%) vs 7 (36.8%), P<0.05]. Conclusion For elderly patients with choledocholithiasis, intra-biliary drainage tube placement after laparoscopic common bile duct exploration can shorten the length of postoperative hospital stay, reduce bile loss, and lower the incidence rate of postoperative complications, thereby helping to accelerate postoperative recovery. -
表 1 PSM前留置内引流管组和留置T管引流组胆总管结石患者一般资料比较
Table 1. Comparison of general data of patients with choledocholithiasis in the pre-PSM indwelling internal drainage tube group and the indwelling T tube group
项目 内引流管组(n=24) T管引流组(n=28) 统计值 P值 性别[例(%)] χ2=0.662 0.416 男 11(45.8) 16(57.1) 女 13(54.2) 12(42.9) 年龄(岁) 80.0(77.0~83.0) 78.5(76.0~82.0) Z=-1.024 0.306 合并胰腺炎[例(%)] 0.346 是 4(16.7) 8(28.6) 否 20(83.3) 20(71.4) ASA分级(级) 2.0(2.0~2.0) 2.0(1.0~2.0) Z=-1.777 0.076 白细胞计数(109/L) 9.3(6.1~12.4) 6.9(5.5~10.6) Z=-1.340 0.180 丙氨酸氨基转移酶(U/L) 191.5(97.5~316.2) 64.5(24.0~224.7) Z=-2.093 0.036 总胆红素(μmol/L) 53.0(32.4~80.3) 25.8(15.5~58.3) Z=-2.129 0.033 直接胆红素(μmol/L) 20.4(9.9~49.6) 11.0(5.4~21.3) Z=-2.157 0.031 胆总管直径(cm) 0.9(0.8~1.3) 1.2(1.0~1.5) Z=-2.101 0.036 胆总管结石数目[例(%)] χ2=0.030 0.862 单发 14(58.3) 17(60.7) 多发 10(41.7) 11(39.3) 表 2 PSM后内引流管组和T管引流组胆总管结石患者一般资料比较
Table 2. Comparison of general data of patients with choledocholithiasis in the internal drainage tube group and the T duct group after PSM
项目 内引流管组(n=19) T管引流组(n=19) 统计值 P值 性别[例(%)] χ2=2.661 0.103 男 8(42.1) 13(68.4) 女 11(57.9) 6(31.6) 年龄(岁) 80.0(77.0~83.0) 77.0(75.0~82.0) Z=-1.134 0.257 合并胰腺炎[例(%)] 0.232 是 2(10.5) 6(31.6) 否 17(89.5) 13(68.4) ASA分级(级) 2.0(2.0~2.0) 2.0(1.0~2.0) Z=-1.746 0.081 白细胞计数(109/L) 7.8(5.6~11.8) 6.6(5.5~10.6) Z=-0.803 0.422 丙氨酸氨基转移酶(U/L) 207.0(94.0~336.0) 115.0(32.0~244.0) Z=-1.445 0.148 总胆红素(μmol/L) 47.0(29.8~81.2) 48.0(21.2~79.1) Z=-0.511 0.609 直接胆红素(μmol/L) 19.7(9.6~36.2) 12.1(9.0~42.8) Z=-0.788 0.453 胆总管直径(cm) 1.0(0.9~1.5) 1.2(1.0~1.2) Z=-0.573 0.567 胆总管结石数目[例(%)] χ2=0.000 1.000 单发 12(63.2) 12(63.2) 多发 7(36.8) 7(36.8) 表 3 PSM后两组围手术期相关指标比较
Table 3. Comparison of perioperative indexes between the two groups after PSM
项目 内引流管组(n=19) T管引流组(n=19) Z值 P值 手术时间(min) 150.0(130.0~175.0) 165.0(145.0~210.0) -1.549 0.121 术中出血量(mL) 50.0(20.0~100.0) 50.0(50.0~100.0) -0.884 0.402 术后住院时间(d) 8.0(7.0~8.0) 11.0(8.0~12.0) -2.845 0.005 引流管拔除时间(d) 5.0(5.0~6.0) 7.0(4.0~9.0) -1.226 0.220 胆汁丢失量(mL) 0 384.6(320.2~452.2) -5.633 <0.001 表 4 PSM后两组术后相关并发症比较
Table 4. Comparison of postoperative related complications between the two groups after PSM
并发症 内引流管组
(n=19)
T管引流组
(n=19)
P值 胆漏[例(%)] >0.05 是 0(0.0) 1(5.3) 否 19(100.0) 18(94.7) 结石残留[例(%)] 0.230 是 0(0.0) 3(15.8) 否 19(100.0) 16(84.2) 引流管相关并发症[例(%)] >0.05 是 0(0.0) 1(5.3) 否 19(100.0) 18(94.7) 结石复发[例(%)] >0.05 是 1(5.3) 1(5.3) 否 18(94.7) 18(94.7) 胆管狭窄[例(%)] 0.230 是 0(0.0) 3(15.8) 否 19(100.0) 16(84.2) 总并发症[例(%)] 0.042 是 1(5.3) 7(36.8) 否 18(94.7) 12(63.2) -
[1] ZHAN ZL, HAN HC, ZHAO DB, et al. Primary closure after laparoscopic common bile duct exploration is feasible for elderly patients: 5-Year experience at a single institution[J]. Asian J Surg, 2020, 43( 1): 110- 115. DOI: 10.1016/j.asjsur.2019.04.009. [2] SONG Y, MA Y, XIE FC, et al. Age, gender, geographic and clinical differences for gallstones in China: A nationwide study[J]. Ann Transl Med, 2022, 10( 13): 735. DOI: 10.21037/atm-21-6186. [3] ZHU JS, TU SJ, YANG ZJ, et al. Laparoscopic common bile duct exploration for elderly patients with choledocholithiasis: A systematic review and meta-analysis[J]. Surg Endosc, 2020, 34( 4): 1522- 1533. DOI: 10.1007/s00464-020-07394-x. [4] CHEN JB, WEI SD, SUN JJ, et al. Clinical comparison of laparoscopic combined with choledochoscope and open surgery in the treatment of gallbladder and common bile duct stones in the elderly[J]. Chin J Geriatr, 2019, 38( 11): 1270- 1272. DOI: 10.3760/cma.j.issn.0254-9026.2019.11.019.陈建斌, 魏思东, 孙建军, 等. 腹腔镜联合胆道镜与开腹手术治疗老年胆囊及胆总管结石的临床对比[J]. 中华老年医学杂志, 2019, 38( 11): 1270- 1272. DOI: 10.3760/cma.j.issn.0254-9026.2019.11.019. [5] GAO C, WANG JY. The development and challenges of geriatric surgery[J]. Chin J Geriatr, 2024, 43( 11): 1392- 1395. DOI: 10.3760/cma.j.issn.0254-9026.2024.11.003.高超, 王建业. 老年外科学的发展与挑战[J]. 中华老年医学杂志, 2024, 43( 11): 1392- 1395. DOI: 10.3760/cma.j.issn.0254-9026.2024.11.003. [6] LI CX, LI XM, LIANG ZQ, et al. Application of indocyanine green fluorescence navigation in laparoscopic cholecystectomy after percutaneous transhepatic gallbladder drainage in elderly patients with acute cholecystitis[J]. J Clin Hepatol, 2023, 39( 4): 885- 891. DOI: 10.3969/j.issn.1001-5256.2023.04.020.李昌旭, 李学民, 梁占强, 等. 吲哚菁绿荧光导航在老年急性胆囊炎患者经皮经肝胆囊穿刺引流术后腹腔镜胆囊切除术中的应用[J]. 临床肝胆病杂志, 2023, 39( 4): 885- 891. DOI: 10.3969/j.issn.1001-5256.2023.04.020. [7] ZHANG ZH, SHAO GH, LI YY, et al. Efficacy and safety of laparoscopic common bile duct exploration with primary closure and intraoperative endoscopic nasobiliary drainage for choledocholithiasis combined with cholecystolithiasis[J]. Surg Endosc, 2023, 37( 3): 1700- 1709. DOI: 10.1007/s00464-022-09601-3. [8] MA XH, CAI SB. The outcome and safety in laparoscopic common bile duct exploration with primary suture versus T-tube drainage: A meta-analysis[J]. Appl Bionics Biomech, 2023, 2023( 1): 7300519. DOI: 10.1155/2023/7300519. [9] XU YK, DONG CY, MA KX, et al. Spontaneously removed biliary stent drainage versus T-tube drainage after laparoscopic common bile duct exploration[J]. Medicine, 2016, 95( 39): e5011. DOI: 10.1097/md.0000-000000005011. [10] DONG HZ, LIU X, LUO MJ, et al. Application of an internal drainage tube in laparoscopic common bile duct exploration[J]. Med Int, 2021, 1( 4): 14. DOI: 10.3892/mi.2021.14. [11] DU KF, WANG XC, WEI L, et al. Clinical efficacy of intra-biliary drainage versus T-tube drainage following laparoscopic common bile duct exploration[J]. Chin J Hepatobiliary Surg, 2023, 29( 10): 732- 736. DOI: 10.3760/cma.j.cn113884-20230618-00172.杜开放, 王希春, 魏磊, 等. 腹腔镜下胆总管探查术放置内引流管与放置T管的临床疗效分析[J]. 中华肝胆外科杂志, 2023, 29( 10): 732- 736. DOI: 10.3760/cma.j.cn113884-20230618-00172. [12] WU PH, YU MW, CHUANG SC, et al. Comparison of laparoscopic common bile duct exploration plus cholecystectomy and endoscopic retrograde cholangiopancreatography followed by laparoscopic cholecystectomy for elderly patients with common bile duct stones and gallbladder stones[J]. J Gastrointest Surg, 2024, 28( 5): 719- 724. DOI: 10.1016/j.gassur.2024.02.026. [13] SUWATTHANARAK T, CHINSWANGWATANAKUL V, METHASATE A, et al. Surgical strategies for challenging common bile duct stones in the endoscopic era: A comprehensive review of current evidence[J]. World J Gastrointest Endosc, 2024, 16( 6): 305- 317. DOI: 10.4253/wjge.v16.i6.305. [14] APREA G, CANFORA A, FERRONETTI A, et al. Morpho-functional gastric pre-and post-operative changes in elderly patients undergoing laparoscopic cholecystectomy for gallstone related disease[J]. BMC Surg, 2012, 12( Suppl 1): S5. DOI: 10.1186/1471-2482-12-S1-S5. [15] ZANG JF, YUAN Y, ZHANG C, et al. Laparoscopic management after failed endoscopic stone removal in nondilated common bile duct[J]. Int J Surg, 2016, 29: 49- 52. DOI: 10.1016/j.ijsu.2016.03.037. [16] RENDELL VR, PAULI EM. Laparoscopic common bile duct exploration[J]. JAMA Surg, 2023, 158( 7): 766. DOI: 10.1001/jamasurg.2022.8141. [17] LI ZQ, SUN JX, LI B, et al. Meta-analysis of single-stage versus two-staged management for concomitant gallstones and common bile duct stones[J]. J Min Access Surg, 2020, 16( 3): 206. DOI: 10.4103/jmas.jmas_146_18. [18] FAN LL, WANG Y, WU ML, et al. Laparoscopic common bile duct exploration with primary closure could be safely performed among elderly patients with choledocholithiasis[J]. BMC Geriatr, 2023, 23( 1): 486. DOI: 10.1186/s12877-023-04149-w. [19] XIE WC, YU WD, ZHANG Z, et al. Is T-tube drainage no longer needed for laparoscopic common bile duct exploration? A retrospective analysis and literature review[J]. Videosurgery Other Miniinvasive Tech, 2022: 99- 107. DOI: 10.5114/wiitm.2022.120727. [20] ZHANG TX, LYU YF, ZHENG JF. Advances in minimally invasive treatment for choledocholithiasis[J/OL]. Chin J Hepat Surg(Electronic Edition), 2023, 12( 5): 585- 588. DOI: 10.3877/cma.j.issn.2095-3232.2023.05.022.张天献, 吕云福, 郑进方. 胆总管结石微创治疗进展[J/OL]. 中华肝脏外科手术学电子杂志, 2023, 12( 5): 585- 588. DOI: 10.3877/cma.j.issn.2095-3232.2023.05.022. [21] LYON M, MENON S, JAIN A, et al. Use of biliary stent in laparoscopic common bile duct exploration[J]. Surg Endosc, 2015, 29( 5): 1094- 1098. DOI: 10.1007/s00464-014-3797-y. [22] LA PV, LE HT, TRAN TM, et al. Primary closure compared with T-tube drainage following laparoscopic common bile duct exploration among elderly patients with hepatolithiasis and/or choledocholithiasis: A comparative study using a propensity score matching[J]. HPB, 2025, 27( 2): 232- 239. DOI: 10.1016/j.hpb.2024.11.004. [23] TANG CN, TAI CK, HA JP, et al. Antegrade biliary stenting versus T-tube drainage after laparoscopic choledochotomy--a comparative cohort study[J]. Hepatogastroenterology, 2006, 53( 69): 330- 334. [24] RUDIMAN R, HANAFI RV, ALMAWIJAYA, et al. Complications of biliary stenting versus T-tube insertion after common bile duct exploration: A systematic review and meta-analysis[J]. PLoS One, 2023, 18( 1): e0280755. DOI: 10.1371/journal.pone.0280755. [25] CORAZZIARI E. Sphincter of Oddi dysfunction[J]. Dig Liver Dis, 2003, 35 Suppl 3: S26- S29. DOI: 10.1016/s1590-8658(03)00090-2. [26] ELSEBAEY MA, ENABA ME, ELASHRY H, et al. Forgotten biliary plastic stents: complications, management, and clinical outcomes[J]. Medicina(Kaunas), 2024, 60( 8): 1258. DOI: 10.3390/medicina60081258. [27] SHI TT, LIU ZQ, YUAN HB, et al. Application of propensity score matching in non-randomized controlled studies[J]. Chin J Health Statistics, 2021, 38( 2): 312- 314. DOI: 10.3969/j.issn.1002-3674.2021.02.040.施婷婷, 刘振球, 袁黄波, 等. 倾向性评分匹配法在非随机对照研究中的应用[J]. 中国卫生统计, 2021, 38( 2): 312- 314. DOI: 10.3969/j.issn.1002-3674.2021.02.040. -



 PDF下载 ( 6943 KB)
PDF下载 ( 6943 KB)


 下载:
下载: