肝性骨病对肝移植术预后的影响
DOI: 10.12449/JCH251135
利益冲突声明:本文不存在任何利益冲突。
作者贡献声明:王依泊负责设计论文框架,文献分析,论文撰写;赵昱博负责文献筛选,论文修改;马艳波负责指导写作思路;孙雨晴进行学术内容审核。
-
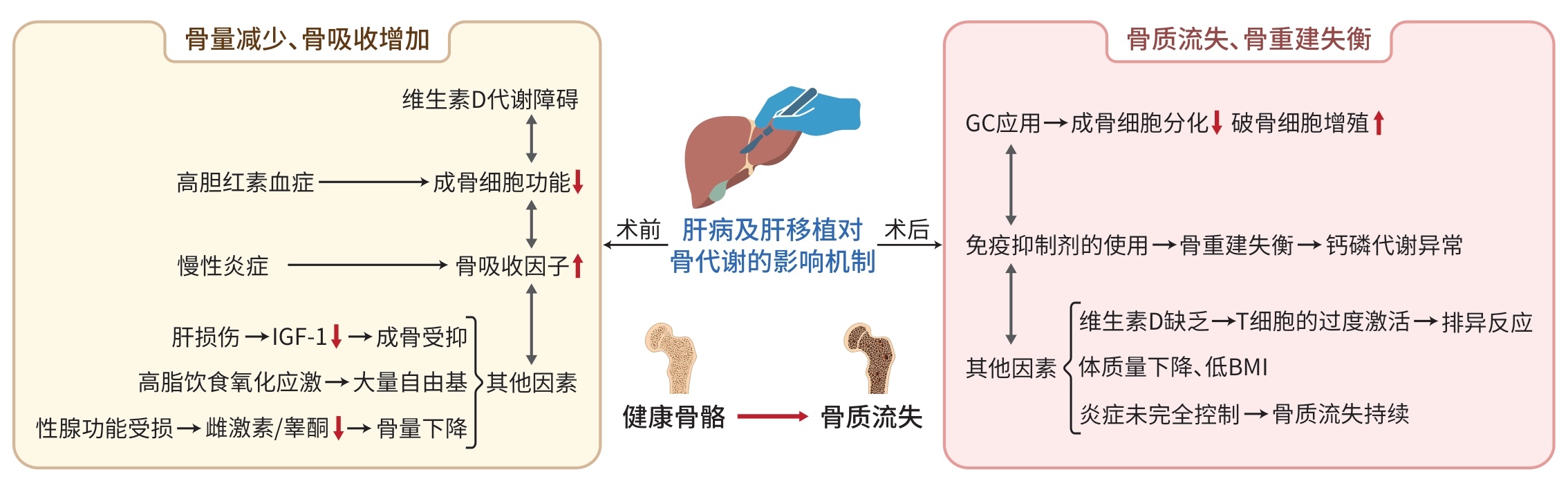
摘要: 肝性骨病是慢性肝病患者常见的并发症,其发生受多种危险因素影响,并已成为影响肝移植术预后的重要因素之一。本文通过分析肝移植围手术期各类因素对骨健康和骨代谢状态的影响,强调在这一时期对患者进行全面骨健康评估和实施必要干预措施的重要性,旨在降低术后并发症的发生风险并改善患者的长期预后。通过深入探讨肝性骨病与肝移植术预后的关系,有助于揭示影响手术效果的关键因素,为术后管理策略的优化提供理论依据。此外,该研究领域的进一步发展将为肝移植患者的治疗提供新思路,有望改善患者的生活质量和长期生存率。Abstract: Hepatic osteodystrophy is a common complication in patients with chronic liver disease and is influenced by various risk factors, and it has become one of the important influencing factors for the prognosis of liver transplantation. By analyzing the influencing factors for bone health and bone metabolism during the perioperative period of liver transplantation, this article emphasizes the importance of a comprehensive assessment of bone health and necessary interventions at this stage, with an aim to reduce the risk of postoperative complications and improve the long-term prognosis of patients. A deeper exploration of the association between hepatic osteodystrophy and the prognosis of liver transplantation can help to reveal the key influencing factors for postoperative outcomes, thus providing a theoretical basis for optimizing postoperative management strategies. Furthermore, advances in this research field will offer new insights into the treatment of patients receiving liver transplantation, and it is expected to further improve quality of life and long-term survival rate.
-
Key words:
- Liver Transplantation /
- Hepatic Osteodystrophy /
- Bone Metabolism /
- Prognosis
-
[1] TSOCHATZIS E, COILLY A, NADALIN S, et al. International liver transplantation consensus statement on end-stage liver disease due to nonalcoholic steatohepatitis and liver transplantation[J]. Transplantation, 2019, 103( 1): 45- 56. DOI: 10.1097/TP.0000000000002433. [2] Chinese Society of Endocrinology, Chinese Medical Association, Chinese Society of Osteoporosis and Bone Mineral Research. Guideline for the diagnosis and management of hypophosphatemic rickets/osteomalacia[J]. Chin J Osteoporos Bone Miner Res, 2022, 15( 2): 107- 125. DOI: 10.3969/j.issn.1674-2591.2022.02.001.中华医学会内分泌学分会, 中华医学会骨质疏松和骨矿盐疾病分会. 中国低血磷性佝偻病/骨软化症诊疗指南[J]. 中华骨质疏松和骨矿盐疾病杂志, 2022, 15( 2): 107- 125. DOI: 10.3969/j.issn.1674-2591.2022.02.001. [3] Chinese Society of Hepatology, Chinese Medical Association. Chinese guidelines on the management of liver cirrhosis[J]. J Clin Hepatol, 2019, 35( 11): 2408- 2425. DOI: 10.3969/j.issn.1001-5256.2019.11.006.中华医学会肝病学分会. 肝硬化诊治指南[J]. 临床肝胆病杂志, 2019, 35( 11): 2408- 2425. DOI: 10.3969/j.issn.1001-5256.2019.11.006. [4] YU TM, LIN CL, CHANG SN, et al. Osteoporosis and fractures after solid organ transplantation: A nationwide population-based cohort study[J]. Mayo Clin Proc, 2014, 89( 7): 888- 895. DOI: 10.1016/j.mayocp.2014.02.017. [5] ANASTASILAKIS AD, TSOURDI E, MAKRAS P, et al. Bone disease following solid organ transplantation: A narrative review and recommendations for management from The European Calcified Tissue Society[J]. Bone, 2019, 127: 401- 418. DOI: 10.1016/j.bone.2019.07.006. [6] QIN RR, QIN JW, LI XF, et al. Influence of immunosuppressive drugs on natural killer cells in therapeutic drug exposure in liver transplantation[J]. Hepatobiliary Surg Nutr, 2023, 12( 6): 835- 853. DOI: 10.21037/hbsn-22-438. [7] GUPTA A, SINHA PK, CHOUDHARY A. Hepatic osteodystrophy after liver transplant: A study on changes in bone mineral density post LT[J]. J Clin Exp Hepatol, 2023, 13: S20- S21. DOI: 10.1016/j.jceh.2023.10.055. [8] ZAVATTA G, VITALE G, MORELLI MC, et al. High bone fracture risk in a large modern cohort of liver transplant recipients[J]. Intern Emerg Med, 2025, 20( 1): 139- 150. DOI: 10.1007/s11739-024-03767-5. [9] PUGLIESE N, ARCARI I, AGHEMO A, et al. Osteosarcopenia in autoimmune cholestatic liver diseases: Causes, management, and challenges[J]. World J Gastroenterol, 2022, 28( 14): 1430- 1443. DOI: 10.3748/wjg.v28.i14.1430. [10] DANFORD CJ, TRIVEDI HD, BONDER A. Bone health in patients with liver diseases[J]. J Clin Densitom, 2020, 23( 2): 212- 222. DOI: 10.1016/j.jocd.2019.01.004. [11] THOMSON M, SCOTT A, TROST S, et al. Low screening rates and high prevalence of osteoporosis in cirrhosis: A real-world retrospective analysis[J]. Aliment Pharmacol Ther, 2024, 59( 4): 535- 546. DOI: 10.1111/apt.17823. [12] LACIN S, YALCIN S, KARAKAS Y, et al. Prognostic significance of serum insulin-like growth factor-1 in hepatocellular cancer patients: A validation study[J]. J Hepatocell Carcinoma, 2020, 7: 143- 153. DOI: 10.2147/JHC.S258930. [13] FU SW. Clinical study of bone metabolic and biochemical indexes and osteoporosis in patients with liver cirrhosis or liver cancer[J]. Chin J Osteoporos, 2013, 19( 11): 1177- 1179. DOI: 10.3969/j.issn.1006-7108.2013.11.015.付士武. 肝硬化、肝癌患者骨代谢生化指标与骨质疏松的临床研究[J]. 中国骨质疏松杂志, 2013, 19( 11): 1177- 1179. DOI: 10.3969/j.issn.1006-7108.2013.11.015. [14] KANG J, GOPAKUMAR H, PULI SR. Prevalence of osteoporosis in cirrhosis: A systematic review and meta-analysis[J]. Cureus, 2023, 15( 1): e33721. DOI: 10.7759/cureus.33721. [15] HANDZLIK-ORLIK G, HOLECKI M, WILCZYŃSKI K, et al. Osteoporosis in liver disease: Pathogenesis and management[J]. Therapeutic Advances Endocrinology, 2016, 7( 3): 128- 135. DOI: 10.1177/204201881-6641351. [16] REINCKE M, SEUFERT J, LAUBNER K, et al. Reduced bone mineral density is associated to post-TIPS survival of female patients with decompensated cirrhosis[J]. Dig Liver Dis, 2024, 56( 10): 1705- 1714. DOI: 10.1016/j.dld.2024.04.009. [17] KOLA S, KOLA I, GJOKA K, et al. Correlation of vitamin D with osteoporosis[J]. Med Clin Res, 2022, 7( 10): 1- 4. DOI: 10.33140/MCR.07.10.01. [18] SUN JY, ZHANG HH, ZHANG Y, et al. Impact of serum calcium levels on total body bone mineral density: A mendelian randomization study in five age strata[J]. Clin Nutr, 2021, 40( 5): 2726- 2733. DOI: 10.1016/j.clnu.2021.03.012. [19] LIU MB, YAO XC, ZHU ZX. Associations between serum calcium, 25(OH)D level and bone mineral density in older adults[J]. J Orthop Surg Res, 2019, 14( 1): 458. DOI: 10.1186/s13018-019-1517-y. [20] CHEN YJ, YU JJ, SHI L, et al. Systemic inflammation markers associated with bone mineral density in perimenopausal and postmenopausal women[J]. J Inflamm Res, 2023, 16: 297- 309. DOI: 10.2147/jir.s385220. [21] SHUKLA V, FATIM J, SIDDIQUI Z, et al. Study of correlation of bone mineral density with severity of liver cirrhosis[J]. J Assoc Physicians Ind, 2023, 71( 6): 30- 32. DOI: 10.5005/japi-11001-0257. [22] RUIZ-GASPÀ S, GUAÑABENS N, JURADO S, et al. Bilirubin and bile acids in osteocytes and bone tissue. Potential role in the cholestatic-induced osteoporosis[J]. Liver Int, 2020, 40( 11): 2767- 2775. DOI: 10.1111/liv.14630. [23] GUAÑABENS N, PARÉS A. Osteoporosis in chronic liver disease[J]. Liver Int, 2018, 38( 5): 776- 785. DOI: 10.1111/liv.13730. [24] HUANG D. Research progress on prevention and treatment of glucocorticoid-induced osteoporosis[J]. Chin J Clin Ration Drug Use, 2020, 13( 11): 180- 181. DOI: 10.15887/j.cnki.13-1389/r.2020.11.109.黄东. 糖皮质激素诱导骨质疏松症防治研究进展[J]. 临床合理用药杂志, 2020, 13( 11): 180- 181. DOI: 10.15887/j.cnki.13-1389/r.2020.11.109. [25] YANG YJ, ZHU Z, WANG DT, et al. Tanshinol alleviates impaired bone formation by inhibiting adipogenesis via KLF15/PPARγ2 signaling in GIO rats[J]. Acta Pharmacol Sin, 2018, 39( 4): 633- 641. DOI: 10.1038/aps.2017.134. [26] YANAGAWA S, TAHARA H, TANAKA Y, et al. Analysis of risk factors affecting incidence of osteoporosis and fragility fractures in liver transplant recipients[J]. Ann Transplant, 2021, 26: 925475. DOI: 10.12659/aot.925475. [27] QU LY, LI JJ. Research progress on the impacts of selective immunosuppressants on bone metabolism[J]. China Med Pharm, 2022, 12( 11): 57- 60. DOI: 10.3969/j.issn.2095-0616.2022.11.015.曲立阳, 李建军. 选择性免疫抑制剂对骨代谢影响的研究进展[J]. 中国医药科学, 2022, 12( 11): 57- 60. DOI: 10.3969/j.issn.2095-0616.2022.11.015. [28] FENG J, MENG ZQ. Insulin growth factor-1 promotes the proliferation and osteogenic differentiation of bone marrow mesenchymal stem cells through the Wnt/β-catenin pathway[J]. Exp Ther Med, 2021, 22( 2): 891. DOI: 10.3892/etm.2021.10323. [29] GARCÍA-ALFARO P, GARCÍA S, RODRIGUEZ I, et al. Association of endogenous hormones and bone mineral density in postmenopausal women[J]. J Midlife Health, 2023, 14( 3): 196- 204. DOI: 10.4103/jmh.jmh_115_23. [30] WANG RC, GAN L, WANG YY, et al. Effect of lyophilized bovine colostrums and compound preparation on prevention and antioxidation of retinoic acid induced osteoporosis in mice[J]. J Anhui Agric Sci, 2021, 49( 10): 157- 160. DOI: 10.3969/j.issn.0517-6611.2021.10.042.王荣昌, 甘露, 王玉莹, 等. 牛初乳冻干粉和复合制剂对维甲酸所致小鼠骨质疏松症的预防和抗氧化作用[J]. 安徽农业科学, 2021, 49( 10): 157- 160. DOI: 10.3969/j.issn.0517-6611.2021.10.042. [31] MAVILIA MG, BHARDWAJ R, WAKEFIELD D, et al. Chronic liver disease patients have worse outcomes and increased postoperative complications after orthopedic fractures[J]. J Clin Gastroenterol, 2019, 53( 9): e371- e375. DOI: 10.1097/mcg.0000000000001166. [32] LIM WH, NG CH, OW ZGW, et al. A systematic review and meta-analysis on the incidence of osteoporosis and fractures after liver transplant[J]. Transpl Int, 2021, 34( 6): 1032- 1043. DOI: 10.1111/tri.13863. [33] HULDÉN E, CASTEDAL M, KARLSSON MK, et al. Osteoporosis in cirrhotics before and after liver transplantation: Relation with malnutrition and inflammatory status[J]. Scand J Gastroenterol, 2020, 55( 3): 354- 361. DOI: 10.1080/00365521.2020.1735507. [34] ZHUO JF, LYU HJ, YI HM, et al. Standard operation procedure of nursing care for enhanced recovery after liver transplantation[J]. Organ Transplant, 2020, 11( 1): 121- 125. DOI: 10.3969/j.issn.1674-7445.2020.01.020.卓金风, 吕海金, 易慧敏, 等. 肝移植术后加速康复护理的标准化操作流程[J]. 器官移植, 2020, 11( 1): 121- 125. DOI: 10.3969/j.issn.1674-7445.2020.01.020. [35] Chinese Society of Osteoporosis and Bone Mineral Research. Guidelines for the diagnosis and treatment of primary osteoporosis(2022)[J]. Chin Gen Pract, 2023, 26( 14): 1671- 1691. DOI: 10.12114/j.issn.1007-9572.2023.0121.中华医学会骨质疏松和骨矿盐疾病分会. 原发性骨质疏松症诊疗指南(2022)[J]. 中国全科医学, 2023, 26( 14): 1671- 1691. DOI: 10.12114/j.issn.1007-9572.2023.0121. [36] CHOUDHARY NS, SARAF N, SAIGAL S, et al. Long-term management of the adult liver transplantation recipients[J]. J Clin Exp Hepatol, 2021, 11( 2): 239- 253. DOI: 10.1016/j.jceh.2020.06.010. [37] KANIS JA, JOHNELL O, ODEN A, et al. FRAX and the assessment of fracture probability in men and women from the UK[J]. Osteoporos Int, 2008, 19( 4): 385- 397. DOI: 10.1007/s00198-007-0543-5. [38] GROVER I, SINGH N, GUNJAN D, et al. Vitamin D status& bone health in patients with liver cirrhosis[J]. Indian J Med Res, 2023, 158( 3): 284- 291. DOI: 10.4103/ijmr.ijmr_1144_20. [39] DÍAZ-TOCADOS JM, RODRÍGUEZ-ORTIZ ME, HERENCIA C, et al. Comparative effects of calcitriol and calcimimetic on bone health in renal insufficiency[J]. FASEB J, 2024, 38( 11): e23726. DOI: 10.1096/fj.202302704R. [40] SANTOS LAA, ROMEIRO FG. Diagnosis and management of cirrhosis-related osteoporosis[J]. Biomed Res Int, 2016, 2016: 1423462. DOI: 10.1155/2016/1423462. [41] WU HJ, XUE Y, ZHANG Y, et al. PTH1-34 promotes osteoblast formation through Beclin1-dependent autophagic activation[J]. J Bone Miner Metab, 2021, 39( 4): 572- 582. DOI: 10.1007/s00774-021-01212-7. [42] YANG Y, DENG YN. Application of immunosuppressants after liver transplantation for hepatocellular carcinoma[J]. J Clin Hepatol, 2021, 37( 2): 263- 266. DOI: 10.3969/j.issn.1001-5256.2021.02.005.杨扬, 邓宜南. 肝细胞癌肝移植术后免疫抑制剂的应用[J]. 临床肝胆病杂志, 2021, 37( 2): 263- 266. DOI: 10.3969/j.issn.1001-5256.2021.02.005. [43] YE ZZ, YI JF, PAN JX. Relationship between exercise and bone strength, body composition, sex hormones in postmenopausal women[J]. Acta Anat Sin, 2021, 52( 3): 473- 478. DOI: 10.16098/j.issn.0529-1356.2021.03.022.叶蓁蓁, 易剑锋, 潘建西. 运动与绝经后女性骨强度、体成分及性激素的关系[J]. 解剖学报, 2021, 52( 3): 473- 478. DOI: 10.16098/j.issn.0529-1356.2021.03.022. [44] XIAO HJ, HAN T. Prevention and treatment of malnutrition, sarcopenia, and osteoporosis in patients with liver cirrhosis[J]. J Clin Hepatol, 2021, 37( 1): 26- 30. DOI: 10.3969/j.issn.1001-5256.2021.01.006.肖慧娟, 韩涛. 肝硬化患者营养不良、肌肉减少症及骨质疏松的防治[J]. 临床肝胆病杂志, 2021, 37( 1): 26- 30. DOI: 10.3969/j.issn.1001-5256.2021.01.006. [45] AKIMOTO S, TAHARA H, KUMAR DL, et al. Predictive factors analysis of osteoporosis and fragility fractures after liver transplantation[J]. Transplantation, 2018, 102( Supplement 7): S80. DOI: 10.1097/01.tp.0000542665.04394.4c. [46] PARVEEN B, PARVEEN A, VOHORA D. Biomarkers of osteoporosis: An update[J]. Endocr Metab Immune Disord Drug Targets, 2019, 19( 7): 895- 912. DOI: 10.2174/1871530319666190204165207. -



 PDF下载 ( 924 KB)
PDF下载 ( 924 KB)

 下载:
下载:


