乳酸化修饰在慢性肝病中的调控作用机制
DOI: 10.12449/JCH251232
利益冲突声明:本文不存在任何利益冲突。
作者贡献声明:容碧晴负责课题设计,资料分析,撰写论文;王佳慧、汪磊、罗淑娟、万宛若、杨仕权参与收集数据,修改论文;郑洋、张荣武、肖华业负责拟定写作思路,指导撰写文章并最后定稿。
-
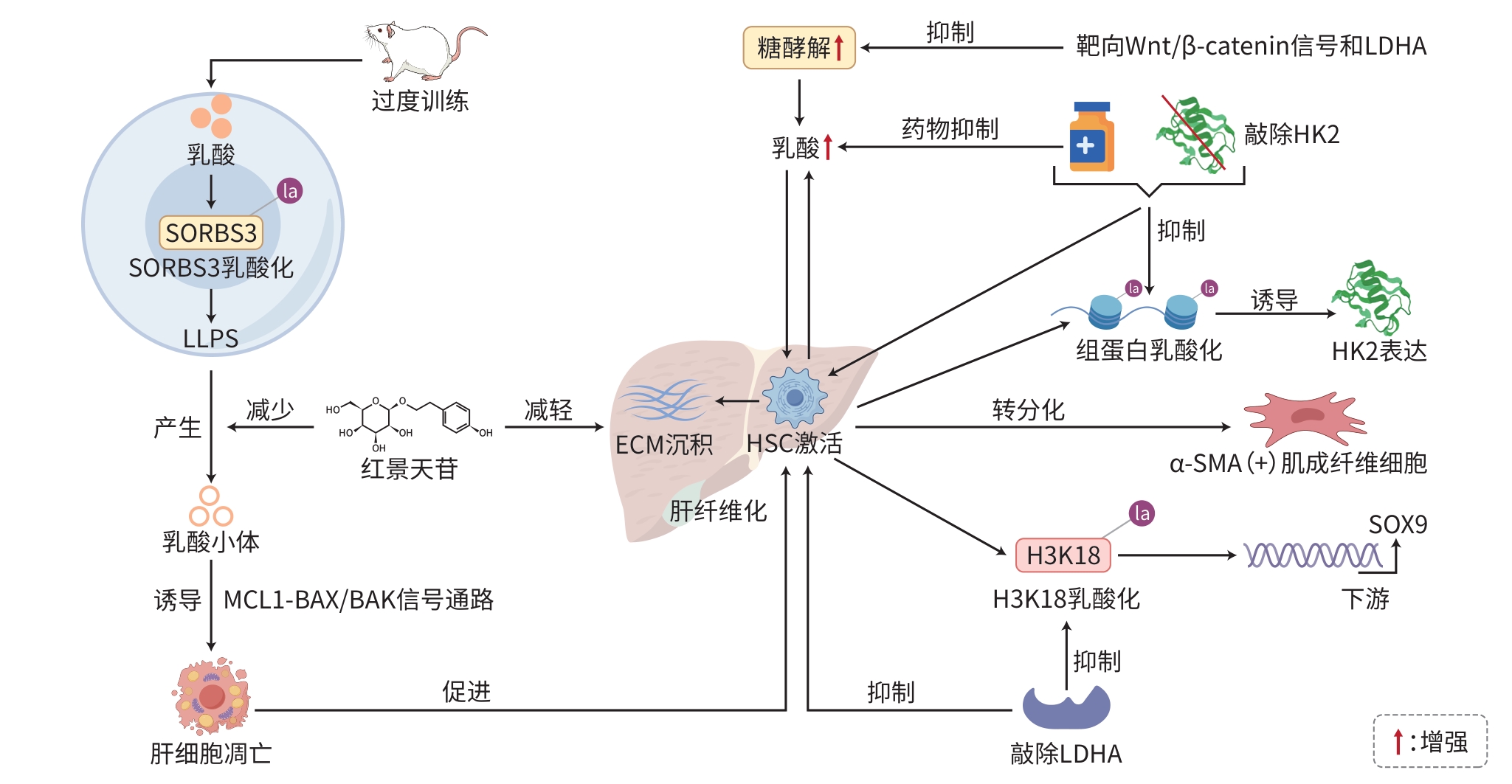
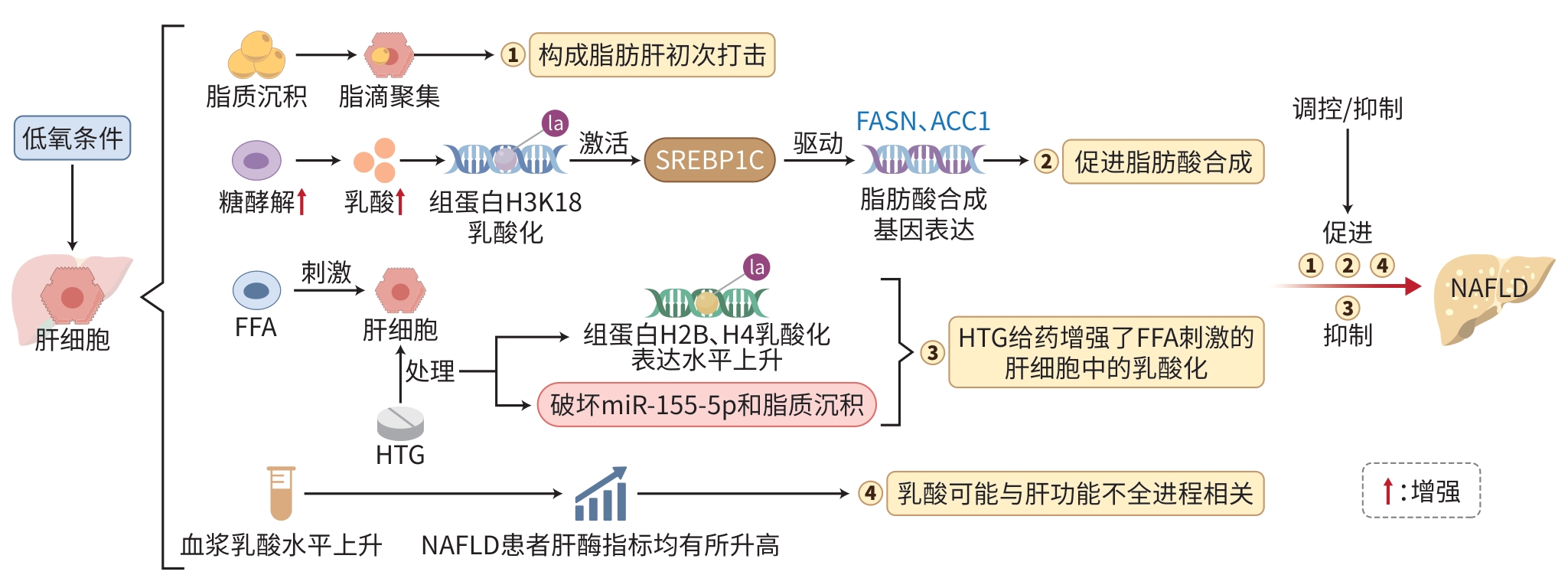
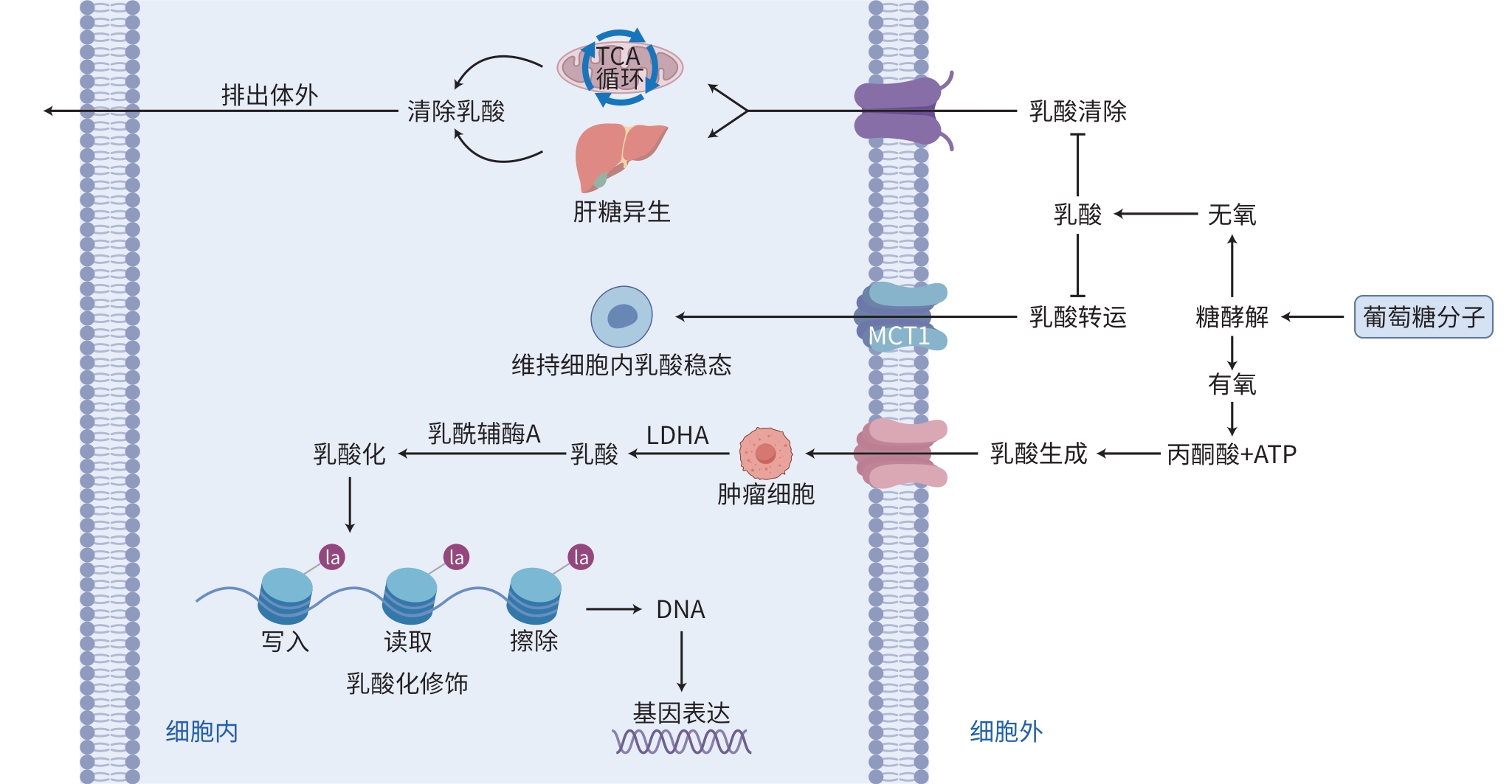
摘要: 慢性肝病是指肝脏长期受各种致病因素的影响,逐渐发展为肝炎、肝纤维化、肝硬化甚至肝癌的病理过程,是一类严重影响肝脏功能的复杂难治性疾病。作为一种新型的蛋白质翻译后修饰,乳酸化修饰通过将乳酸共价连接至靶蛋白的赖氨酸残基,从而动态地调控基因的转录表达与下游细胞功能。近年研究发现,慢性肝病常伴随乳酸代谢异常。乳酸作为肝脏代谢的关键产物,其研究价值日益凸显;而乳酸化修饰则以代谢-表观遗传交互为中介,在肝病的代谢重编程、免疫调控及纤维化进程中发挥着关键作用。本文在概述慢性肝病流行病学的基础上,重点综述了乳酸化修饰的分子机制,其对肝细胞代谢、基因通路及肝星状细胞活化的调控作用,并探讨其作为诊断标志物和治疗靶点的潜力,旨在为揭示乳酸化修饰在慢性肝病的生物化学与分子生物学中的作用机制提供新思路。Abstract: Chronic liver disease refers to the pathological process in which the liver is affected by various pathogenic factors for a long time, gradually leading to hepatitis, hepatic fibrosis, liver cirrhosis, and even hepatocellular carcinoma, and it is a group of complex refractory diseases that severely impairs liver function. As a novel post-translational and epigenetic modification, lactylation modification dynamically regulates gene transcriptional expression and downstream cellular function through the covalent binding of lactate to lysine residues on target proteins. Recent studies have shown that chronic liver disease is often accompanied by abnormal lactate metabolism. As a key metabolic product of the liver, lactate holds a significant research value, and lactylation modification plays a pivotal role in metabolic reprogramming, immune regulation, and fibrogenesis through metabolic-epigenetic interactions. This article introduces the epidemiology of chronic liver disease and reviews the molecular mechanism of lactylation modification and its regulatory effect on hepatocyte metabolism, gene pathways, and hepatic stellate cell activation, as well as its potential as a diagnostic biomarker and a therapeutic target, in order to provide new insights into the biochemical and molecular biological mechanisms of lactylation modification in chronic liver disease.
-
Key words:
- Lactylation Modification /
- Chronic Liver Disease /
- Proteomics
-
-
[1] LI MY, ZHANG W. Research progress of chronic liver disease complicated with depression and anxiety in traditional Chinese and western medicine[J]. Chin J Integr Tradit West Med Liver Dis, 2025, 35( 1): 109- 114. DOI: 10.3969/j.issn.1005-0264.2025.001.026.李梦羽, 张玮. 慢性肝病合并抑郁焦虑的中西医研究进展[J]. 中西医结合肝病杂志, 2025, 35( 1): 109- 114. DOI: 10.3969/j.issn.1005-0264.2025.001.026. [2] YANG ZH, WANG JH, WANG L, et al. Research progress of the regulation of orphan nuclear receptors on chronic liver diseases[J]. Acta Physiol Sin, 2023, 75( 4): 555- 568. DOI: 10.13294/j.aps.2023.0047.杨智荟, 王佳慧, 汪磊, 等. 孤儿受体调控慢性肝病的研究进展[J]. 生理学报, 2023, 75( 4): 555- 568. DOI: 10.13294/j.aps.2023.0047. [3] ZHANG D, TANG ZY, HUANG H, et al. Metabolic regulation of gene expression by histone lactylation[J]. Nature, 2019, 574( 7779): 575- 580. DOI: 10.1038/s41586-019-1678-1. [4] SHI J, LI HJ, ZHAO MY, et al. Progress in the study of anti-hepatic fibrosis of phenylpropanoid constituents of traditional Chinese medicines[J]. Strait Pharm J, 2024, 36( 10): 1- 5. DOI: 10.3969/j.issn.1006-3765.2024.10.001.石杰, 李海军, 赵梅玉, 等. 中药苯丙素类成分抗肝纤维化的研究进展[J]. 海峡药学, 2024, 36( 10): 1- 5. DOI: 10.3969/j.issn.1006-3765.2024.10.001. [5] ZHANG TT, WANG C, SONG AN, et al. Water extract of earthworms mitigates mouse liver fibrosis by potentiating hepatic LKB1/Nrf2 axis to inhibit HSC activation and hepatocyte death[J]. J Ethnopharmacol, 2024, 321: 117495. DOI: 10.1016/j.jep.2023.117495. [6] WANG FX, CHEN L, KONG DS, et al. Canonical Wnt signaling promotes HSC glycolysis and liver fibrosis through an LDH-A/HIF-1α transcriptional complex[J]. Hepatology, 2024, 79( 3): 606- 623. DOI: 10.1097/HEP.0000000000000569. [7] MA YJ, YU HF. The roles of protein lactylation in liver diseases[J]. Chem Life, 2024, 44( 12): 2334- 2341. DOI: 10.13488/j.smhx.20240457.马一捷, 余和芬. 蛋白质乳酸化修饰在肝脏疾病中的作用[J]. 生命的化学, 2024, 44( 12): 2334- 2341. DOI: 10.13488/j.smhx.20240457. [8] RHO H, TERRY AR, CHRONIS C, et al. Hexokinase 2-mediated gene expression via histone lactylation is required for hepatic stellate cell activation and liver fibrosis[J]. Cell Metab, 2023, 35( 8): 1406- 1423. e 8. DOI: 10.1016/j.cmet.2023.06.013. [9] WU SJ, LI JH, ZHAN YF. H3K18 lactylation accelerates liver fibrosis progression through facilitating SOX9 transcription[J]. Exp Cell Res, 2024, 440( 2): 114135. DOI: 10.1016/j.yexcr.2024.114135. [10] LIU Y, ZHOU R, GUO YF, et al. Muscle-derived small extracellular vesicles induce liver fibrosis during overtraining[J]. Cell Metab, 2025, 37( 4): 824- 841. e 8. DOI: 10.1016/j.cmet.2024.12.005. [11] HUANG WQ, WEN HY, LI JX, et al. Viral hepatitis: A review of global prevalence and research progress toward elimination[J]. Chin J Public Health, 2024, 40( 11): 1413- 1416. DOI: 10.11847/zgggws11-44938.黄文琪, 温卉妍, 李佳昕, 等. 全球病毒性肝炎现状及消除进展[J]. 中国公共卫生, 2024, 40( 11): 1413- 1416. DOI: 10.11847/zgggws1144938. [12] WANG Y. Public health management strategies: A pathway to eliminating viral hepatitis threats[J]. J Clin Hepatol, 2025, 41( 2): 201- 204. DOI: 10.12449/JCH250201.王宇. 建立公共卫生管理模式, 促进消除病毒性肝炎危害[J]. 临床肝胆病杂志, 2025, 41( 2): 201- 204. DOI: 10.12449/JCH250201. [13] YANG ZJ, YAN C, MA JQ, et al. Lactylome analysis suggests lactylation-dependent mechanisms of metabolic adaptation in hepatocellular carcinoma[J]. Nat Metab, 2023, 5( 1): 61- 79. DOI: 10.1038/s42255-022-00710-w. [14] HENRY L, PAIK J, YOUNOSSI ZM. Review article: The epidemiologic burden of non-alcoholic fatty liver disease across the world[J]. Aliment Pharmacol Ther, 2022, 56( 6): 942- 956. DOI: 10.1111/apt.17158. [15] CHENG WH. Effect of hypoxia on lipid metabolism of L02 cells and its possible mechanism[D]. Chongqing: Chongqing Medical University, 2012.程文会. 低氧对L02细胞脂肪代谢的影响及其可能机制[D]. 重庆: 重庆医科大学, 2012. [16] GAO RX, LI Y, XU ZM, et al. Mitochondrial pyruvate carrier 1 regulates fatty acid synthase lactylation and mediates treatment of nonalcoholic fatty liver disease[J]. Hepatology, 2023, 78( 6): 1800- 1815. DOI: 10.1097/HEP.0000000000000279. [17] YIN XJ, LI M, WANG YZ, et al. Herbal medicine formula Huazhuo Tiaozhi granule ameliorates dyslipidaemia via regulating histone lactylation and miR-155-5p biogenesis[J]. Clin Epigenetics, 2023, 15( 1): 175. DOI: 10.1186/s13148-023-01573-y. [18] ZHANG SY. Correlation study on the relationship between plasma lactate levels and the severity of fatty liver and related clinical indicators in NAFLD patients[D]. Hangzhou: Hangzhou Normal University, 2023.章思懿. NAFLD患者血浆乳酸水平与脂肪肝严重程度及相关临床指标的相关性研究[D]. 杭州: 杭州师范大学, 2023. [19] SHENG XD. Study on the mechanism of action of tea water extract in treating alcohol-related liver injury[D]. Hefei: Anhui Medical University, 2024.盛啸东. 茶叶水提取物治疗酒精性相关性肝损伤的作用机制研究[D]. 合肥: 安徽医科大学, 2024. [20] JIANG QL. Shanghai Institute of Nutrition and Health, CAS, Elucidates Mechanism of Ethyl Lactate in Ameliorating Liver Injury and Alcohol-Associated Liver Disease[N]. Science Times, 2024-12-16(3). DOI: 10.28514/n.cnki.nkxsb.2024.002987.江庆龄. 中国科学院上海营养与健康研究所等揭示乳酸乙酯改善肝损伤与酒精相关性肝病机制[N]. 中国科学报, 2024-12-16(3). DOI: 10.28514/n.cnki.nkxsb.2024.002987. [21] JIANG Y, WEI S, SHEN SM, et al. Ethyl lactate ameliorates hepatic steatosis and acute-on-chronic liver injury in alcohol-associated liver disease by inducing fibroblast growth factor 21[J]. Adv Sci(Weinh), 2025, 12( 5): e2409516. DOI: 10.1002/advs.202409516. [22] JIANG YC, ZHANG T, KUSUMANCHI P, et al. Alcohol metabolizing enzymes, microsomal ethanol oxidizing system, cytochrome P450 2E1, catalase, and aldehyde dehydrogenase in alcohol-associated liver disease[J]. Biomedicines, 2020, 8( 3): 50. DOI: 10.3390/biomedicines8030050. [23] LLOVET JM, KELLEY RK, VILLANUEVA A, et al. Hepatocellular carcinoma[J]. Nat Rev Dis Primers, 2021, 7( 1): 6. DOI: 10.1038/s41572-020-00240-3. [24] ZHU CF, WANG XD. Value of local treatment combined with systemic therapy in conversion therapy for hepatocellular carcinoma[J]. J Clin Hepatol, 2024, 40( 9): 1732- 1737. DOI: 10.12449/JCH240903.朱超凡, 王晓东. 局部治疗联合系统治疗在肝细胞癌转化治疗中的价值[J]. 临床肝胆病杂志, 2024, 40( 9): 1732- 1737. DOI: 10.12449/JCH24-0903. [25] YE ZJ. The impact of LSD1 lactic acid modification on the development of liver cancer and the mechanism of TIGD1 on liver cancer growth[D]. Guangzhou: South China University of Technology, 2023.叶子坚. LSD1乳酸化修饰对肝癌发生发展的影响和TIGD1对肝癌生长的机制研究[D]. 广州: 华南理工大学, 2023. [26] JIN J, BAI L, WANG DY, et al. SIRT3-dependent delactylation of cyclin E2 prevents hepatocellular carcinoma growth[J]. EMBO Rep, 2023, 24( 5): e56052. DOI: 10.15252/embr.202256052. [27] HONG H, HAN HX, WANG L, et al. ABCF1-K430-Lactylation promotes HCC malignant progression via transcriptional activation of HIF1 signaling pathway[J]. Cell Death Differ, 2025, 32( 4): 613- 631. DOI: 10.1038/s41418-024-01436-w. [28] PAN LH, FENG F, WU JQ, et al. Demethylzeylasteral targets lactate by inhibiting histone lactylation to suppress the tumorigenicity of liver cancer stem cells[J]. Pharmacol Res, 2022, 181: 106270. DOI: 10.1016/j.phrs.2022.106270. [29] XU HY, LI LQ, WANG SS, et al. Royal jelly acid suppresses hepatocellular carcinoma tumorigenicity by inhibiting H3 histone lactylation at H3K9la and H3K14la sites[J]. Phytomedicine, 2023, 118: 154940. DOI: 10.1016/j.phymed.2023.154940. [30] PERALTA RM, XIE BX, LONTOS K, et al. Dysfunction of exhausted T cells is enforced by MCT11-mediated lactate metabolism[J]. Nat Immunol, 2024, 25( 12): 2297- 2307. DOI: 10.1038/s41590-024-01999-3. [31] HAN SL, BAO XY, ZOU YF, et al. D-lactate modulates M2 tumor-associated macrophages and remodels immunosuppressive tumor microenvironment for hepatocellular carcinoma[J]. Sci Adv, 2023, 9( 29): eadg2697. DOI: 10.1126/sciadv.adg2697. [32] FENG F, WU JQ, CHI QJ, et al. Lactylome analysis unveils lactylation-dependent mechanisms of stemness remodeling in the liver cancer stem cells[J]. Adv Sci, 2024, 11( 38): 2405975. DOI: 10.1002/advs.202405975. [33] WANG HY, XU M, ZHANG T, et al. PYCR1 promotes liver cancer cell growth and metastasis by regulating IRS1 expression through lactylation modification[J]. Clin Transl Med, 2024, 14( 10): e70045. DOI: 10.1002/ctm2.70045. [34] DONG RY, FEI Y, HE YR, et al. Lactylation-driven HECTD2 limits the response of hepatocellular carcinoma to lenvatinib[J]. Adv Sci(Weinh), 2025, 12( 15): e2412559. DOI: 10.1002/advs.202412559. [35] CHEN J, HUANG ZY, CHEN Y, et al. Lactate and lactylation in cancer[J]. Sig Transduct Target Ther, 2025, 10( 1): 38. DOI: 10.1038/s41392-024-02082-x. [36] HALFORD S, VEAL GJ, WEDGE SR, et al. A phase I dose-escalation study of AZD3965, an oral monocarboxylate transporter 1 inhibitor, in patients with advanced cancer[J]. Clin Cancer Res, 2023, 29( 8): 1429- 1439. DOI: 10.1158/1078-0432.CCR-22-2263. [37] JIANG PR, NING WS, SHI YS, et al. FSL-Kla: A few-shot learning-based multi-feature hybrid system for lactylation site prediction[J]. Comput Struct Biotechnol J, 2021, 19: 4497- 4509. DOI: 10.1016/j.csbj.2021.08.013. -



 PDF下载 ( 2063 KB)
PDF下载 ( 2063 KB)

 下载:
下载: