Expert consensus on clinical practice for the diagnosis and treatment of hepatic vascular diseases (2026 edition)
-
摘要: 肝脏血管性疾病(如门静脉血栓、门静脉肝窦血管病、遗传性出血性毛细血管扩张症、动脉门静脉瘘、肝窦阻塞综合征、布-加综合征等)临床表现多样、诊断困难、治疗方案多样,给临床诊疗带来巨大挑战,目前国内尚无肝脏血管性疾病诊治指南或共识。为规范并提高我国肝脏血管性疾病的诊疗水平,中国研究型医院学会肝病(中西医结合)专业委员会、中国研究型医院学会介入医学专业委员会、北京医师协会门静脉高压症多学科诊治医师分会组织相关领域专家,基于最新循证医学证据,结合我国临床实践,围绕肝脏血管性疾病的临床诊断与治疗,制定本共识。Abstract: Hepatic vascular diseases (such as portal vein thrombosis, porto-sinusoidal vascular disease, hereditary hemorrhagic telangiectasia, arterioportal fistula, and sinusoidal obstruction syndrome, Budd-Chiari syndrome) are characterized by diverse clinical manifestations, difficulties in diagnosis, and various treatment regimens, which brings huge challenges to clinical diagnosis and treatment, and at present, there are still no guidelines or consensus statements on the diagnosis and treatment of hepatic vascular diseases in China. To standardize and improve the diagnosis and treatment of hepatic vascular diseases in China, Committee on Liver Diseases (Integrated Traditional Chinese and Western Medicine) of China Research Hospital Association, Committee on Interventional Medicine of China Research Hospital Association, and Branch for Multidisciplinary Diagnosis and Treatment of Portal Hypertension of Beijing Medical Doctor Association organized the experts in related fields to develop expert consensus on clinical practice for the diagnosis and treatment of hepatic vascular diseases (2025 edition) based on the latest evidence-based medical research and the clinical practice in China, with a focus on the diagnosis and treatment of hepatic vascular diseases.
-
Key words:
- Hepatic Vascular Diseases /
- Diagnosis /
- Therapeutics /
- Hypertension, Portal /
- Practice Guideline
-
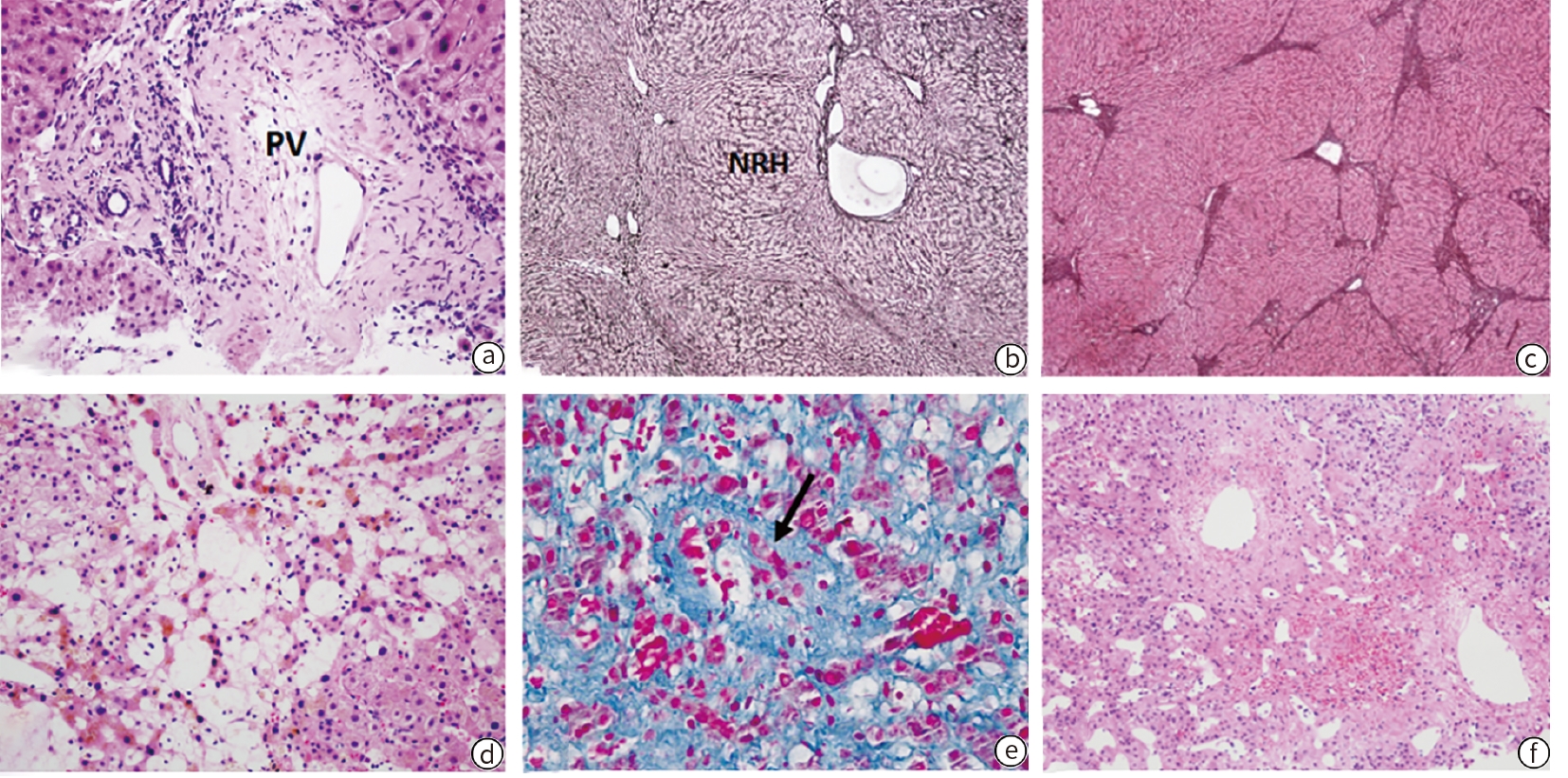
注: PSVD(a~c):门静脉管壁增厚,管腔狭小(a,苏木精-伊红染色,×200);结节性再生性增生,萎缩的肝板围绕增生的肝板形成结节状(b,网织染色,×100);不全间隔肝纤维化/肝硬化,纤细的不完全的纤维隔不规则分隔肝实质(c,网织染色,×100)。HSOS(d、e):中央区肝窦扩张、肝板萎缩、肝细胞坏死消失(d,苏木精-伊红染色,×200);中央静脉内膜增生、管腔闭塞(e,箭头,Masson 三色染色,×400)。BCS(f):中央静脉伸出纤维化带分隔肝实质,周围肝实质内肝窦扩张淤血(f,苏木精-伊红染色,×100)。PSVD,门脉肝窦血管病;PV,门静脉;HE,苏木精-伊红;NRH,结节性再生性增生;HSOS,肝窦阻塞综合征;BCS,布加综合征。
图 4 PSVD、HSOS及BCS病理图
Figure 4. Pathological diagram of PSVD, HSOS and BCS
表 1 牛津大学循证医学中心证据分级(2011版)
Table 1. Oxford Centre for Evidence-based Medicine - levels of evidence (2011 edition)
证据级别 描述 1 基于RCT的系统评价,全或无研究(即干预前所
有患者结局一致,干预后几乎全部转变)、效应量
大的观察性研究2 单个RCT研究、效应量大的观察性研究 3 非RCT 研究,随访研究 4 病例系列,病例对照研究、回顾性对照研究 5 专家意见(基于机制推理) 注:RCT,随机对照试验。
表 2 GRADE推荐标准
Table 2. GRADE recommendation system
推荐强度 描述 A 强烈推荐:明确显示干预措施利大于弊或
弊大于利B 较弱推荐:利弊不明确或无论证据质量高
低均显示利弊相当注:GRADE,推荐分级的评估、制定与评价。
表 3 肝脏血管性疾病分类及其致病因素
Table 3. Classification and etiology of hepatic vascular diseases
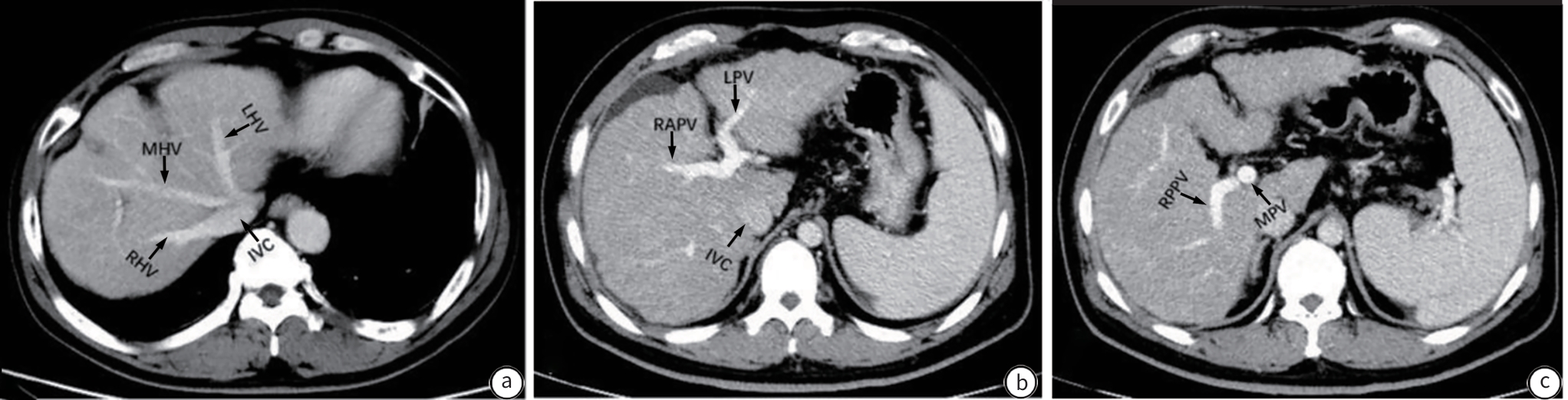
疾病分类 相关疾病 主要致病因素 肝动脉系统及其延伸 肝动脉狭窄(血栓或外科手术后)
动脉瘤
缺血性胆管病
动脉门静脉瘘
遗传性出血性毛细血管扩张症
脾动脉盗血综合征后天性因素(包括机械性损伤、医源性损伤
等)、先天发育异常、遗传因素、感染等门静脉系统及其延伸 门静脉阻塞性疾病(包括PVT)
脾静脉阻塞性疾病(包括脾静脉血栓)
肠系膜静脉阻塞性疾病(包括肠系膜上静脉血栓、
肠系膜下静脉血栓)
门静脉肝窦血管病
先天性门体分流(包括Abernethy综合征等)
门静脉瘤血栓形成、门静脉纤维化、机械性及药物性肝损
伤、先天发育异常、遗传因素、肿瘤、胰腺疾病、
感染等肝窦系统 肝窦阻塞综合征
肝窦阻塞相关性疾病(肝淀粉样变、镰状细胞病、
骨髓纤维化、戈谢病、恶性肿瘤等引起肝窦阻塞)
肝紫斑病遗传因素、细胞浸润或物质沉积性疾病、血液
系统疾病、药源性损伤等肝静脉系统及其延伸 布-加综合征
肉芽肿性静脉炎
淤血性肝病
肝静脉瘤发育异常、血栓性疾病、机械性及药物性肝损
伤、心源性疾病、感染等表 4 不同类型PH血管压力特征
Table 4. Features of vascular pressure in different types of PH
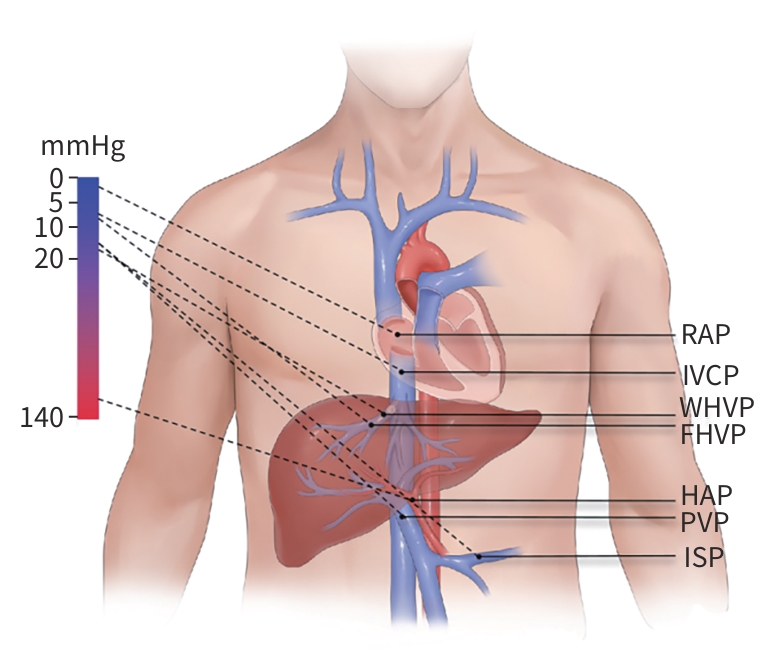
类型 FHVP WHVP HVPG RAP IVCP PVP ISP PPG 肝前性 → → → → → ↑ ↑ ↑ 窦前性 → ↑ →↑ → → ↑ ↑ ↑ 窦性 → ↑ →↑ → → ↑ ↑ ↑ 窦后性 → ↑ →↑ → →↑ ↑ ↑ →↑ 肝后性 ↑ ↑ →↑ →↑ ↑ ↑ ↑ →↑ 注:↑表示压力升高,→表示压力正常,→↑表示压力正常或升高。FHVP,肝静脉游离压力;WHVP,肝静脉楔压;HVPG,肝静脉压力梯度;RAP,右心房压力;IVCP,下腔静脉压;PVP,门静脉压力;ISP,脾内压力;PPG,门静脉压力梯度。
表 5 HSCT-HSOS与PA-HSOS的诊断标准
Table 5. Diagnostic criteria for HSCT-HSOS and PA-HSOS
诊断 EBMT-HSCT-HSOS精细分类(成人) PA-HSOS 疑似 HSCT后(经典型21天内,迟发型21天后)出现以下其中两项:
胆红素≥34.2 μmol/L、体重增加5%、腹水、肝区胀痛肝肿大、超
声和/或弹性成像提示HSOS腹胀和/或肝区疼痛、肝大和腹水;血清总胆红素升高或
其他肝功能异常;典型的增强CT或MRI表现临床 HSCT后出现总胆红素≥34.2 μmol/L且包括以下其中两项:体重
增加5%、腹水、肝区胀痛肝肿大上述症状加上有明确服用含PA植物史或者血清吡咯蛋
白加合物阳性,同时排除其他已知病因所致肝损伤确诊 组织学证据 组织学证据 注:HSCT,造血干细胞移植;HSOS,肝窦阻塞综合征;PA,吡咯生物碱;EBMT, 欧洲血液与骨髓移植学会;CT,计算机体层成像;MRI,磁共振成像。
-
[1] NORTHUP PG, GARCIA-PAGAN JC, GARCIA-TSAO G, et al. Vascular liver disorders, portal vein thrombosis, and procedural bleeding in patients with liver disease: 2020 practice guidance by the American association for the study of liver diseases[J]. Hepatology, 2021, 73( 1): 366- 413. DOI: 10.1002/hep.31646. [2] TYRASKIS A, DURKIN N, DAVENPORT M. Congenital vascular anomalies of the liver[J]. S Afr Med J, 2017, 107( 10): 12130. [3] GUYATT G, OXMAN AD, AKL EA, et al. GRADE guidelines: 1. Introduction: GRADE evidence profiles and summary of findings tables[J]. J Clin Epidemiol, 2011, 64( 4): 383- 394. DOI: 10.1016/j.jclinepi.2010.04.026. [4] KHANNA R, SARIN SK. Non-cirrhotic portal hypertension-diagnosis and management[J]. J Hepatol, 2014, 60( 2): 421- 441. DOI: 10.1016/j.jhep.2013.08.013. [5] KHANNA R, SARIN SK. Idiopathic portal hypertension and extrahepatic portal venous obstruction[J]. Hepatol Int, 2018, 12( Suppl 1): 148- 167. DOI: 10.1007/s12072-018-9844-3. [6] CRAWFORD JM. Vascular disorders of the liver[J]. Clin Liver Dis, 2010, 14( 4): 635- 650. DOI: 10.1016/j.cld.2010.08.002. [7] BOOZARI B, BAHR MJ, KUBICKA S, et al. Ultrasonography in patients with Budd-Chiari syndrome: Diagnostic signs and prognostic implications[J]. J Hepatol, 2008, 49( 4): 572- 580. DOI: 10.1016/j.jhep.2008.04.025. [8] ZHANG LM, ZHANG GY, LIU YL, et al. Ultrasonography and computed tomography diagnostic evaluation of Budd-Chiari syndrome based on radical resection exploration results[J]. Ultrasound Q, 2015, 31( 2): 124- 129. DOI: 10.1097/RUQ.0000000000000122. [9] MOHAMED AFIF A, ANTHONY APM, JAMARUDDIN S, et al. Diagnostic accuracy of Doppler ultrasound for detecting hepatic artery stenosis after liver transplantation[J]. Clin Radiol, 2021, 76( 9): 708.e19- 708.e25. DOI: 10.1016/j.crad.2021.02.032. [10] FRONGILLO F, LIROSI MC, NURE E, et al. Diagnosis and management of hepatic artery complications after liver transplantation[J]. Transplant Proc, 2015, 47( 7): 2150- 2155. DOI: 10.1016/j.transproceed.2014.11.068. [11] BUSCARINI E, BUSCARINI L, DANESINO C, et al. Hepatic vascular malformations in hereditary hemorrhagic telangiectasia: Doppler sonographic screening in a large family[J]. J Hepatol, 1997, 26( 1): 111- 118. DOI: 10.1016/s0168-8278(97)80017-7. [12] BUSCARINI E, DANESINO C, OLIVIERI C, et al. Doppler ultrasonographic grading of hepatic vascular malformations in hereditary hemorrhagic telangiectasia: Results of extensive screening[J]. Ultraschall Med, 2004, 25( 5): 348- 355. DOI: 10.1055/s-2004-813549. [13] CASELITZ M, BAHR MJ, BLECK JS, et al. Sonographic criteria for the diagnosis of hepatic involvement in hereditary hemorrhagic telangiectasia(HHT)[J]. Hepatology, 2003, 37( 5): 1139- 1146. DOI: 10.1053/jhep.2003.50197. [14] LI ZY, LI X. Clinical value of color Doppler ultrasound in hepatic vascular diseases[J]. J Pract Med Imag, 2021, 22( 1): 29- 31. DOI: 10.16106/j.cnki.cn14-1281/r.2021.01.009.李志勇, 李星. 彩色多普勒超声对肝脏血管性疾病的临床价值[J]. 实用医学影像杂志, 2021, 22( 1): 29- 31. DOI: 10.16106/j.cnki.cn14-1281/r.2021.01.009. [15] DENG LL, ZHANG Y, YANG XS, et al. Liver hemodynamic changes in patients with portal hypertension after splenectomy plus cardia peripheral vascular amputation by ultrasound[J]. J Clin Ultrasound Med, 2016, 18( 5): 304- 307. DOI: 10.16245/j.cnki.issn1008-6978.2016.05.006.邓岚岚, 张嫄, 杨雪松, 等. 门静脉高压症患者行脾切除及贲门周围血管离断术后肝脏血流动力学变化的超声观测[J]. 临床超声医学杂志, 2016, 18( 5): 304- 307. DOI: 10.16245/j.cnki.issn1008-6978.2016.05.006. [16] WALSER EM, DELA PENA R, VILLANUEVA-MEYER J, et al. Hepatic perfusion before and after the transjugular intrahepatic portosystemic shunt procedure: Impact on survival[J]. J Vasc Interv Radiol, 2000, 11( 7): 913- 918. DOI: 10.1016/s1051-0443(07)61811-9. [17] GÜLBERG V, HAAG K, RÖSSLE M, et al. Hepatic arterial buffer response in patients with advanced cirrhosis[J]. Hepatology, 2002, 35( 3): 630- 634. DOI: 10.1053/jhep.2002.31722. [18] ENGSTROM BI, HORVATH JJ, SUHOCKI PV, et al. Covered transjugular intrahepatic portosystemic shunts: Accuracy of ultrasound in detecting shunt malfunction[J]. AJR Am J Roentgenol, 2013, 200( 4): 904- 908. DOI: 10.2214/AJR.12.8761. [19] FANG L, HUANG BJ, DING H, et al. Contrast-enhanced ultrasound(CEUS) for the diagnosis of hypoechoic hepatic hemangioma in clinical practice[J]. Clin Hemorheol Microcirc, 2019, 72( 4): 395- 405. DOI: 10.3233/CH-190558. [20] PISCAGLIA F, GIANSTEFANI A, RAVAIOLI M, et al. Criteria for diagnosing benign portal vein thrombosis in the assessment of patients with cirrhosis and hepatocellular carcinoma for liver transplantation[J]. Liver Transpl, 2010, 16( 5): 658- 667. DOI: 10.1002/lt.22044. [21] CHEN ZH, CHEN FH, JI JS, et al. Diagnostic value of contrast-enhanced ultrasound for secondary arterio-portal fistula after radiofrequency ablation on hepatocellular carcinoma[J]. J Med Imag, 2019, 29( 2): 252- 256.陈志辉, 陈方红, 纪建松, 等. 超声造影对肝癌射频消融后继发性肝动脉-门静脉瘘的诊断价值[J]. 医学影像学杂志, 2019, 29( 2): 252- 256. [22] SIDHU PS, ELLIS SM, KARANI JB, et al. Hepatic artery stenosis following liver transplantation: Significance of the tardus Parvus waveform and the role of microbubble contrast media in the detection of a focal stenosis[J]. Clin Radiol, 2002, 57( 9): 789- 799. [23] ZHENG RQ, MAO R, REN J, et al. Contrast-enhanced ultrasound for the evaluation of hepatic artery stenosis after liver transplantation: Potential role in changing the clinical algorithm[J]. Liver Transpl, 2010, 16( 6): 729- 735. DOI: 10.1002/lt.22054. [24] GAO X, WANG HH, ZHANG YZ, et al. Contrast-enhanced ultrasound at high mechanical index: A new method for transjugular intrahepatic portosystemic shunt follow-up[J]. Clin Radiol, 2020, 75( 4): 302- 307. DOI: 10.1016/j.crad.2019.10.011. [25] Chinese Society of Imaging Technology Chinese Medical Association. Expert consensus on multi-slice spiral CT examination for acute stroke[J]. Chin J Radiol, 2020, 54( 9): 839- 845. DOI: 10.3760/cma.j.cn112149-20191226-01008.中华医学会影像技术分会. 急性脑卒中多层螺旋CT检查技术专家共识[J]. 中华放射学杂志, 2020, 54( 9): 839- 845. DOI: 10.3760/cma.j.cn112149-20191226-01008. [26] ZHANG YQ, ZHU JY, LYU HJ, et al. Role of CT angiography in preoperative evaluation of donor hepatic veins before right lobe living donor liver transplantation[J/CD]. Chin J Hepatic Surg, 2017, 6( 6): 489- 493. DOI: 10.3877/cma.j.issn.2095-3232.2017.06.016.张亚琴, 朱俊颖, 吕海金, 等. CT血管造影在肝右叶活体肝移植术前供者肝静脉评估中价值[J/CD]. 中华肝脏外科手术学电子杂志, 2017, 6( 6): 489- 493. DOI: 10.3877/cma.j.issn.2095-3232.2017.06.016. [27] DI MARTINO M, ROSSI M, MENNINI G, et al. Imaging follow-up after liver transplantation[J]. Br J Radiol, 2016, 89( 1064): 20151025. DOI: 10.1259/bjr.20151025. [28] XU HT, DAI Y, LIU XH, et al. Using liver acceleration volume acquisition enhanced MRI to study the different collateral pathways in patients with various types of Budd-Chiari syndrome[J]. Chin J Hepatobiliary Surg, 2016, 22( 8): 526- 529. DOI: 10.3760/cma.j.issn.1007-8118.2016.08.007.徐慧婷, 代岳, 刘小华, 等. 利用磁共振肝脏加速容积采集技术研究布加综合征患者不同侧支循环类型与分型[J]. 中华肝胆外科杂志, 2016, 22( 8): 526- 529. DOI: 10.3760/cma.j.issn.1007-8118.2016.08.007. [29] LI JY, FU Q, LIU XM, et al. Feasibility study of 3D high-resolution compressed sensing contrast-enhanced whole-body MRA imaging technology[J]. Chin J Magn Reson Imag, 2024, 15( 11): 123- 129. DOI: 10.12015/issn.1674-8034.2024.11.019.李景阳, 富青, 刘小明, 等. 三维高分辨压缩感知对比增强全身MRA技术的可行性研究[J]. 磁共振成像, 2024, 15( 11): 123- 129. DOI: 10.12015/issn.1674-8034.2024.11.019. [30] Imaging Technology Branch of Chinese Medical Association, Radiology Branch of Chinese Medical Association. Expert consensus on MRI technology[J]. Chin J Radiol, 2016, 50( 10): 724- 739. DOI: 10.3760/cma.j.issn.1005-1201.2016.10.002.中华医学会影像技术分会, 中华医学会放射学分会. MRI检查技术专家共识[J]. 中华放射学杂志, 2016, 50( 10): 724- 739. DOI: 10.3760/cma.j.issn.1005-1201.2016.10.002. [31] LAMBERT MA, WEIR-MCCALL JR, SALSANO M, et al. Prevalence and distribution of atherosclerosis in a low- to intermediate-risk population: Assessment with whole-body MR angiography[J]. Radiology, 2018, 287( 3): 795- 804. DOI: 10.1148/radiol.2018171609. [32] RIEDEL C, LENZ A, FISCHER L, et al. Abdominal applications of 4D flow MRI[J]. Rofo, 2021, 193( 4): 388- 398. DOI: 10.1055/a-1271-7405. [33] BRUNSING RL, BROWN D, ALMAHOUD H, et al. Quantification of the hemodynamic changes of cirrhosis with free-breathing self-navigated MRI[J]. J Magn Reson Imag, 2021, 53( 5): 1410- 1421. DOI: 10.1002/jmri.27488. [34] HIGAKI A, KANKI A, YAMAMOTO A, et al. Liver cirrhosis: Relationship between fibrosis-associated hepatic morphological changes and portal hemodynamics using four-dimensional flow magnetic resonance imaging[J]. Jpn J Radiol, 2023, 41( 6): 625- 636. DOI: 10.1007/s11604-023-01388-0. [35] ROLDÁN-ALZATE A, FRYDRYCHOWICZ A, SAID A, et al. Impaired regulation of portal venous flow in response to a meal challenge as quantified by 4D flow MRI[J]. J Magn Reson Imag, 2015, 42( 4): 1009- 1017. DOI: 10.1002/jmri.24886. [36] STANKOVIC Z, CSATARI Z, DEIBERT P, et al. Normal and altered three-dimensional portal venous hemodynamics in patients with liver cirrhosis[J]. Radiology, 2012, 262( 3): 862- 873. DOI: 10.1148/radiol.11110127. [37] National Health Commission of the People's Republic of China. Standard for diagnosis and treatment of primary liver cancer(2024 edition)[J]. J Clin Hepatol, 2024, 40( 5): 893- 918. DOI: 10.12449/JCH240508.中华人民共和国国家卫生健康委员会. 原发性肝癌诊疗指南(2024年版)[J]. 临床肝胆病杂志, 2024, 40( 5): 893- 918. DOI: 10.12449/JCH240508. [38] LI B, WANG HG, GAO LM, et al. Expert consensus on operating specifications of abdominal interventional imaging technicians[J]. J Clin Radiol, 2024, 43( 11): 1842- 1848. DOI: 10.13437/j.cnki.jcr.2024.11.017.李博, 王红光, 高丽敏, 等. 腹部介入影像技师操作规范专家共识[J]. 临床放射学杂志, 2024, 43( 11): 1842- 1848. DOI: 10.13437/j.cnki.jcr.2024.11.017. [39] Chinese Society of Imaging Technology of Chinese Medical Association, Medical Technologist Professional Committee of Chinese Medical Doctor Association, Professional Committee of Medical Imaging Technology of Chinese Medical Education Association. Expert consensus on standard clinical application of DSA examination technical[J]. Chin J Radiol, 2024, 58( 10): 995- 1005. DOI: 10.3760/cma.j.cn112149-20240410-00201.中华医学会影像技术分会, 中国医师协会医学技师专业委员会, 中国医药教育协会医学影像技术学专业委员会. DSA检查技术临床应用专家共识[J]. 中华放射学杂志, 2024, 58( 10): 995- 1005. DOI: 10.3760/cma.j.cn112149-20240410-00201. [40] GINÈS P, KRAG A, ABRALDES JG, et al. Liver cirrhosis[J]. Lancet, 2021, 398( 10308): 1359- 1376. DOI: 10.1016/S0140-6736(21)01374-X. [41] GARCIA-TSAO G, ABRALDES JG, BERZIGOTTI A, et al. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases[J]. Hepatology, 2017, 65( 1): 310- 335. DOI: 10.1002/hep.28906. [42] HARRISON SA, ABDELMALEK MF, CALDWELL S, et al. Simtuzumab is ineffective for patients with bridging fibrosis or compensated cirrhosis caused by nonalcoholic steatohepatitis[J]. Gastroenterology, 2018, 155( 4): 1140- 1153. DOI: 10.1053/j.gastro.2018.07.006. [43] de FRANCHIS R, BOSCH J, GARCIA-TSAO G, et al. Baveno VII-Renewing consensus in portal hypertension[J]. J Hepatol, 2022, 76( 4): 959- 974. DOI: 10.1016/j.jhep.2021.12.022. [44] GARCIA-TSAO G, GROSZMANN RJ, FISHER RL, et al. Portal pressure, presence of gastroesophageal varices and variceal bleeding[J]. Hepatology, 1985, 5( 3): 419- 424. DOI: 10.1002/hep.1840050313. [45] KERBERT AJC, CHIANG FWT, van der WERF M, et al. Hemodynamic response to primary prophylactic therapy with nonselective β-blockers is related to a reduction of first variceal bleeding risk in liver cirrhosis: A meta-analysis[J]. Eur J Gastroenterol Hepatol, 2017, 29( 4): 380- 387. DOI: 10.1097/MEG.0000000000000812. [46] VELDHUIJZEN VAN ZANTEN D, BUGANZA E, ABRALDES JG. The role of hepatic venous pressure gradient in the management of cirrhosis[J]. Clin Liver Dis, 2021, 25( 2): 327- 343. DOI: 10.1016/j.cld.2021.01.002. [47] VILLANUEVA C, GRAUPERA I, ARACIL C, et al. A randomized trial to assess whether portal pressure guided therapy to prevent variceal rebleeding improves survival in cirrhosis[J]. Hepatology, 2017, 65( 5): 1693- 1707. DOI: 10.1002/hep.29056. [48] LV Y, WANG QH, LUO BH, et al. Identifying the optimal measurement timing and hemodynamic targets of portal pressure gradient after TIPS in patients with cirrhosis and variceal bleeding[J]. J Hepatol, 2025, 82( 2): 245- 257. DOI: 10.1016/j.jhep.2024.08.007. [49] RAUTOU PE, ELKRIEF L, DECRAECKER M, et al. Non-invasive diagnosis and follow-up of vascular liver diseases[J]. Clin Res Hepatol Gastroenterol, 2022, 46( 1): 101764. DOI: 10.1016/j.clinre.2021.101764. [50] DAJTI E, RAVAIOLI F, ZYKUS R, et al. Accuracy of spleen stiffness measurement for the diagnosis of clinically significant portal hypertension in patients with compensated advanced chronic liver disease: A systematic review and individual patient data meta-analysis[J]. Lancet Gastroenterol Hepatol, 2023, 8( 9): 816- 828. DOI: 10.1016/S2468-1253(23)00150-4. [51] SEGNA D, MENDOZA YP, LANGE NF, et al. Non-invasive tools for compensated advanced chronic liver disease and portal hypertension after Baveno VII- an update[J]. Dig Liver Dis, 2023, 55( 3): 326- 335. DOI: 10.1016/j.dld.2022.10.009. [52] KUMAR A, MARUYAMA H, ARORA A, et al. Diagnostic accuracy of transient elastography in diagnosing clinically significant portal hypertension in patients with chronic liver disease: A systematic review and meta-analysis[J]. J Med Ultrason, 2022, 49( 3): 333- 346. DOI: 10.1007/s10396-022-01239-x. [53] BERZIGOTTI A. Non-invasive evaluation of portal hypertension using ultrasound elastography[J]. J Hepatol, 2017, 67( 2): 399- 411. DOI: 10.1016/j.jhep.2017.02.003. [54] DAJTI E, RAVAIOLI F, COLECCHIA A, et al. Liver and spleen stiffness measurements for assessment of portal hypertension severity in patients with budd chiari syndrome[J]. Can J Gastroenterol Hepatol, 2019, 2019: 1673197. DOI: 10.1155/2019/1673197. [55] COLECCHIA A, RAVAIOLI F, SESSA M, et al. Liver stiffness measurement allows early diagnosis of veno-occlusive disease/sinusoidal obstruction syndrome in adult patients who undergo hematopoietic stem cell transplantation: Results from a monocentric prospective study[J]. Biol Blood Marrow Transplant, 2019, 25( 5): 995- 1003. DOI: 10.1016/j.bbmt.2019.01.019. [56] DEBUREAUX PE, BOURRIER P, RAUTOU PE, et al. Elastography improves accuracy of early hepato-biliary complications diagnosis after allogeneic stem cell transplantation[J]. Haematologica, 2021, 106( 9): 2374- 2383. DOI: 10.3324/haematol.2019.245407. [57] ELKRIEF L, LAZARETH M, CHEVRET S, et al. Liver stiffness by transient elastography to detect Porto-sinusoidal vascular liver disease with portal hypertension[J]. Hepatology, 2021, 74( 1): 364- 378. DOI: 10.1002/hep.31688. [58] VALLA DC, CAZALS-HATEM D. Vascular liver diseases on the clinical side: Definitions and diagnosis, new concepts[J]. Virchows Arch, 2018, 473( 1): 3- 13. DOI: 10.1007/s00428-018-2331-3. [59] ROCKEY DC, CALDWELL SH, GOODMAN ZD, et al. Liver biopsy[J]. Hepatology, 2009, 49( 3): 1017- 1044. DOI: 10.1002/hep.22742. [60] de GOTTARDI A, RAUTOU PE, SCHOUTEN J, et al. Porto-sinusoidal vascular disease: Proposal and description of a novel entity[J]. Lancet Gastroenterol Hepatol, 2019, 4( 5): 399- 411. DOI: 10.1016/S2468-1253(19)30047-0. [61] BAYRAKTAR UD, SEREN S, BAYRAKTAR Y. Hepatic venous outflow obstruction: Three similar syndromes[J]. World J Gastroenterol, 2007, 13( 13): 1912- 1927. DOI: 10.3748/wjg.v13.i13.1912. [62] YU H, KIRKPATRICK IDC. An update on acute mesenteric ischemia[J]. Can Assoc Radiol J, 2023, 74( 1): 160- 171. DOI: 10.1177/08465371221094280. [63] REINTAM BLASER A, ACOSTA S, ARABI YM. A clinical approach to acute mesenteric ischemia[J]. Curr Opin Crit Care, 2021, 27( 2): 183- 192. DOI: 10.1097/MCC.0000000000000802. [64] LIU FQ. Transjugular intrahepatic portosystemic shunt: Accurate technique and standardized management of the whole process[M]. Beijing: People's Medical Publishing House, 2024.刘福全. 经颈静脉肝内门体静脉分流术: 精准技术与全程规范化管理[M]. 北京: 人民卫生出版社, 2024. [65] ELKRIEF L, HERNANDEZ-GEA V, SENZOLO M, et al. Portal vein thrombosis: Diagnosis, management, and endpoints for future clinical studies[J]. Lancet Gastroenterol Hepatol, 2024, 9( 9): 859- 883. DOI: 10.1016/S2468-1253(24)00155-9. [66] AGENO W, RIVA N, SCHULMAN S, et al. Long-term clinical outcomes of splanchnic vein thrombosis: Results of an international registry[J]. JAMA Intern Med, 2015, 175( 9): 1474- 1480. DOI: 10.1001/jamainternmed.2015.3184. [67] RIVA N, AGENO W, POLI D, et al. Safety of vitamin K antagonist treatment for splanchnic vein thrombosis: A multicenter cohort study[J]. J Thromb Haemost, 2015, 13( 6): 1019- 1027. DOI: 10.1111/jth.12930. [68] OGREN M, BERGQVIST D, BJÖRCK M, et al. Portal vein thrombosis: Prevalence, patient characteristics and lifetime risk: A population study based on 23, 796 consecutive autopsies[J]. World J Gastroenterol, 2006, 12( 13): 2115- 2119. DOI: 10.3748/wjg.v12.i13.2115. [69] GUERRERO A, DEL CAMPO L, PISCAGLIA F, et al. Anticoagulation improves survival in patients with cirrhosis and portal vein thrombosis: The IMPORTAL competing-risk meta-analysis[J]. J Hepatol, 2023, 79( 1): 69- 78. DOI: 10.1016/j.jhep.2023.02.023. [70] NERY F, CHEVRET S, CONDAT B, et al. Causes and consequences of portal vein thrombosis in 1, 243 patients with cirrhosis: Results of a longitudinal study[J]. Hepatology, 2015, 61( 2): 660- 667. DOI: 10.1002/hep.27546. [71] BOZZATO AM, BRUNO O, PAYANCE A, et al. Portal vein thrombosis: Baveno VII consensus recommendations for diagnosis and management[J]. Radiographics, 2023, 43( 11): e230128. DOI: 10.1148/rg.230128. [72] LI Z, XU WT, WANG L, et al. Risk of bleeding in liver cirrhosis receiving direct oral anticoagulants: A systematic review and meta-analysis[J]. Thromb Haemost, 2023, 123( 11): 1072- 1088. DOI: 10.1055/s-0043-1770100. [73] PETTINARI I, VUKOTIC R, STEFANESCU H, et al. Clinical impact and safety of anticoagulants for portal vein thrombosis in cirrhosis[J]. Am J Gastroenterol, 2019, 114( 2): 258- 266. DOI: 10.1038/s41395-018-0421-0. [74] DELGADO MG, SEIJO S, YEPES I, et al. Efficacy and safety of anticoagulation on patients with cirrhosis and portal vein thrombosis[J]. Clin Gastroenterol Hepatol, 2012, 10( 7): 776- 783. DOI: 10.1016/j.cgh.2012.01.012. [75] BAIGES A, PROCOPET B, SILVA-JUNIOR G, et al. Incidence and factors predictive of recurrent thrombosis in people with non-cirrhotic portal vein thrombosis[J]. J Hepatol, 2023, 78( 1): 114- 122. DOI: 10.1016/j.jhep.2022.08.023. [76] LV Y, PAN YL, XIE HH, et al. Timing of TIPS for the management of portal vein thrombosis in liver cirrhosis[J]. J Transl Int Med, 2023, 11( 4): 316- 319. DOI: 10.2478/jtim-2023-0095. [77] SENZOLO M, GARCIA-TSAO G, GARCÍA-PAGÁN JC. Current knowledge and management of portal vein thrombosis in cirrhosis[J]. J Hepatol, 2021, 75( 2): 442- 453. DOI: 10.1016/j.jhep.2021.04.029. [78] LV Y, QI XS, HE CY, et al. Covered TIPS versus endoscopic band ligation plus propranolol for the prevention of variceal rebleeding in cirrhotic patients with portal vein thrombosis: A randomised controlled trial[J]. Gut, 2018, 67( 12): 2156- 2168. DOI: 10.1136/gutjnl-2017-314634. [79] CUI T, WANG T, ZHU B, et al. Short-term efficacy and safety analysis of percutaneous liver puncture for local treatment of portal vein thrombosis[J]. J Pract Radiol, 2024, 40( 8): 1338- 1341. DOI: 10.3969/j.issn.1002-1671.2024.08.027.崔婷, 王涛, 朱冰, 等. 经皮肝穿刺局部处理门静脉血栓形成短期疗效与安全性分析[J]. 实用放射学杂志, 2024, 40( 8): 1338- 1341. DOI: 10.3969/j.issn.1002-1671.2024.08.027. [80] VIOLI F, PIGNATELLI P. Management of portal vein thrombosis in cirrhosis[J]. Lancet Gastroenterol Hepatol, 2024, 9( 12): 1080- 1081. DOI: 10.1016/S2468-1253(24)00312-1. [81] GAO FB, WANG L, PAN JH, et al. Efficacy and safety of thrombolytic therapy for portal venous system thrombosis: A systematic review and meta-analysis[J]. J Intern Med, 2023, 293( 2): 212- 227. DOI: 10.1111/joim.13575. [82] TIAN YQ, DHARA S, BARRETT CD, et al. Antibiotic use in acute mesenteric ischemia: A review of the evidence and call to action[J]. Thromb J, 2023, 21( 1): 39. DOI: 10.1186/s12959-023-00486-3. [83] TILSED JVT, CASAMASSIMA A, KURIHARA H, et al. ESTES guidelines: Acute mesenteric ischaemia[J]. Eur J Trauma Emerg Surg, 2016, 42( 2): 253- 270. DOI: 10.1007/s00068-016-0634-0. [84] HERNÁNDEZ-GEA V, BAIGES A, TURON F, et al. Idiopathic portal hypertension[J]. Hepatology, 2018, 68( 6): 2413- 2423. DOI: 10.1002/hep.30132. [85] HE FL, MA L, LI YR, et al. Non-cirrhotic portal hypertension: The highlight of its diagnosis[J]. J Pract Hepatol, 2022, 25( 1): 1- 4. DOI: 10.3969/j.issn.1672-5069.2022.01.001.何福亮, 马琳, 李悦榕, 等. 非肝硬化性门脉高压的临床诊断[J]. 实用肝脏病杂志, 2022, 25( 1): 1- 4. DOI: 10.3969/j.issn.1672-5069.2022.01.001. [86] CAI ZH, ZHUGE YZ. Disease characteristics, diagnosis and treatment progress of vascular diseases of portal vein and hepatic sinus[J]. Chin Hepatol, 2023, 28( 2): 148- 151. DOI: 10.14000/j.cnki.issn.1008-1704.2023.02.007.蔡子豪, 诸葛宇征. 门静脉肝窦血管性疾病的疾病特点与诊疗进展[J]. 肝脏, 2023, 28( 2): 148- 151. DOI: 10.14000/j.cnki.issn.1008-1704.2023.02.007. [87] BISSONNETTE J, GARCIA-PAGÁN JC, ALBILLOS A, et al. Role of the transjugular intrahepatic portosystemic shunt in the management of severe complications of portal hypertension in idiopathic noncirrhotic portal hypertension[J]. Hepatology, 2016, 64( 1): 224- 231. DOI: 10.1002/hep.28547. [88] HU GH, SHEN LG, YANG J, et al. Insight into congenital absence of the portal vein: Is it rare?[J]. World J Gastroenterol, 2008, 14( 39): 5969- 5979. DOI: 10.3748/wjg.14.5969. [89] SAVALE L, GUIMAS M, EBSTEIN N, et al. Portopulmonary hypertension in the current era of pulmonary hypertension management[J]. J Hepatol, 2020, 73( 1): 130- 139. DOI: 10.1016/j.jhep.2020.02.021. [90] KIM MJ, KO JS, SEO JK, et al. Clinical features of congenital portosystemic shunt in children[J]. Eur J Pediatr, 2012, 171( 2): 395- 400. DOI: 10.1007/s00431-011-1564-9. [91] DIPAOLA F, TROUT AT, WALTHER AE, et al. Congenital portosystemic shunts in children: Associations, complications, and outcomes[J]. Dig Dis Sci, 2020, 65( 4): 1239- 1251. DOI: 10.1007/s10620-019-05834-w. [92] EVANS WN, GALINDO A, ACHERMAN RJ, et al. Congenital portosystemic shunts and AMPLATZER vascular plug occlusion in newborns[J]. Pediatr Cardiol, 2009, 30( 8): 1083- 1088. DOI: 10.1007/s00246-009-9501-7. [93] RAJU SN, PANDEY NN, SINGH SP, et al. Successful embolization of type II congenital extrahepatic portosystemic shunt using amplatzer septal occluder and amplatzer vascular plug II[J]. J Vasc Interv Radiol, 2021, 32( 8): 1236- 1237. DOI: 10.1016/j.jvir.2021.05.022. [94] FRANCHI-ABELLA S, GONZALES E, ACKERMANN O, et al. Congenital portosystemic shunts: Diagnosis and treatment[J]. Abdom Radiol, 2018, 43( 8): 2023- 2036. DOI: 10.1007/s00261-018-1619-8. [95] BLANC T, GUERIN F, FRANCHI-ABELLA S, et al. Congenital portosystemic shunts in children: A new anatomical classification correlated with surgical strategy[J]. Ann Surg, 2014, 260( 1): 188- 198. DOI: 10.1097/SLA.0000000000000266. [96] FAUGHNAN ME, MAGER JJ, HETTS SW, et al. Second international guidelines for the diagnosis and management of hereditary hemorrhagic telangiectasia[J]. Ann Intern Med, 2020, 173( 12): 989- 1001. DOI: 10.7326/M20-1443. [97] GARCIA-TSAO G, KORZENIK JR, YOUNG L, et al. Liver disease in patients with hereditary hemorrhagic telangiectasia[J]. N Engl J Med, 2000, 343( 13): 931- 936. DOI: 10.1056/NEJM200009283431305. [98] GARG N, KHUNGER M, GUPTA A, et al. Optimal management of hereditary hemorrhagic telangiectasia[J]. J Blood Med, 2014, 5: 191- 206. DOI: 10.2147/JBM.S45295. [99] VÁZQUEZ C, GONZALEZ ML, FERRARIS A, et al. Bevacizumab for treating Hereditary Hemorrhagic Telangiectasia patients with severe hepatic involvement or refractory Anemia[J]. PLoS One, 2020, 15( 2): e0228486. DOI: 10.1371/journal.pone.0228486. [100] DUPUIS-GIROD S, GINON I, SAURIN JC, et al. Bevacizumab in patients with hereditary hemorrhagic telangiectasia and severe hepatic vascular malformations and high cardiac output[J]. JAMA, 2012, 307( 9): 948- 955. DOI: 10.1001/jama.2012.250. [101] FELLI E, ADDEO P, FAITOT F, et al. Liver transplantation for hereditary hemorrhagic telangiectasia: A systematic review[J]. HPB, 2017, 19( 7): 567- 572. DOI: 10.1016/j.hpb.2017.03.005. [102] LEE M, SZE DY, BONHAM CA, et al. Hepatic arteriovenous malformations from hereditary hemorrhagic telangiectasia: Treatment with liver transplantation[J]. Dig Dis Sci, 2010, 55( 11): 3059- 3062. DOI: 10.1007/s10620-010-1353-8. [103] VAUTHEY JN, TOMCZAK RJ, HELMBERGER T, et al. The arterioportal fistula syndrome: Clinicopathologic features, diagnosis, and therapy[J]. Gastroenterology, 1997, 113( 4): 1390- 1401. DOI: 10.1053/gast.1997.v113.pm9322535. [104] WAKIL A, MOHAMED M, AL-HILLAN A, et al. S2839 Non-cirrhotic portal hypertension secondary to hepatic arterioportal fistula[J]. Am J Gastroenterol, 2021, 116( 1): S1179- S1180. DOI: 10.14309/01.ajg.0000784888.16068.ec. [105] XIA JL, ZHAO JW, CHANG B. Case report: Congenital arterioportal fistula: An unusual cause of variceal bleeding in adults[J]. Front Med, 2022, 9: 970254. DOI: 10.3389/fmed.2022.970254. [106] CHOI JW, LEE JM, KIM HC, et al. Iatrogenic arterioportal fistula caused by radiofrequency ablation of hepatocellular carcinoma: Clinical course and treatment outcomes[J]. J Vasc Interv Radiol, 2020, 31( 5): 728- 736. DOI: 10.1016/j.jvir.2019.10.020. [107] AHN JH, YU JS, HWANG SH, et al. Nontumorous arterioportal shunts in the liver: CT and MRI findings considering mechanisms and fate[J]. Eur Radiol, 2010, 20( 2): 385- 394. DOI: 10.1007/s00330-009-1542-z. [108] LYU TS, XIE Y, SHE K, et al. Symptomatic hepatic arterioportal fistula-related portal vein hypertension[J]. J Vasc Surg Venous Lymphat Disord, 2025, 13( 1): 101888. DOI: 10.1016/j.jvsv.2024.101888. [109] GUZMAN EA, MCCAHILL LE, ROGERS FB. Arterioportal fistulas: Introduction of a novel classification with therapeutic implications[J]. J Gastrointest Surg, 2006, 10( 4): 543- 550. DOI: 10.1016/j.gassur.2005.06.022. [110] MOHTY M, MALARD F, ABECASSIS M, et al. Revised diagnosis and severity criteria for sinusoidal obstruction syndrome/veno-occlusive disease in adult patients: A new classification from the European Society for Blood and Marrow Transplantation[J]. Bone Marrow Transplant, 2016, 51( 7): 906- 912. DOI: 10.1038/bmt.2016.130. [111] CORBACIOGLU S, CARRERAS E, ANSARI M, et al. Diagnosis and severity criteria for sinusoidal obstruction syndrome/veno-occlusive disease in pediatric patients: A new classification from the European society for blood and marrow transplantation[J]. Bone Marrow Transplant, 2018, 53( 2): 138- 145. DOI: 10.1038/bmt.2017.161. [112] MOHTY M, MALARD F, ABECASIS M, et al. Prophylactic, preemptive, and curative treatment for sinusoidal obstruction syndrome/veno-occlusive disease in adult patients: A position statement from an international expert group[J]. Bone Marrow Transplant, 2020, 55( 3): 485- 495. DOI: 10.1038/s41409-019-0705-z. [113] Cooperative Group for Hepatic and Gall Diseases, Chinese Society of Gastroenterology, Chinese Medical Association. Expert consensus on diagnosis and treatment of pyrrolidine alkaloids-related sinusoidal obstruction syndrome(2017, Nanjing)[J]. J Clin Hepatol, 2017, 33( 9): 1627- 1637. DOI: 10.3969/j.issn.1001-5256.2017.09.003.中华医学会消化病学分会肝胆疾病协作组. 吡咯生物碱相关肝窦阻塞综合征诊断和治疗专家共识意见(2017年,南京)[J]. 临床肝胆病杂志, 2017, 33( 9): 1627- 1637. DOI: 10.3969/j.issn.1001-5256.2017.09.003. [114] MOHTY M, MALARD F, ALASKAR AS, et al. Diagnosis and severity criteria for sinusoidal obstruction syndrome/veno-occlusive disease in adult patients: A refined classification from the European society for blood and marrow transplantation(EBMT)[J]. Bone Marrow Transplant, 2023, 58( 7): 749- 754. DOI: 10.1038/s41409-023-01992-8. [115] NISHIDA M, SUGITA J, TAKAHASHI S, et al. Refined ultrasonographic criteria for sinusoidal obstruction syndrome after hematopoietic stem cell transplantation[J]. Int J Hematol, 2021, 114( 1): 94- 101. DOI: 10.1007/s12185-021-03137-3. [116] KAN XF, YE J, RONG XX, et al. Diagnostic performance of contrast-enhanced CT in pyrrolizidine alkaloids-induced hepatic sinusoidal obstructive syndrome[J]. Sci Rep, 2016, 6: 37998. DOI: 10.1038/srep37998. [117] GRESSENS SB, CAZALS-HATEM D, LLOYD V, et al. Hepatic venous pressure gradient in sinusoidal obstruction syndrome: Diagnostic value and link with histological lesions[J]. JHEP Rep, 2022, 4( 11): 100558. DOI: 10.1016/j.jhepr.2022.100558. [118] GRUPP SA, CORBACIOGLU S, KANG HJ, et al. A phase 3, randomized, adaptive study of defibrotide(DF) vs best supportive care(BSC) for the prevention of hepatic veno-occlusive disease/sinusoidal obstruction syndrome(VOD/SOS) in patients(pts) undergoing hematopoietic cell transplantation(HCT): Preliminary results[J]. Blood, 2021, 138( Supplement 1): 749. DOI: 10.1182/blood-2021-147284. [119] ZHANG W, ZHUGE YZ. Anticoagulant therapy and transjugular intrahepatic portosystemic shunt for pyrrolizidine alkaloid related hepatic sinusoidal obstruction syndrome[J]. J Clin Hepatol, 2022, 38( 6): 1234- 1236. DOI: 10.3969/j.issn.1001-5256.2022.06.005.张玮, 诸葛宇征. 吡咯里西啶生物碱相关肝窦阻塞综合征的抗凝-经颈静脉肝内门体分流术阶梯治疗[J]. 临床肝胆病杂志, 2022, 38( 6): 1234- 1236. DOI: 10.3969/j.issn.1001-5256.2022.06.005. [120] COPELAN A, REMER EM, SANDS M, et al. Diagnosis and management of budd chiari syndrome: An update[J]. CardioVascular Interv Radiol, 2015, 38( 1): 1- 12. DOI: 10.1007/s00270-014-0919-9. [121] GARCIA-PAGÁN JC, VALLA DC. Primary budd-chiari syndrome[J]. N Engl J Med, 2023, 388( 14): 1307- 1316. DOI: 10.1056/nejmra2207738. [122] LYU LL, XU P. Hepatic CT perfusion in budd-chiari syndrome before and after intervention[J]. Radiology, 2024, 311( 1): e232426. DOI: 10.1148/radiol.232426. [123] European Association for the Study of the Liver. EASL clinical practice guidelines: Vascular diseases of the liver[J]. J Hepatol, 2016, 64( 1): 179- 202. DOI: 10.1016/j.jhep.2015.07.040. [124] MANCUSO A, AMATA M, POLITI F, et al. Controversies in budd-chiari syndrome management: Potential role of liver stiffness[J]. Am J Gastroenterol, 2020, 115( 6): 952- 953. DOI: 10.14309/ajg.0000000000000586. [125] SHUKLA A, SHRESHTHA A, MUKUND A, et al. Budd-Chiari syndrome: Consensus guidance of the Asian Pacific Association for the study of the liver(APASL)[J]. Hepatol Int, 2021, 15( 3): 531- 567. DOI: 10.1007/s12072-021-10189-4. [126] DELEVE LD, VALLA DC, GARCIA-TSAO G. Vascular disorders of the liver[J]. Hepatology, 2009, 49( 5): 1729- 1764. DOI: 10.1002/hep.22772. [127] PATEL RK, CHANDEL K, TRIPATHY T, et al. Interventions in Budd-Chiari syndrome: An updated review[J]. Abdom Radiol, 2025, 50( 3): 1307- 1319. DOI: 10.1007/s00261-024-04558-4. [128] WANG ZG, ZHANG FJ, YI MQ, et al. Evolution of management for Budd-Chiari syndrome: A team's view from 2564 patients[J]. ANZ J Surg, 2005, 75( 1-2): 55- 63. DOI: 10.1111/j.1445-2197.2005.03135.x. [129] WANG QH, LUO BH, XIA DD, et al. WED-167 Recanalization for Budd-Chiari syndrome and development of a prognostic score: A multicentre study of 834 cases from China[J]. J Hepatol, 2024, 80: S716. DOI: 10.1016/S0168-8278(24)02024-5. [130] MORENO MOA, SILVA LIMA PAZ CL DA, DEZAN MGF, et al. Ten-year outcomes of tips for budd-chiari syndrome: Systematic review and meta-analysis[J]. Arq Gastroenterol, 2024, 61: e23171. DOI: 10.1590/S0004-2803.24612023-171. [131] MANCUSO A. Timing of transjugular intrahepatic portosystemic shunt for budd-chiari syndrome: An Italian hepatologist's perspective[J]. J Transl Int Med, 2017, 5( 4): 194- 199. DOI: 10.1515/jtim-2017-0033. [132] RÖSSLE M. Interventional treatment of budd-chiari syndrome[J]. Diagnostics, 2023, 13( 8): 1458. DOI: 10.3390/diagnostics13081458. [133] ROSENQVIST K, SHEIKHI R, ERIKSSON LG, et al. Endovascular treatment of symptomatic Budd-Chiari syndrome-in favour of early transjugular intrahepatic portosystemic shunt[J]. Eur J Gastroenterol Hepatol, 2016, 28( 6): 656- 660. DOI: 10.1097/MEG.0000000000000621. [134] JOUEIDI F, ALHANAEE A, ALSUHAIBANI H, et al. Transjugular intrahepatic portosystemic shunt for budd-chiari syndrome: A single-centre experience[J]. J Clin Med, 2024, 13( 19): 5858. DOI: 10.3390/jcm13195858. [135] AKABANE M, IMAOKA Y, NAKAYAMA T, et al. Effect of TIPS insertion on waitlist mortality and access to liver transplantation in Budd-Chiari syndrome[J]. Liver Transpl, 2025, 31( 2): 151- 160. DOI: 10.1097/LVT.0000000000000469. [136] SONG AT, AVELINO-SILVA VI, PECORA RA, et al. Liver transplantation: fifty years of experience[J]. World J Gastroenterol, 2014, 20( 18): 5363- 5374. DOI: 10.3748/wjg.v20.i18.5363. [137] ZU MH, XU H, ZHANG QQ, et al. Review of budd-chiari syndrome[J]. J Interv Med, 2020, 3( 2): 65- 76. DOI: 10.1016/j.jimed.2020.03.002. [138] DONGELMANS E, ERLER N, ADAM R, et al. Recent outcomes of liver transplantation for Budd-Chiari syndrome: A study of the European Liver Transplant Registry(ELTR) and affiliated centers[J]. Hepatology, 2024, 80( 1): 136- 151. DOI: 10.1097/HEP.0000000000000778. [139] SEMMLER G, LINDORFER A, SCHÄFER B, et al. Outcome of budd-chiari syndrome patients treated with direct oral anticoagulants: An Austrian multicenter study[J]. Clin Gastroenterol Hepatol, 2023, 21( 4): 978- 987.e2. DOI: 10.1016/j.cgh.2022.04.024. [140] JINDAL A, MUKUND A. Direct oral anticoagulants in budd-chiari syndrome: Need a closer look![J]. Clin Gastroenterol Hepatol, 2023, 21( 4): 1117. DOI: 10.1016/j.cgh.2022.05.034. [141] HEIDENREICH PA, BOZKURT B, AGUILAR D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: A report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines[J]. Circulation, 2022, 145( 18): e895- e1032. DOI: 10.1161/CIR.0000000000001063. [142] FORTEA JI, PUENTE Á, CUADRADO A, et al. Congestive hepatopathy[J]. Int J Mol Sci, 2020, 21( 24): 9420. DOI: 10.3390/ijms21249420. [143] LEMMER A, van WAGNER LB, GANGER D. Assessment of advanced liver fibrosis and the risk for hepatic decompensation in patients with congestive hepatopathy[J]. Hepatology, 2018, 68( 4): 1633- 1641. DOI: 10.1002/hep.30048. [144] GUO ZY, YE ZX, XU QF, et al. Association of liver fibrosis scores with all-cause and cardiovascular mortality in patients with heart failure[J]. Clin Transl Sci, 2024, 17( 12): e70104. DOI: 10.1111/cts.70104. [145] PONIKOWSKI P, VOORS AA, ANKER SD, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology(ESC). Developed with the special contribution of the Heart Failure Association(HFA) of the ESC[J]. Eur J Heart Fail, 2016, 18( 8): 891- 975. DOI: 10.1002/ejhf.592. [146] MEHRA MR, CANTER CE, HANNAN MM, et al. The 2016 International Society for Heart Lung Transplantation listing criteria for heart transplantation: A 10-year update[J]. J Heart Lung Transplant, 2016, 35( 1): 1- 23. DOI: 10.1016/j.healun.2015.10.023. [147] BERG CJ, BAUER BS, HAGEMAN A, et al. Mortality risk stratification in fontan patients who underwent heart transplantation[J]. Am J Cardiol, 2017, 119( 10): 1675- 1679. DOI: 10.1016/j.amjcard.2017.02.005. -



 PDF下载 ( 22502 KB)
PDF下载 ( 22502 KB)

 下载:
下载: