丙型肝炎病毒/乙型肝炎病毒重叠感染者的血清学特征分析
DOI: 10.12449/JCH260109
Serological characteristics of individuals with hepatitis C virus/hepatitis B virus overlapping infection
-
摘要:
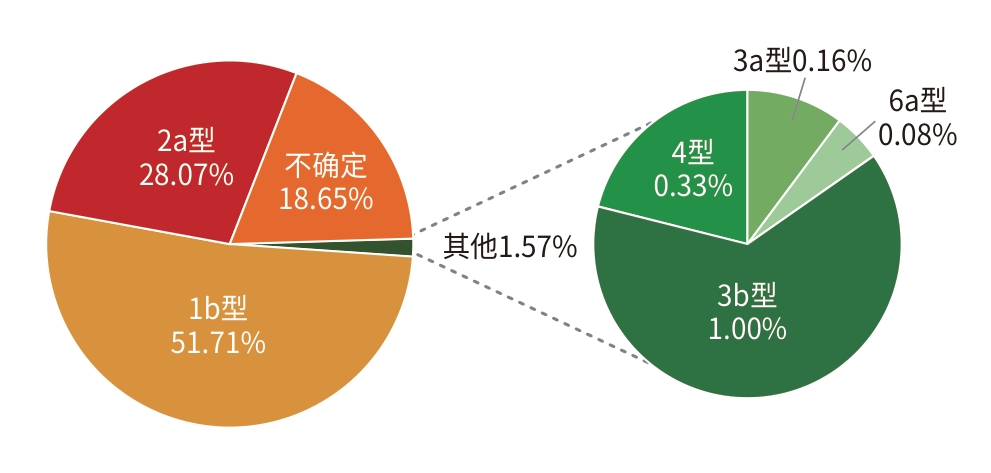
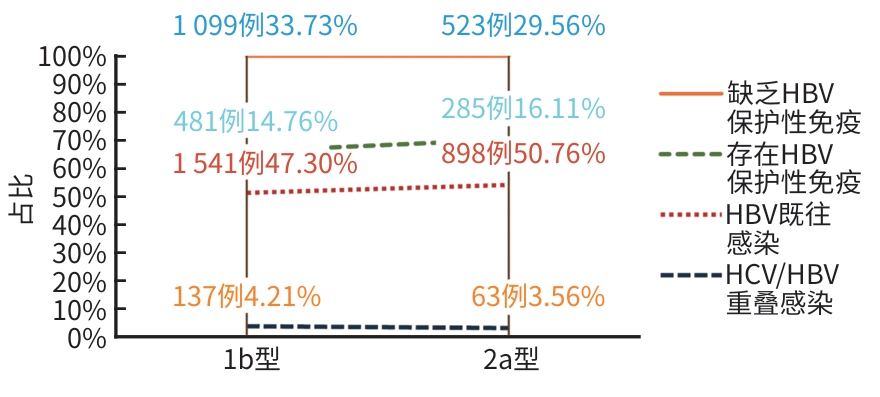
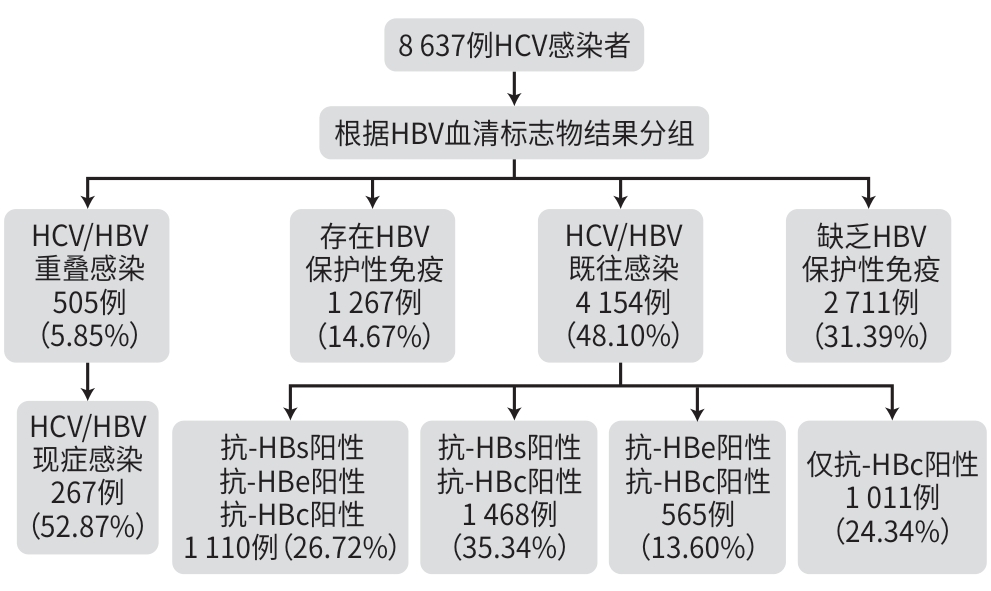
目的 探讨慢性丙型肝炎病毒(HCV)感染者中重叠乙型肝炎病毒(HBV)感染的状况及其血清学特征分析。 方法 选取中国人民解放军总医院第五医学中心2010年1月1日—2020年12月31日住院患者中HBV血清标志物资料完整的HCV感染者8 637例,分析HCV感染者中重叠HBV血清学标志物的构成比,按年龄、出生年份分组分析患者的血清学特征,并进一步分析不同HCV基因型的HBV相关血清学特征分布。 结果 HCV/HBV重叠感染者占5.85%;HBV既往感染者占48.10%;存在HBV保护性免疫者占14.67%;缺乏HBV保护性免疫者占31.39%。按不同年龄将患者分组:0~17岁以存在HBV保护性免疫人群为主(61.41%,304例);18~44岁以HBV既往感染人群为主(37.31%,698例);45~59岁以HBV既往感染人群为主(50.38%,1 945例);≥60岁以HBV既往感染人群为主(61.66%,1 486例)。按不同出生年份将患者分组:1992年以前以HBV既往感染人群为主(51.63%,4 112例);1992—2005年以存在HBV保护性免疫人群为主(54.72%,168例);2005年以后以存在HBV保护性免疫人群为主(64.38%,235例)。本研究中6 301例患者进行了HCV基因型检测:基因1b型占比最多(51.71%,3 258例),基因2a型占28.07%(1 769例),基因3b型占1.00%(63例),基因3a型占0.16%(10例),基因4型占0.33%(21例),基因6a型占0.08%(5例)。 结论 随着我国乙型肝炎疫苗计划免疫政策的推行,HCV重叠HBV感染者中HBV既往感染者比例明显降低,但仍存在较高比例人群缺乏HBV保护性免疫。 Abstract:Objective To investigate the status of overlapping hepatitis B virus (HBV) infection in patients with chronic hepatitis C virus (HCV) infection and the serological characteristics of such patients. Methods A total of 8 637 patients with HCV infection who were hospitalized from January 1, 2010 to December 31, 2020 and had complete data of HBV serological markers were enrolled, and the composition ratio of patients with overlapping HBV serological markers was analyzed among the patients with HCV infection. The patients were divided into groups based on age and year of birth, and serological characteristics were analyzed, and the distribution of HBV-related serological characteristics were analyzed across different HCV genotypes. Results The patients with HCV/HBV overlapping infection accounted for 5.85%, and the patients with previous HBV infection accounted for 48.10%; the patients with protective immunity against HBV accounted for 14.67%, while the patients with a lack of protective immunity against HBV accounted for 31.39%. The patients were divided into groups based on age: in the 0 — 17 years group, the patients with protective immunity against HBV accounted for 61.41% (304 patients); the 18 — 44 years group was mainly composed of patients with previous HBV infection (698 patients, 37.31%), the 45 — 59 years group was predominantly composed of patients with previous HBV infection (1 945 patients, 50.38%), and the ≥60 years group was also predominantly composed of patients with previous HBV infection (1 486 patients, 61.66%). The patients were divided into groups based on the year of birth: in the pre-1992 group, the patients with previous HBV infection accounted for 51.63% (4 112 patients); in the 1992 — 2005 group, the patients with protective immunity against HBV accounted for 54.72% (168 patients); in the post-2005 group, the patients with protective immunity against HBV accounted for 64.38% (235 patients). In this study, 6 301 patients underwent HCV genotype testing: the patients with genotype 1b accounted for the highest proportion of 51.71% (3 258 patients), followed by those with genotype 2a (1 769 patients, 28.07%), genotype 3b (63 patients, 1.00%), genotype 3a (10 patients, 0.16%), genotype 4 (21 patients, 0.33%), and genotype 6a (5 patients, 0.08%). Conclusion With the implementation of hepatitis B planned vaccination program in China, there has been a significant reduction in the proportion of patients with previous HBV infection among the patients with HCV/HBV overlapping infection, but there is still a relatively high proportion of patients with a lack of protective immunity against HBV. -
Key words:
- Hepatitis B Virus /
- Hepatitis C Virus /
- Superinfection /
- Hepatitis B Virus Markers
-
表 1 HCV感染者中不同HBV相关血清学特征的年龄分布
Table 1. Age distribution of different HBV related serological characteristics among HCV infected individuals
组别 0~17岁[例(%)] 18~44岁[例(%)] 45~59岁[例(%)] ≥60岁[例(%)] HCV/HBV重叠感染 5(1.01) 123(6.57) 266(6.89) 111(4.61) HBV既往感染 25(5.05) 698(37.31) 1 945(50.38) 1 486(61.66) 存在HBV保护性免疫 304(61.41) 438(23.41) 359(9.30) 166(6.89) 缺乏HBV保护性免疫 161(32.53) 612(32.71) 1 291(33.44) 647(26.85) 合计 495 1 871 3 861 2 410 注:HCV,丙型肝炎病毒;HBV,乙型肝炎病毒。
表 2 不同出生年代HCV感染者的HBV相关血清学特征分布
Table 2. Distribution of HBV related serological characteristics in HCV infected individuals of different birth years
组别 1992年以前
[例(%)]1992—2005年
[例(%)]2005年以后
[例(%)]HCV/HBV重叠感染 495(6.21) 9(2.93) 1(0.27) HBV既往感染 4 112(51.63) 25(8.14) 17(4.66) 存在HBV保护性免疫 864(10.85) 168(54.72) 235(64.38) 缺乏HBV保护性免疫 2 494(31.31) 105(34.20) 112(30.68) 合计 7 965 307 365 注:HCV,丙型肝炎病毒;HBV,乙型肝炎病毒。
-
[1] LIU ZH, HOU JL. Hepatitis B virus(HBV) and hepatitis C virus(HCV) dual infection[J]. Int J Med Sci, 2006, 3( 2): 57- 62. DOI: 10.7150/ijms.3.57. [2] Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Infectious Diseases, Chinese Medical Association. Guidelines for prevention and treatment of chronic hepatitis B(2022 Edition)[J]. Infect Dis Info, 2023, 36( 1): 1- 17. DOI: 10.3969/j.issn.1007-8134.2023.01.01中华医学会肝病学分会, 中华医学会感染病学分会. 慢性乙型肝炎防治指南(2022年版)[J]. 传染病信息, 2023, 36( 1): 1- 17. DOI: 10.3969/j.issn.1007-8134.2023.01.01. [3] Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Infectious Diseases, Chinese Medical Association. Guidelines for the prevention and treatment of hepatitis C(2022 Edition)[J]. Chin J Infect Dis, 2023, 41( 1): 29- 46. DOI: 10.3760/cmaj.cn311365-20230217-00045.中华医学会肝病学分会, 中华医学会感染病学分会. 丙型肝炎防治指南(2022年版)[J]. 中华传染病杂志, 2023, 41( 1): 29- 46. DOI: 10.3760/cma.j.cn311365-20230217-00045. [4] World Health Organization. 1.3 million people die from viral hepatitis every year![EB/OL].( 2024-04-21)[ 2025-03-06]. https://www.163.com/dy/article/J0N5E1OK0552ZA4S.html. https: //www.163.com/dy/article/J0N5E1OK0552ZA4S.html [5] SAYED D, BAKRY R, MIKHAIL N, et al. The prevalence of infection and potential risk factors for HBV and HCV among healthcare workers not vaccinated against HBV: A study from a cancer center in Egypt, 2021-2022[J]. Arab J Gastroenterol, 2025, 26( 2): 201- 206. DOI: 10.1016/j.ajg.2025.01.013. [6] YANG J, RAO HY. EASL recommendations on treatment of hepatitis C: Final update of the series(2020)[J]. J Clin Hepatol, 2020, 36( 12): 2681- 2687. DOI: 10.3969/j.issn.1001-5256.2020.12.009.杨甲, 饶慧瑛. 2020年欧洲肝病学会推荐意见: 丙型肝炎的治疗(最终更新版)[J]. 临床肝胆病杂志, 2020, 36( 12): 2681- 2687. DOI: 10.3969/j.issn.1001-5256.2020.12.009. [7] XIE YD, FENG B, RAO HY. Interpretation of guidelines for the prevention and treatment of chronic hepatitis B(2022 edition)[J]. J Clin Hepatol, 2023, 39( 7): 1553- 1559. DOI: 10.3969/j.issn.1001-5256.2023.07.007.谢艳迪, 封波, 饶慧瑛.《慢性乙型肝炎防治指南(2022年版)》解读[J]. 临床肝胆病杂志, 2023, 39( 7): 1553- 1559. DOI: 10.3969/j.issn.1001-5256.2023.07.007. [8] MAVILIA MG, WU GY. HBV-HCV coinfection: Viral interactions, management, and viral reactivation[J]. J Clin Transl Hepatol, 2018, 6( 3): 296- 305. DOI: 10.14218/JCTH.2018.00016. [9] Stem Cell Application Group, Chinese Society of Hematology, Chinese Medical Association. Chinese expert consensus on prevention of hepatitis B virus reactivation after allogeneic hematopoietic stem cell transplantation(2023)[J]. Chin J Hematol, 2023, 44( 6): 441- 448. DOI: 10.3760/cma/j.issn.0253-2727.2023.06.001.中华医学会血液学分会造血干细胞应用学组. 异基因造血干细胞移植后防治乙型肝炎病毒再激活中国专家共识(2023年版)[J]. 中华血液学杂志, 2023, 44( 6): 441- 448. DOI: 10.3760/cma.j.issn.0253-2727.2023.06.001. [10] DANG RB, ZHANG SX, ZHANG WD, et al. Assessment for immune effectiveness of hepatitis B vaccination among infant population in China[J]. Chin J Public Health, 2009, 25( 4): 385- 387. DOI: 10.3321/j.issn: 1001-0580.2009.04.001.党如波, 张顺祥, 张卫东, 等. 中国新生儿乙肝疫苗免疫效果评估[J]. 中国公共卫生, 2009, 25( 4): 385- 387. DOI: 10.3321/j.issn: 1001-0580.2009.04.001. [11] RAZAVI-SHEARER D, KONDILI L, HALL S, et al. WED-034 Prevalence of HBV and HCV among migrants in EU-27: The impact of the Ukrainian refugee crisis[J]. J Hepatol, 2025, 82: S695- S696. DOI: 10.1016/S0168-8278(25)01837-9. [12] LIU YQ, YANG F, LI L, et al. Study on the overlapping infection of hepatitis B and hepatitis C in Shandong Province[J]. Chongqing Med, 2018, 47( 10): 1389- 1391. DOI: 10.3969/j.issn.1671-8348.2018.10.026.刘义庆, 杨帆, 李丽, 等. 山东地区人群乙型肝炎和丙型肝炎重叠感染情况研究[J]. 重庆医学, 2018, 47( 10): 1389- 1391. DOI: 10.3969/j.issn.1671-8348.2018.10.026. [13] LI FY, FENG Y, LIU X, et al. HBV and HCV co-infection in Chinese newly diagnosed HIV+ subjects in 2015 and 2023: A cross-sectional study[J]. Pathogens, 2024, 13( 5): 367. DOI: 10.3390/pathogens13050367. [14] DESIKAN P, RANGNEKAR A, KHAN Z, et al. Sero-occurrence of HBV/HCV co-infection and levels of liver enzymes among patients at a tertiary care hospital in central India: A pilot study[J]. Cent Asian J Glob Health, 2019, 8( 1): 313. DOI: 10.5195/cajgh.2019.313. [15] WANG L, LIU N, YANG H, et al. Analysis on epidemic trend and spatio-temporal clustering of hepatitis B in China from 2006 to 2020[J]. Chin J Epidemiol, 2025, 46( 3): 410- 417. DOI: 10.3760/cma.j.cn112338-2024-1031-00676.王磊, 刘娜, 杨宏, 等. 2006—2020年中国乙型肝炎流行趋势和时空聚集性分析[J]. 中华流行病学杂志, 2025, 46( 3): 410- 417. DOI: 10.3760/cma.j.cn112338-20241031-00676. [16] WANG X, PAN F. China still faces great challenges in eliminating hepatitis B[J]. China Mod Med, 2025, 32( 2): 1- 3. DOI: 10.3969/j.issn.1674-4721.2025.02.002.王霞, 潘锋. 我国消除乙肝仍面临巨大挑战[J]. 中国当代医药, 2025, 32( 2): 1- 3. DOI: 10.3969/j.issn.1674-4721.2025.02.002. [17] ZAMANI K, ROSTAMI P, DAREHBAGH RR, et al. Hepatitis B and C virus infection and risk of multiple myeloma: A systematic review and meta-analysis[J]. BMC Cancer, 2025, 25( 1): 998. DOI: 10.1186/s12885-025-14420-5. [18] ZARĘBSKA-MICHALUK D, BRZDĘK M, RZYMSKI P, et al. Hepatitis B virus coinfection in patients treated for chronic hepatitis C: Clinical characteristics, risk of reactivation with long-term follow-up, and effectiveness of antiviral therapy[J]. Pol Arch Intern Med, 2024, 134( 1): 16638 DOI: 10.20452/pamw.16638. [19] DECORSIÈRE A, MUELLER H, van BREUGEL PC, et al. Hepatitis B virus X protein identifies the Smc5/6 complex as a host restriction factor[J]. Nature, 2016, 531( 7594): 386- 389. DOI: 10.1038/nature17170. [20] AWADH AA, ALHARTHI AA, ALGHAMDI BA, et al. Coinfection of hepatitis B and C viruses and risk of hepatocellular carcinoma: Systematic review and meta-analysis[J]. J Glob Infect Dis, 2024, 16( 4): 127- 134. DOI: 10.4103/jgid.jgid_211_23. [21] ZHOU DQ, LIU JY, ZHAO F, et al. Risk factors for hepatocellular carcinoma in cirrhosis: A comprehensive analysis from a decade-long study[J]. World J Gastrointest Oncol, 2024, 16( 12): 4625- 4635. DOI: 10.4251/wjgo.v16.i12.4625. [22] HUANG M, WANG DY, HUANG J, et al. Hepatitis B virus promotes liver cancer by modulating the immune response to environmental carcinogens[J]. Nat Commun, 2025, 16( 1): 5360. DOI: 10.1038/s41467-025-60894-z. [23] SAJID MS, VARGHESE RS, KROEMER A, et al. Low-abundance serum protein biomarker candidates for HCC in patients with liver cirrhosis[J]. J Proteome Res, 2025, 24( 7): 3656- 3665. DOI: 10.1021/acs.jproteome.5c00231. [24] YAN LB, RAO HY, MA YJ, et al. Hepatitis B virus infection in Chinese patients with hepatitis C virus infection: Prevalence, clinical characteristics, viral interactions and host genotypes: A nationwide cross-sectional study[J]. BMJ Open, 2016, 6( 10): e012016. DOI: 10.1136/bmjopen-2016-012016. [25] WANG N, ZHAO SM, CHENG Q, et al. Meta-analysis of the association between super infection of HBV, HCV and primary liver cancer in China[J]. J Mod Oncol, 2015, 23( 15): 2169- 2172. DOI: 10.3969/j.issn.1672-4992.2015.15.027.王宁, 赵四敏, 程琦, 等. 我国HBV、HCV重叠感染与原发性肝癌关系的Meta分析[J]. 现代肿瘤医学, 2015, 23( 15): 2169- 2172. DOI: 10.3969/j.issn.1672-4992.2015.15.027. [26] CHEN Y, YU CS, YIN XR, et al. Hepatitis C virus genotypes and subtypes circulating in Mainland China[J]. Emerg Microbes Infect, 2017, 6( 11): e95. DOI: 10.1038/emi.2017.77. [27] RAO HY, WEI L, LOPEZ-TALAVERA JC, et al. Distribution and clinical correlates of viral and host genotypes in Chinese patients with chronic hepatitis C virus infection[J]. J Gastroenterol Hepatol, 2014, 29( 3): 545- 553. DOI: 10.1111/jgh.12398. [28] ZHANG B, WANG RY, XIAO JY, et al. Genotype distribution characteristics of HCV infection in voluntary blood donors in Ankang area[J]. Clin Res Pract, 2023, 8( 33): 6- 9. DOI: 10.19347/j.cnki.2096-1413.202333002.张博, 王儒意, 肖金玉, 等. 安康地区无偿献血人群HCV感染的基因型分布特征[J]. 临床医学研究与实践, 2023, 8( 33): 6- 9. DOI: 10.19347/j.cnki.2096-1413.202333002. [29] MU CY, ZHANG XM, FAN DS, et al. Analysis of HCV genotype distribution and natural drug resistance mutation in Huaibei city[J]. J Bengbu Med Coll, 2023, 48( 2): 260- 263. DOI: 10.13898/j.cnki.issn.1000-2200.2023.02.029.木朝宇, 张晓梅, 范德胜, 等. 淮北市HCV感染者基因亚型分布特征及1b型天然耐药突变分析[J]. 蚌埠医学院学报, 2023, 48( 2): 260- 263. DOI: 10.13898/j.cnki.issn.1000-2200.2023.02.029. [30] TANG Q, CHEN ZW, LI H, et al. Molecular epidemiology of hepatitis C virus genotypes in different geographical regions of Chinese mainland and a phylogenetic analysis[J]. Infect Dis Poverty, 2023, 12( 1): 66. DOI: 10.1186/s40249-023-01106-y. [31] WEN XY, TANG M, DENG ZH, et al. Distribution and clinical features of HCV genotypes in three areas in southwest China[J]. China J Mod Med, 2016, 26( 23): 42- 46. DOI: 10.3969/j.issn.1005-8982.2016.23.009.温先勇, 唐敏, 邓正华, 等. 中国西南三地HCV基因型的分布及临床特征[J]. 中国现代医学杂志, 2016, 26( 23): 42- 46. DOI: 10.3969/j.issn.1005-8982.2016.23.009. [32] TENG Y, XU ZC, ZHAO KT, et al. Novel function of SART1 in HNF4α transcriptional regulation contributes to its antiviral role during HBV infection[J]. J Hepatol, 2021, 75( 5): 1072- 1082. DOI: 10.1016/j.jhep.2021.06.038. [33] KANDA T, LAU GKK, WEI L, et al. APASL HCV guidelines of virus-eradicated patients by DAA on how to monitor HCC occurrence and HBV reactivation[J]. Hepatol Int, 2019, 13( 6): 649- 661. DOI: 10.1007/s12072-019-09988-7. -



 PDF下载 ( 784 KB)
PDF下载 ( 784 KB)

 下载:
下载: