特殊口腔异位定植菌与慢性肝病的关系
DOI: 10.12449/JCH260131
利益冲突声明:本文不存在任何利益冲突。
作者贡献声明:贺靖淋负责资料分析,撰写论文;卢晨霞负责拟定写作思路,修改论文;李晓东负责指导撰写文章并最后定稿。
-
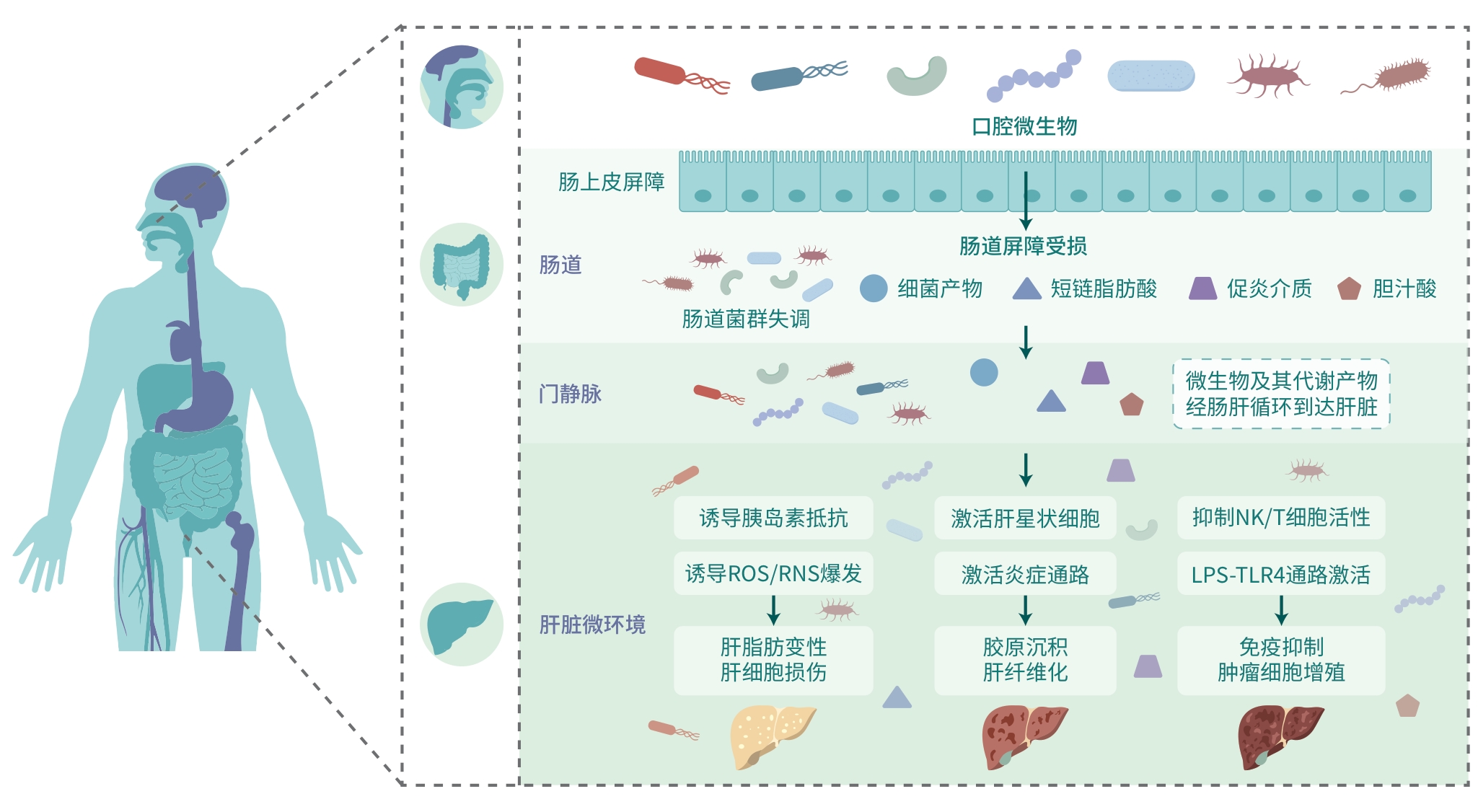
摘要: 慢性肝病是多种肝脏疾病的总称,其患病率呈逐年上升趋势。随着疾病进展,患者可出现多种严重并发症,甚至发展为肝衰竭。近年来,多项研究揭示了异位定植菌与慢性肝病的关系,探讨了异位定植菌在慢性肝病诊断及治疗等方面的潜在价值。本文系统综述了特殊异位定植菌与代谢相关脂肪性肝病、肝硬化和肝癌之间的关系,解析异位定植菌影响慢性肝病的相关机制,为利用异位定植菌对慢性肝病进行诊治提供参考。Abstract: Chronic liver disease is a general term for a variety of liver diseases, and its prevalence rate is increasing year by year. With the progression of the disease, patients may experience a variety of serious complications and even progress to liver failure. In recent years, a number of studies have revealed the association between ectopically colonized oral bacteria and chronic liver disease and explored their potential value in the diagnosis and treatment of chronic liver disease. This article systematically reviews the association of ectopically colonized oral bacteria with metabolic associated fatty liver disease, liver cirrhosis, and liver cancer and analyzes the mechanism for the influence of ectopically colonized oral bacteria on chronic liver disease, so as to provide a reference for the diagnosis and treatment of chronic liver disease using ectopically colonized oral bacteria.
-
[1] CZAJA AJ. Hepatic inflammation and progressive liver fibrosis in chronic liver disease[J]. World J Gastroenterol, 2014, 20( 10): 2515- 2532. DOI: 10.3748/wjg.v20.i10.2515. [2] MANIKAT R, AHMED A, KIM D. Current epidemiology of chronic liver disease[J]. Gastroenterol Rep, 2024, 12: goae069. DOI: 10.1093/gastro/goae069. [3] ATARASHI K, SUDA W, LUO CW, et al. Ectopic colonization of oral bacteria in the intestine drives TH1 cell induction and inflammation[J]. Science, 2017, 358( 6361): 359- 365. DOI: 10.1126/science.aan4526. [4] LI YQ, TANG WJ, ZHOU YJ. Role of intestinal microbiota and metabolites in the development, progression, and treatment of nonalcoholic fatty liver disease[J]. J Clin Hepatol, 2023, 39( 8): 1805- 1810. DOI: 10.3969/j.issn.1001-5256.2023.08.006.李永强, 唐文娟, 周永健. 肠道菌群及其代谢产物在非酒精性脂肪性肝病发生发展及治疗中的作用[J]. 临床肝胆病杂志, 2023, 39( 8): 1805- 1810. DOI: 10.3969/j.issn.1001-5256.2023.08.006. [5] XU SL, DENG KQ, LU CB, et al. Interleukin-6 classic and trans-signaling utilize glucose metabolism reprogramming to achieve anti- or pro-inflammatory effects[J]. Metabolism, 2024, 155: 155832. DOI: 10.1016/j.metabol.2024.155832. [6] ACHARYA C, SAHINGUR SE, BAJAJ JS. Microbiota, cirrhosis, and the emerging oral-gut-liver axis[J]. JCI Insight, 2017, 2( 19): e94416. DOI: 10.1172/jci.insight.94416. [7] ZHOU JH, ZHOU F, WANG WX, et al. Epidemiological features of NAFLD from 1999 to 2018 in China[J]. Hepatology, 2020, 71( 5): 1851- 1864. DOI: 10.1002/hep.31150. [8] Chinese Society of Hepatology, Chinese Medical Association. Guidelines for the prevention and treatment of metabolic dysfunction-associated(non-alcoholic)fatty liver disease(Version 2024)[J]. J Pract Hepatol, 2024, 27( 4): 494- 510. DOI: 10.3760/cma.j.cn501113-20240327-00163.中华医学会肝病学分会. 代谢相关(非酒精性)脂肪性肝病防治指南(2024年版)[J]. 实用肝脏病杂志, 2024, 27( 4): 494- 510. DOI: 10.3760/cma.j.cn501113-20240327-00163. [9] YANG B, ZHANG R. Progress on the treatment of metabolic associated fatty liver disease[J/CD]. Chin J Liver Dis: Electronic Edition, 2024, 16( 4): 25- 30. DOI: 10.3969/j.issn.1674-7380.2024.04.004.杨彬, 张瑞. 代谢相关脂肪性肝病治疗进展[J/CD]. 中国肝脏病杂志(电子版), 2024, 16( 4): 25- 30. DOI: 10.3969/j.issn.1674-7380.2024.04.004. [10] BUZZETTI E, PINZANI M, TSOCHATZIS EA. The multiple-hit pathogenesis of non-alcoholic fatty liver disease(NAFLD)[J]. Metabolism, 2016, 65( 8): 1038- 1048. DOI: 10.1016/j.metabol.2015.12.012. [11] LIU LB, GENG Y, XIONG CL. Impact of Porphyromonas gingivalis-odontogenic-odontogenic infection on the pathogenesis of non-alcoholic fatty liver disease[J]. Ann Med, 2023, 55( 2): 2255825. DOI: 10.1080/07853890.2023.2255825. [12] WANG T, ISHIKAWA T, SASAKI M, et al. Oral and gut microbial dysbiosis and non-alcoholic fatty liver disease: The central role of Porphyromonas gingivalis[J]. Front Med, 2022, 9: 822190. DOI: 10.3389/fmed.2022.822190. [13] BLASCO-BAQUE V, GARIDOU L, POMIÉ C, et al. Periodontitis induced by Porphyromonas gingivalis drives periodontal microbiota dysbiosis and insulin resistance via an impaired adaptive immune response[J]. Gut, 2017, 66( 5): 872- 885. DOI: 10.1136/gutjnl-2015-309897. [14] SASAKI N, KATAGIRI S, KOMAZAKI R, et al. Endotoxemia by Porphyromonas gingivalis injection aggravates non-alcoholic fatty liver disease, disrupts glucose/lipid metabolism, and alters gut microbiota in mice[J]. Front Microbiol, 2018, 9: 2470. DOI: 10.3389/fmicb.2018.02470. [15] NAKAJIMA M, ARIMATSU K, KATO T, et al. Oral administration of P. gingivalis induces dysbiosis of gut microbiota and impaired barrier function leading to dissemination of enterobacteria to the liver[J]. PLoS One, 2015, 10( 7): e0134234. DOI: 10.1371/journal.pone.0134234. [16] FURUSHO H, MIYAUCHI M, HYOGO H, et al. Dental infection of Porphyromonas gingivalis exacerbates high fat diet-induced steatohepatitis in mice[J]. J Gastroenterol, 2013, 48( 11): 1259- 1270. DOI: 10.1007/s00535-012-0738-1. [17] YONEDA M, NAKA S, NAKANO K, et al. Involvement of a periodontal pathogen, Porphyromonas gingivalis on the pathogenesis of non-alcoholic fatty liver disease[J]. BMC Gastroenterol, 2012, 12: 16. DOI: 10.1186/1471-230X-12-16. [18] NAKAHARA T, HYOGO H, ONO A, et al. Involvement of Porphyromonas gingivalis in the progression of non-alcoholic fatty liver disease[J]. J Gastroenterol, 2018, 53( 2): 269- 280. DOI: 10.1007/s00535-017-1368-4. [19] RAJA M, UMMER F, DHIVAKAR CP. Aggregatibacter actinomycetemcomitans-A tooth killer?[J]. J Clin Diagn Res, 2014, 8( 8): ZE13- 6. DOI: 10.7860/JCDR/2014/9845.4766. [20] CASTRILLON CA, HINCAPIE JP, YEPES FL, et al. Occurrence of red complex microorganisms and Aggregatibacter actinomycetemcomitans in patients with diabetes[J]. J Investig Clin Dent, 2015, 6( 1): 25- 31. DOI: 10.1111/jicd.12051. [21] KOMAZAKI R, KATAGIRI S, TAKAHASHI H, et al. Periodontal pathogenic bacteria, Aggregatibacter actinomycetemcomitans affect non-alcoholic fatty liver disease by altering gut microbiota and glucose metabolism[J]. Sci Rep, 2017, 7( 1): 13950. DOI: 10.1038/s41598-017-14260-9. [22] TUOMAINEN AM, JAUHIAINEN M, KOVANEN PT, et al. Aggregatibacter actinomycetemcomitans induces MMP-9 expression and proatherogenic lipoprotein profile in apoE-deficient mice[J]. Microb Pathog, 2008, 44( 2): 111- 117. DOI: 10.1016/j.micpath.2007.08.011. [23] HUANG DQ, TERRAULT NA, TACKE F, et al. Global epidemiology of cirrhosis: Aetiology, trends and predictions[J]. Nat Rev Gastroenterol Hepatol, 2023, 20( 6): 388- 398. DOI: 10.1038/s41575-023-00759-2. [24] SCAGLIONE S, KLIETHERMES S, CAO GC, et al. The epidemiology of cirrhosis in the United States: A population-based study[J]. J Clin Gastroenterol, 2015, 49( 8): 690- 696. DOI: 10.1097/MCG.0000-00000000-0208. [25] GBD 2017 Cirrhosis Collaborators. The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017[J]. Lancet Gastroenterol Hepatol, 2020, 5( 3): 245- 266. DOI: 10.1016/S2468-1253(19)30349-8. [26] MOHAMMED H, VARONI EM, COCHIS A, et al. Oral dysbiosis in pancreatic cancer and liver cirrhosis: A review of the literature[J]. Biomedicines, 2018, 6( 4): 115. DOI: 10.3390/biomedicines6040-115. [27] QIN N, YANG FL, LI A, et al. Alterations of the human gut microbiome in liver cirrhosis[J]. Nature, 2014, 513( 7516): 59- 64. DOI: 10.1038/nature13568. [28] GIACOMINI JJ, TORRES-MORALES J, DEWHIRST FE, et al. Site specialization of human oral Veillonella Species[J]. Microbiol Spectr, 2023, 11( 1): e04042-22. DOI: 10.1128/spectrum.04042-22. [29] CHEN YF, JI F, GUO J, et al. Dysbiosis of small intestinal microbiota in liver cirrhosis and its association with etiology[J]. Sci Rep, 2016, 6: 34055. DOI: 10.1038/srep34055. [30] PARADA VENEGAS D, de la FUENTE MK, LANDSKRON G, et al. Short chain fatty acids(SCFAs)-Mediated gut epithelial and immune regulation and its relevance for inflammatory bowel diseases[J]. Front Immunol, 2019, 10: 277. DOI: 10.3389/fimmu.2019.00277. [31] HUA XL, FENG H. Changes in intestinal microbiota of HBV-associated liver cirrhosis with/without hepatic encephalopathy[J]. Medicine, 2022, 101( 33): e29935. DOI: 10.1097/MD.00000000000-29935. [32] BAJAJ JS, RIDLON JM, HYLEMON PB, et al. Linkage of gut microbiome with cognition in hepatic encephalopathy[J]. Am J Physiol Gastrointest Liver Physiol, 2012, 302( 1): G168- G175. DOI: 10.1152/ajpgi.00190.2011. [33] DONG LM, YAO KH. Advances in the classification and biological properties of streptococcal superantigens[J]. Chin J Appl Clin Pediatr, 2022, 37( 21): 1674- 1677. DOI: 10.3760/cma.j.cn101070-202-20524-00601.董立民, 姚开虎. 链球菌超抗原分类及其生物学作用研究进展[J]. 中华实用儿科临床杂志, 2022, 37( 21): 1674- 1677. DOI: 10.3760/cma.j.cn101070-20220524-00601. [34] ZHONG XD, CUI P, JIANG JJ, et al. Streptococcus, the predominant bacterium to predict the severity of liver injury in alcoholic liver disease[J]. Front Cell Infect Microbiol, 2021, 11: 649060. DOI: 10.3389/fcimb.2021.649060. [35] CHEN YF, YANG FL, LU HF, et al. Characterization of fecal microbial communities in patients with liver cirrhosis[J]. Hepatology, 2011, 54( 2): 562- 572. DOI: 10.1002/hep.24423. [36] BAJAJ JS, MATIN P, WHITE MB, et al. Periodontal therapy favorably modulates the oral-gut-hepatic axis in cirrhosis[J]. Am J Physiol Gastrointest Liver Physiol, 2018, 315( 5): G824- G837. DOI: 10.1152/ajpgi.00230.2018. [37] BAJAJ JS, BETRAPALLY NS, HYLEMON PB, et al. Salivary microbiota reflects changes in gut microbiota in cirrhosis with hepatic encephalopathy[J]. Hepatology, 2015, 62( 4): 1260- 1271. DOI: 10.1002/hep.27819. [38] ZHENG RS, CHEN R, HAN BF, et al. Cancer incidence and mortality in China, 2022[J]. Chin J Oncol, 2024, 46( 3): 221- 231. DOI: 10.3760/cma.j.cn112152-20240119-00035.郑荣寿, 陈茹, 韩冰峰, 等. 2022年中国恶性肿瘤流行情况分析[J]. 中华肿瘤杂志, 2024, 46( 3): 221- 231. DOI: 10.3760/cma.j.cn112152-20240119-00035. [39] SCHWABE RF, GRETEN TF. Gut microbiome in HCC- Mechanisms, diagnosis and therapy[J]. J Hepatol, 2020, 72( 2): 230- 238. DOI: 10.1016/j.jhep.2019.08.016. [40] ZHOU Q, CAI CL, LI JQ. Gut-liver axis: Intestinal microbial homeostasis and hepatocellular carcinoma[J]. J Clin Hepatol, 2023, 39( 11): 2710- 2717. DOI: 10.3969/j.issn.1001-5256.2023.11.029.周荃, 蔡春琳, 李金强. 肠-肝轴: 肠道微生物稳态与肝细胞癌[J]. 临床肝胆病杂志, 2023, 39( 11): 2710- 2717. DOI: 10.3969/j.issn.1001-5256.2023.11.029. [41] LI XK, LUO SM, JIANG YF, et al. Enhancing fibroblast-epithelial cell communications: Serpine2 as a key molecule in Fusobacterium nucleatum-promoted-promoted colon cancer[J]. Front Immunol, 2025, 16: 1563922. DOI: 10.3389/fimmu.2025.1563922. [42] DHARMANI P, STRAUSS J, AMBROSE C, et al. Fusobacterium nucleatum infection of colonic cells stimulates MUC2 mucin and tumor necrosis factor alpha[J]. Infect Immun, 2011, 79( 7): 2597- 2607. DOI: 10.1128/IAI.05118-11. [43] DARNAUD M, FAIVRE J, MONIAUX N. Targeting gut flora to prevent progression of hepatocellular carcinoma[J]. J Hepatol, 2013, 58( 2): 385- 387. DOI: 10.1016/j.jhep.2012.08.019. [44] DAPITO DH, MENCIN A, GWAK GY, et al. Promotion of hepatocellular carcinoma by the intestinal microbiota and TLR4[J]. Cancer Cell, 2012, 21( 4): 504- 516. DOI: 10.1016/j.ccr.2012.02.007. [45] HUYNH T, KAPUR RV, KAPLAN CW, et al. The role of aggregation in Fusobacterium nucleatum- induced immune cell death[J]. J Endod, 2011, 37( 11): 1531- 1535. DOI: 10.1016/j.joen.2011.06.034. [46] LU HF, REN ZG, LI A, et al. Deep sequencing reveals microbiota dysbiosis of tongue coat in patients with liver carcinoma[J]. Sci Rep, 2016, 6: 33142. DOI: 10.1038/srep33142. [47] ZHANG WZ, XU XS, CAI LP, et al. Dysbiosis of the gut microbiome in elderly patients with hepatocellular carcinoma[J]. Sci Rep, 2023, 13( 1): 7797. DOI: 10.1038/s41598-023-34765-w. [48] ZHENG RP, WANG GQ, PANG ZQ, et al. Liver cirrhosis contributes to the disorder of gut microbiota in patients with hepatocellular carcinoma[J]. Cancer Med, 2020, 9( 12): 4232- 4250. DOI: 10.1002/cam4.3045. [49] HE YT, ZHANG QY, YU X, et al. Overview of microbial profiles in human hepatocellular carcinoma and adjacent nontumor tissues[J]. J Transl Med, 2023, 21( 1): 68. DOI: 10.1186/s12967-023-03938-6. -



 PDF下载 ( 876 KB)
PDF下载 ( 876 KB)

 下载:
下载:


