外周血淋巴细胞计数在慢加急性肝衰竭短期预后评估中的价值
DOI: 10.3969/j.issn.1001-5256.2023.10.016
Value of peripheral blood lymphocyte count in evaluating the short-term prognosis of patients with acute-on-chronic liver failure
-
摘要:
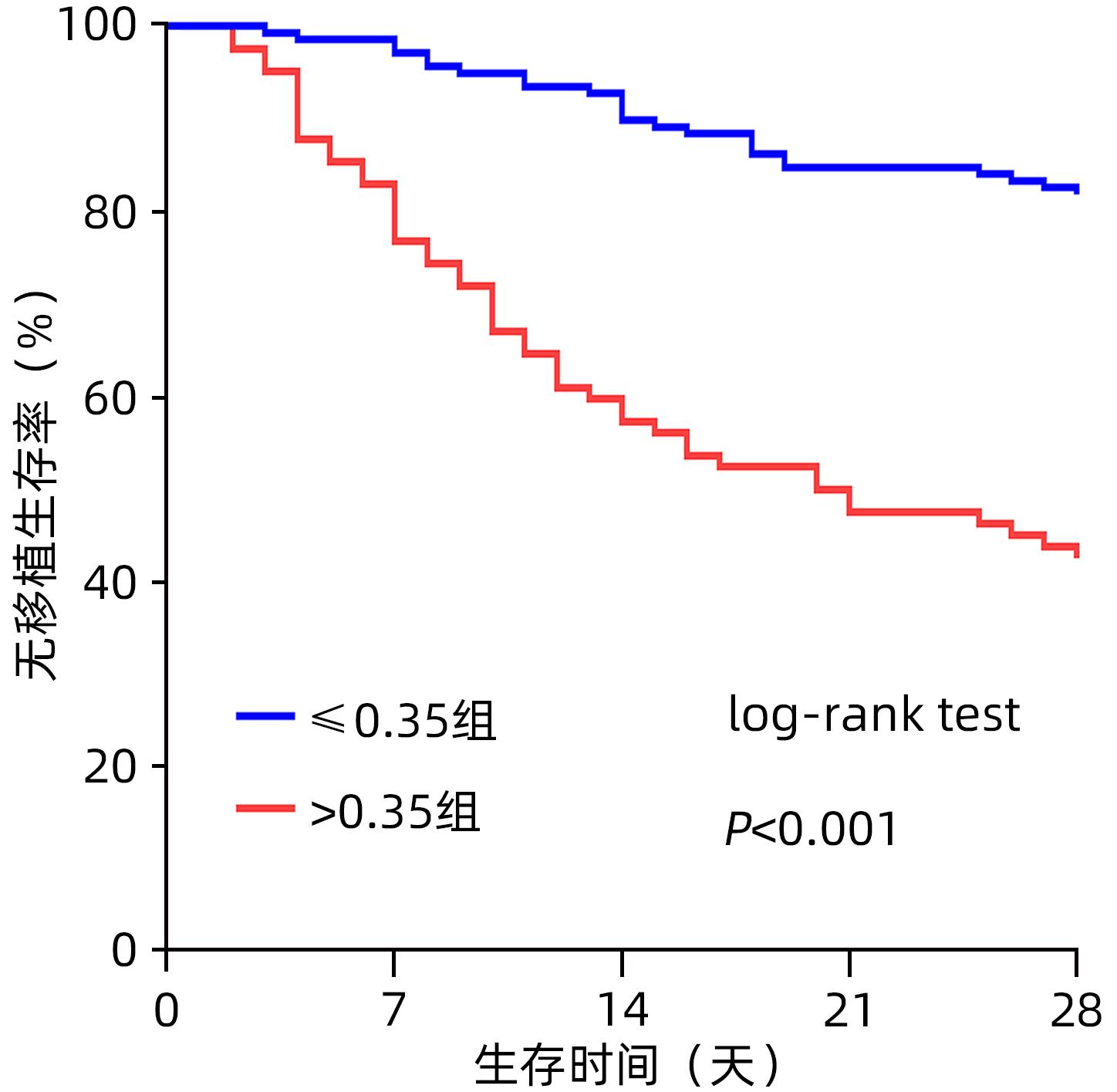
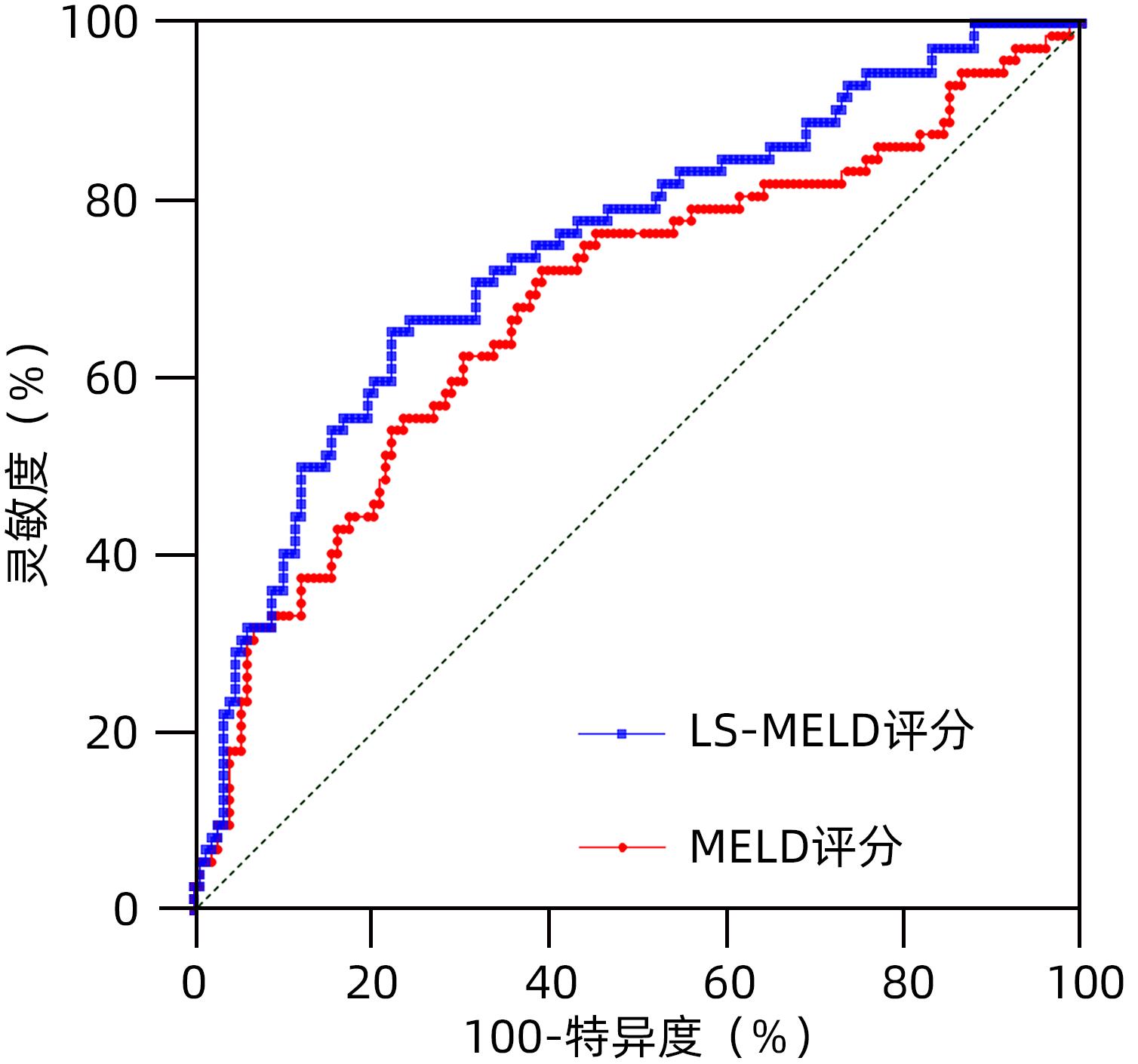
目的 探讨慢加急性肝衰竭(ACLF)患者预后影响因素,建立短期预后模型。 方法 回顾2011年1月—2016年12月在西安交通大学第一附属医院感染科住院的247例ACLF患者的基线临床资料。将患者分为生存组及死亡组,比较组间差异,分析预后影响因素,同时建立预后模型,应用受试者工作特征曲线(ROC曲线)评估预测效能并确定最佳截断值。正态分布的计量资料两组间比较采用成组t检验;不服从正态分布的资料两组间比较采用Mann-Whitney U秩和检验;计数资料两组间比较采用Fisher精确检验或Pearson卡方检验。Logistic单因素及多因素分析28天、90天预后相关的独立危险因素。使用Kaplan-Meier方法绘制28天生存曲线。 结果 经纳入及排除标准筛选后共纳入ACLF患者220例,28天生存组148例、死亡组72例,28天无移植生存率67.27%;90天生存组115例、死亡组105例,90天无移植生存率52.27%。Logistic回归分析结果显示女性(OR=2.149,P=0.030)、高MELD评分(OR=1.120,P<0.001)、外周血低淋巴细胞计数(OR=0.411,P=0.002)是影响28天预后的独立危险因素;据此建立影响28天预后的LS-MELD模型:-3.432+0.765×性别-0.890×淋巴细胞计数×10-9+0.113×MELD(性别赋值:男性为1,女性为2)。经ROC曲线确定模型的最佳截断值为0.35,据此将患者分为低LS-MELD组(≤0.35)及高LS-MELD组(>0.35),低LS-MELD组的28天生存率显著高于高LS-MELD组(P<0.001)。 结论 外周血淋巴细胞计数及性别联合MELD评分对ALCF患者的短期预后具有预测价值。 Abstract:Objective To investigate the influencing factors for the prognosis of patients with acute-on-chronic liver failure (ACLF), and to establish a short-term prognostic model. Methods A retrospective analysis was performed for the baseline clinical data of 247 patients with ACLF who were hospitalized in Department of Infectious Diseases, The First Affiliated Hospital of Xi’an Jiaotong University, from January 2011 to December 2016, and the patients were divided into survival group and death group. The two groups were compared to identify the influencing factors for prognosis; a prognostic model was established, and the receiver operating characteristic (ROC) curve was used to assess its predictive efficacy and determine the optimal cut-off value. The independent-samples t test was used for comparison of normally distributed continuous data between groups, and the Mann-Whitney U rank sum test was used for comparison of non-normally distributed continuous data between groups; the Fisher’s exact test or the Pearson’s chi-square test was used for comparison of categorical data between groups. The univariate and multivariate logistic regression analyses were used to investigate the independent risk factors for 28- and 90-day prognosis, and the Kaplan-Meier method was used to plot the 28-day survival curves. Results A total of 220 patients with ACLF were included based on the inclusion and exclusion criteria; there were 148 patients in the 28-day survival group and 72 patients in the 28-day death group, with a 28-day transplantation-free survival rate of 67.27%; there were 115 patients in the 90-day survival group and 105 patients in the 90-day death group, with a 90-day transplantation-free survival rate of 52.27%. The logistic regression analysis showed that female sex (odds ratio [OR]=2.149, P=0.030), high Model for End-Stage Liver Disease (MELD) score (OR=1.120, P<0.001), and low lymphocyte count (OR=0.411, P=0.002) were independent risk factors for 28-day prognosis, and an LS-MELD model for 28-day prognosis was established as Logit (28-day prognosis)=-3.432+0.765×sex-0.890×lymphocyte count×10-9+0.113×MELD(1 for male sex and 2 for female sex). The ROC curve analysis showed that this model had an optimal cut-off value of 0.35, and then the patients were divided into low LS-MELD group (≤0.35) and high LS-MELD group (>0.35); the low LS-MELD group had a significantly higher 28-day survival rate than the high LS-MELD group (P<0.001). Conclusion Peripheral blood lymphocyte count combined with sex and MELD score has a certain value in predicting the short-term prognosis of ALCF patients. -
Key words:
- Acute-On-Chronic Liver Failure /
- Risk Factors /
- Lymphocyte Count /
- Prognosis
-
表 1 220例ACLF患者基线一般资料及实验室指标
Table 1. Baseline general data and laboratory indicators of 220 patients with ACLF
指标 数值 年龄(岁) 45.00(37.00~56.75) 性别(男/女,例) 163/57 腹水(有/无,例) 127/93 肝性脑病(有/无,例) 84/136 消化道出血(有/无,例) 12/208 肝肾综合征(有/无,例) 27/193 感染(有/无,例) 151/69 高血压(有/无,例) 11/209 糖尿病(有/无,例) 14/206 病因(HBV/HEV/酒精/药物/免疫/其他,例) 156/4/3/11/1/45 ALT(U/L) 279.13(90.58~687.53) AST(U/L) 241.00(107.24~293.75) TBil(μmol/L) 304.95(202.30~410.45) Alb(g/L) 30.6±4.9 Glo(g/L) 29.65(24.34~36.70) BUN(mmol/L) 4.19(2.92~6.20) 肌酐(μmol/L) 62.0(50.1~78.7) INR 2.23(1.80~2.95) FIB(g/L) 1.21(0.96~1.68) Hb(g/L) 124(102~141) PLT(×109/L) 90.0(55.0~132.5) WBC(×109/L) 6.52(4.76~8.68) 淋巴细胞计数(×109/L) 1.11(0.78~1.54) 淋巴细胞百分比 15.52(8.78~24.28) 中性粒细胞计数(×109/L) 5.30(3.46~8.24) 中性粒细胞百分比 70.50(61.65~79.28) MELD评分 22.89(18.99~27.44) 表 2 28天、90天生存组及死亡组临床资料与实验室指标对比
Table 2. Comparison of clinical data and laboratory indexes between 28-day, 90-day survival group and death group
指标 28天生存组 (n=148) 28天死亡组 (n=72) 统计值 P值 90天生存组 (n=115) 90天死亡组 (n=105) 统计值 P值 年龄(岁) 45.0(35.0~45.0) 44.5(38.0~60.0) Z=-1.085 0.278 45.0(34.0~55.0) 46.0(39.5~60.0) Z=-1.961 0.050 性别(男/女,例) 116/32 47/25 χ2=4.330 0.037 93/22 70/35 χ2=5.768 0.016 腹水(有/无,例) 85/63 42/30 χ2=0.016 0.899 65/50 62/43 χ2=0.143 0.705 肝性脑病(有/无,例) 39/109 45/27 χ2=26.815 <0.001 25/90 59/46 χ2=27.600 <0.001 消化道出血(有/无,例) 5/143 7/65 χ2=2.650 0.104 3/112 9/96 χ2=3.784 0.052 肝肾综合征(有/无,例) 14/134 13/59 χ2=3.324 0.068 5/110 22/83 χ2=14.055 <0.001 感染(有/无,例) 94/54 57/15 χ2=5.513 0.019 75/40 76/29 χ2=1.308 0.253 高血压(有/无,例) 5/143 6/66 χ2=1.569 0.210 3/112 8/97 χ2=2.901 0.089 糖尿病(有/无,例) 7/141 7/65 χ2=1.275 0.259 6/109 8/97 χ2=0.531 0.466 ALT(U/L) 281.69(99.91~648.05) 277.00(76.60~725.89) Z=-0.564 0.573 282.37(134.00~700.11) 275.00(74.64~645.10) Z=-1.071 0.284 AST(U/L) 244.50(109.58~525.15) 214.45(93.33~701.00) Z=-0.131 0.896 260.00(115.00~534.80) 202.00(94.51~630.50) Z=-0.868 0.385 TBil(μmol/L) 284.70(199.10~368.78) 366.83(208.28~426.21) Z=-2.067 0.039 262.40(193.00~341.14) 367.50(225.04~431.30) Z=-3.856 <0.001 Alb(g/L) 30.50±0.42 30.47±0.58 t=0.036 0.971 30.51±5.22 30.38±4.68 t=0.323 0.747 Glo(g/L) 30.30(24.68~37.18) 29.30(23.20~34.23) Z=-1.367 0.172 31.10(25.80~37.64) 28.60(23.05~34.16) Z=-2.292 0.022 BUN(mmol/L) 4.11(3.04~5.54) 4.60(2.83~8.10) Z=-1.346 0.178 3.98(2.86~5.14) 4.46(2.98~7.94) Z=-2.214 0.027 肌酐(μmol/L) 61.60(50.16~76.00) 62.00(49.35~86.85) Z=-0.516 0.606 61.30(50.64~76.29) 62.00(48.60~81.60) Z=-0.288 0.773 INR 2.01(1.71~2.63) 2.85(2.23~4.21) Z=-5.504 <0.001 1.97(1.71~2.42) 2.67(1.95~3.89) Z=-4.716 <0.001 FIB(g/L) 1.32(0.99~1.73) 1.11(0.84~1.48) Z=-2.779 0.005 1.29(1.00~1.68) 1.16(0.90~1.68) Z=-1.663 0.096 Hb(g/L) 126.00(109.00~141.75) 119.50(97.25~138.00) Z=-1.670 0.095 126.00±23.66 118.05±26.42 t=2.281 0.024 PLT(×109/L) 90.50(59.25~133.50) 87.50(50.25~132.50) Z=-0.742 0.458 98.00(60.00~153.00) 80.00(51.00~125.00) Z=-1.795 0.073 WBC(×109/L) 6.48(4.58~8.68) 6.68(5.07~8.68) Z=-0.445 0.657 6.21(4.49~8.35) 6.80(5.19~9.14) Z=-1.674 0.094 淋巴细胞计数(×109/L) 1.18(0.89~1.59) 0.89(0.60~1.39) Z=-3.208 0.001 1.18(0.89~1.59) 1.00(0.65~1.47) Z=-2.559 0.011 淋巴细胞百分比(%) 18.10(10.26~25.43) 11.20(6.59~20.90) Z=-2.982 0.003 18.34(9.63~27.50) 13.40(7.57~22.05) Z=-2.218 0.027 中性粒细胞计数(×109/L) 4.99(3.32~7.63) 5.66(3.96~9.58) Z=-1.219 0.223 4.54(3.22~7.58) 5.59(3.92~8.87) Z=-1.124 0.261 中性粒细胞百分比(%) 68.22(59.83~78.21) 73.47(66.33~81.69) Z=-2.806 0.005 67.00(58.10~77.00) 73.70(65.60~87.92) Z=-3.734 <0.001 MELD评分 21.80(18.54~25.60) 26.20(22.16~32.91) Z=-4.422 <0.001 21.31(17.96~25.19) 24.96(21.30~31.65) Z=-4.410 <0.001 表 3 影响ACLF患者28天生存的单因素及多因素分析
Table 3. Univariate and multivariate analysis of 28-day prognosis in ACLF patients
指标 单因素分析 多因素分析 OR(95%CI) P值 OR(95%CI) P值 年龄(岁) 1.015(0.995~1.036) 0.137 性别 1.928(1.034~3.596) 0.039 2.149(1.076~4.292) 0.030 感染 3.080(0.942~10.069) 0.063 肝肾综合征 2.109(0.934~4.763) 0.073 Hb(g/L) 0.989(0.978~1.000) 0.059 PLT(×109/L) 0.998(0.993~1.002) 0.340 淋巴细胞计数(×109/L) 0.444(0.254~0.776) 0.004 0.411(0.231~0.730) 0.002 中性粒细胞百分比(%) 1.035(1.010~1.060) 0.005 FIB(g/L) 0.561(0.324~0.971) 0.039 MELD评分 1.107(1.058~1.159) <0.001 1.120(1.066~1.176) <0.001 -
[1] Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, Chinese Medical Association; Severe Liver Disease and Artificial Liver Group, Chinese Society of Hepatology, Chinese Medical Association. Guideline for diagnosis and treatment of liver failure(2018)[J]. J Clin Hepatol, 2019, 35( 1): 38- 44. DOI: 10.3969/j.issn.1001-5256.2019.01.007.中华医学会感染病学分会肝衰竭与人工肝学组, 中华医学会肝病学分会重型肝病与人工肝学组. 肝衰竭诊治指南(2018年版)[J]. 临床肝胆病杂志, 2019, 35( 1): 38- 44. DOI: 10.3969/j.issn.1001-5256.2019.01.007. [2] ARROYO V, ANGELI P, MOREAU R, et al. The systemic inflammation hypothesis: Towards a new paradigm of acute decompensation and multiorgan failure in cirrhosis[J]. J Hepatol, 2021, 74( 3): 670- 685. DOI: 10.1016/j.jhep.2020.11.048. [3] LI J, LIANG X, JIANG J, et al. PBMC transcriptomics identifies immune-metabolism disorder during the development of HBV-ACLF[J]. Gut, 2022, 71( 1): 163- 175. DOI: 10.1136/gutjnl-2020-323395. [4] WIESNER R, EDWARDS E, FREEMAN R, et al. Model for end-stage liver disease(MELD) and allocation of donor livers[J]. Gastroenterology, 2003, 124( 1): 91- 96. DOI: 10.1053/gast.2003.50016. [5] LI JQ, LIANG X, YOU SL, et al. Development and validation of a new prognostic score for hepatitis B virus-related acute-on-chronic liver failure[J]. J Hepatol, 2021, 75( 5): 1104- 1115. DOI: 10.1016/j.jhep.2021.05.026. [6] CAI JJ, WANG K, HAN T, et al. Evaluation of prognostic values of inflammation-based makers in patients with HBV-related acute-on-chronic liver failure[J]. Medicine, 2018, 97( 46): e13324. DOI: 10.1097/MD.0000000000013324. [7] GAO FY, SUN L, YE XQ, et al. Development and validation of a prognostic model for acute-on-chronic hepatitis B liver failure[J]. Eur J Gastroenterol Hepatol, 2017, 29( 6): 669- 678. DOI: 10.1097/MEG.0000000000000854. [8] LEI Q, AO KJ, ZHANG YH, et al. Prognostic factors of the short-term outcomes of patients with hepatitis B virus-associated acute-on-chronic liver failure[J]. Clinics, 2017, 72( 11): 686- 692. DOI: 10.6061/clinics/2017(11)07. [9] GAO X, ZHAO CJ, HU SH. Short-term prognostic value of age-bilirubin-international normalized ratio-creatinine score in patients with hepatitis B virus-related acute-on-chronic liver failure[J/CD]. Chin J Exp Clin Infect Dis(Electronic Edition), 2022, 16( 2): 108- 114. DOI: 10.3877/cma.j.issn.1674-1358.2022.02.005.高祥, 赵成军, 胡世宏. 年龄-胆红素-国际标准化比率-肌酐评分对乙型肝炎相关慢加急性肝功能衰竭患者短期预后的评估价值[J/CD]. 中华实验和临床感染病杂志(电子版), 2022, 16( 2): 108- 114. DOI: 10.3877/cma.j.issn.1674-1358.2022.02.005. [10] TRIANTAFYLLOU E, WOOLLARD KJ, MCPHAIL MJW, et al. The role of monocytes and macrophages in acute and acute-on-chronic liver failure[J]. Front Immunol, 2018, 9: 2948. DOI: 10.3389/fimmu.2018.02948. [11] ZHANG DJ, ZHOU B, HOU JL. Research progress in prognostic models of acute-on-chronic liver failure[J]. J Clin Hepatol, 2018, 34( 6): 1351- 1356. DOI: 10.3969/j.issn.1001-5256.2018.06.047.张东敬, 周彬, 侯金林. 慢加急性肝衰竭预后模型的研究进展[J]. 临床肝胆病杂志, 2018, 34( 6): 1351- 1356. DOI: 10.3969/j.issn.1001-5256.2018.06.047. [12] CHEN W, YOU J, CHEN J, et al. Modified model for end-stage liver disease improves short-term prognosis of hepatitis B virus-related acute-on-chronic liver failure[J]. World J Gastroenterol, 2017, 23( 40): 7303- 7309. DOI: 10.3748/wjg.v23.i40.7303. [13] MONSANTO P, ALMEIDA N, LRIAS C, et al. Evaluation of MELD score and Maddrey discriminant function for mortality prediction in patients with alcoholic hepatitis[J]. Hepato-gastroenterology, 2013, 60( 125): 1089- 1094. DOI: 10.5754/hge11969. [14] DURAND F, VALLA D. Assessment of the prognosis of cirrhosis: Child-Pugh versus MELD[J]. J Hepatol, 2005, 42 Suppl(1): S100-S 107. DOI: 10.1016/j.jhep.2004.11.015. [15] ARABI YM, DARA SI, MEMISH Z, et al. Antimicrobial therapeutic determinants of outcomes from septic shock among patients with cirrhosis[J]. Hepatology, 2012, 56( 6): 2305- 2315. DOI: 10.1002/hep.25931. [16] RUBIN JB, HAMEED B, GOTTFRIED M, et al. Acetaminophen-induced acute liver failure is more common and more severe in women[J]. Clin Gastroenterol Hepatol, 2018, 16( 6): 936- 946. DOI: 10.1016/j.cgh.2017.11.042. [17] NEPHEW LD, ZIA Z, GHABRIL M, et al. Sex disparities in waitlisting and liver transplant for acute liver failure[J]. JHEP Rep, 2020, 3( 1): 100200. DOI: 10.1016/j.jhepr.2020.100200. [18] WLODZIMIROW KA, ESLAMI S, ABU-HANNA A, et al. A systematic review on prognostic indicators of acute on chronic liver failure and their predictive value for mortality[J]. Liver Int, 2013, 33( 1): 40- 52. DOI: 10.1111/j.1478-3231.2012.02790.x. [19] HAN CJ, JIN X, WU ZX, et al. Predicting the prognosis of patients with HBV-related acute liver failure by combining the ratio of neutrophils to lymphocytes and the ratio of C-reactive protein to albumin[J]. Chin J Clin Lab Sci, 2022, 40( 4): 281- 285. DOI: 10.13602/j.cnki.jcls.2022.04.10.韩才均, 金星, 吴政燮, 等. 联合中性粒细胞与淋巴细胞比值和C反应蛋白与清蛋白比值预测HBV相关慢加急性肝衰竭患者预后[J]. 临床检验杂志, 2022, 40( 4): 281- 285. DOI: 10.13602/j.cnki.jcls.2022.04.10. [20] QIANG L, QIN J, SUN CF, et al. Prognostic evaluation of a prediction model based on neutrophil/lymphocyte ratio and red blood cell distribution width of inflammatory factors on hepatitis B virus-related acute-on-chronic liver failure[J]. J Chongqing Med Univ, 2021, 46( 3): 317- 324. DOI: 10.13406/j.cnki.cyxb.002486.强丽, 秦娇, 孙长峰, 等. 基于炎症因子中性粒/淋巴细胞比值与红细胞分布宽度的预测模型对乙肝相关慢加急性肝衰竭的预后评估[J]. 重庆医科大学学报, 2021, 46( 3): 317- 324. DOI: 10.13406/j.cnki.cyxb.002486. [21] CHEN LL, LI Q. Short-term prognostic value of peripheral blood NLR, PCT and MELD score in patients with acute-on-chronic(subacute) liver failure[J]. J Tianjin Med Univ, 2017, 23( 2): 151- 154.陈岭岭, 李谦. 外周血NLR、PCT及MELD评分对慢加急(亚急)性肝衰竭近期预后的预测价值[J]. 天津医科大学学报, 2017, 23( 2): 151- 154. [22] LEITHEAD JA, RAJORIYA N, GUNSON BK, et al. Neutrophil-to-lymphocyte ratio predicts mortality in patients listed for liver transplantation[J]. Liver Int, 2015, 35( 2): 502- 509. DOI: 10.1111/liv.12688. -



 PDF下载 ( 746 KB)
PDF下载 ( 746 KB)

 下载:
下载: