失代偿期肝硬化合并多原发癌1例报告
DOI: 10.12449/JCH240923
伦理学声明:本例报告已获得患者及家属知情同意。
利益冲突声明:本文不存在任何利益冲突。
作者贡献声明:晁文婷、黄睿起草或修改文章关键内容,研究数据的获取分析解释过程;黄睿对文章的知识性内容作批评性审阅,获取研究经费,提供行政、技术或材料支持,指导撰写文章并最终定稿。
Diagnosis and treatment of decompensated cirrhosis with multiple primary cancers: A case report
-
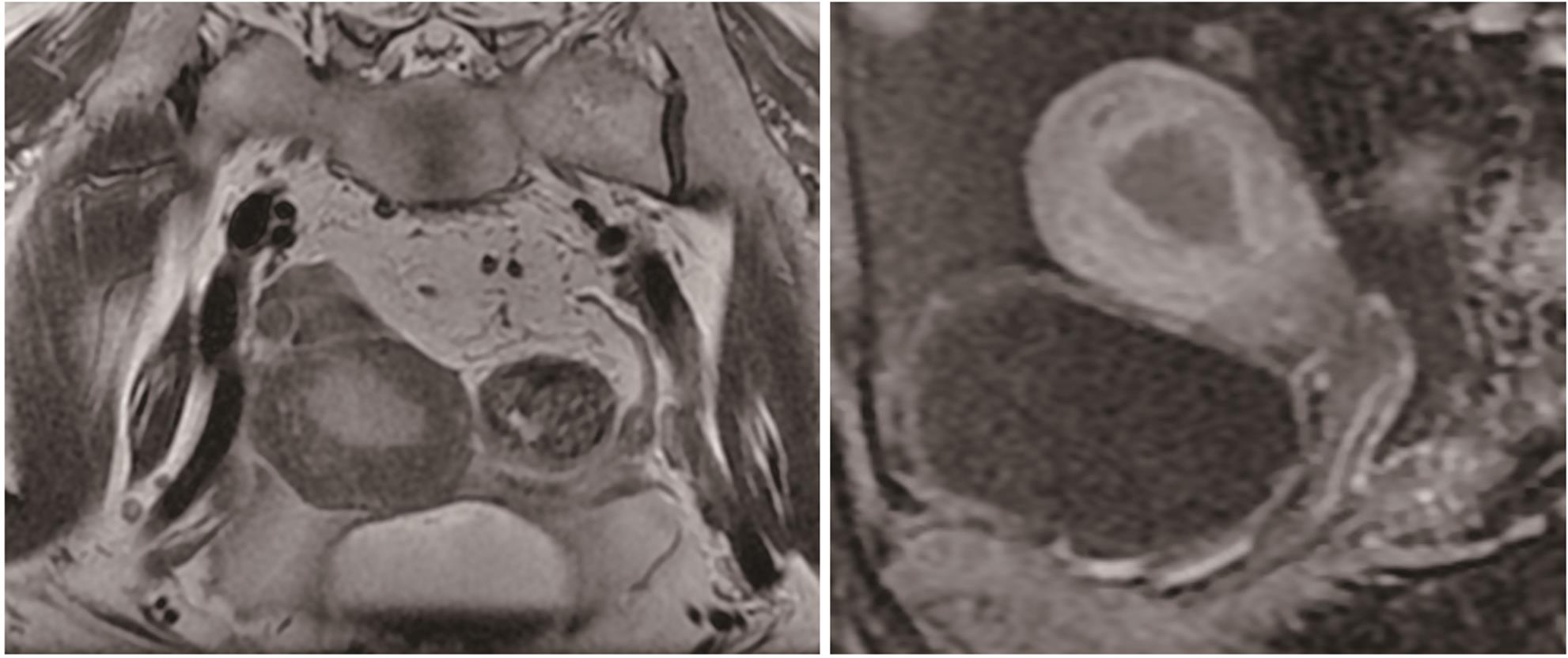
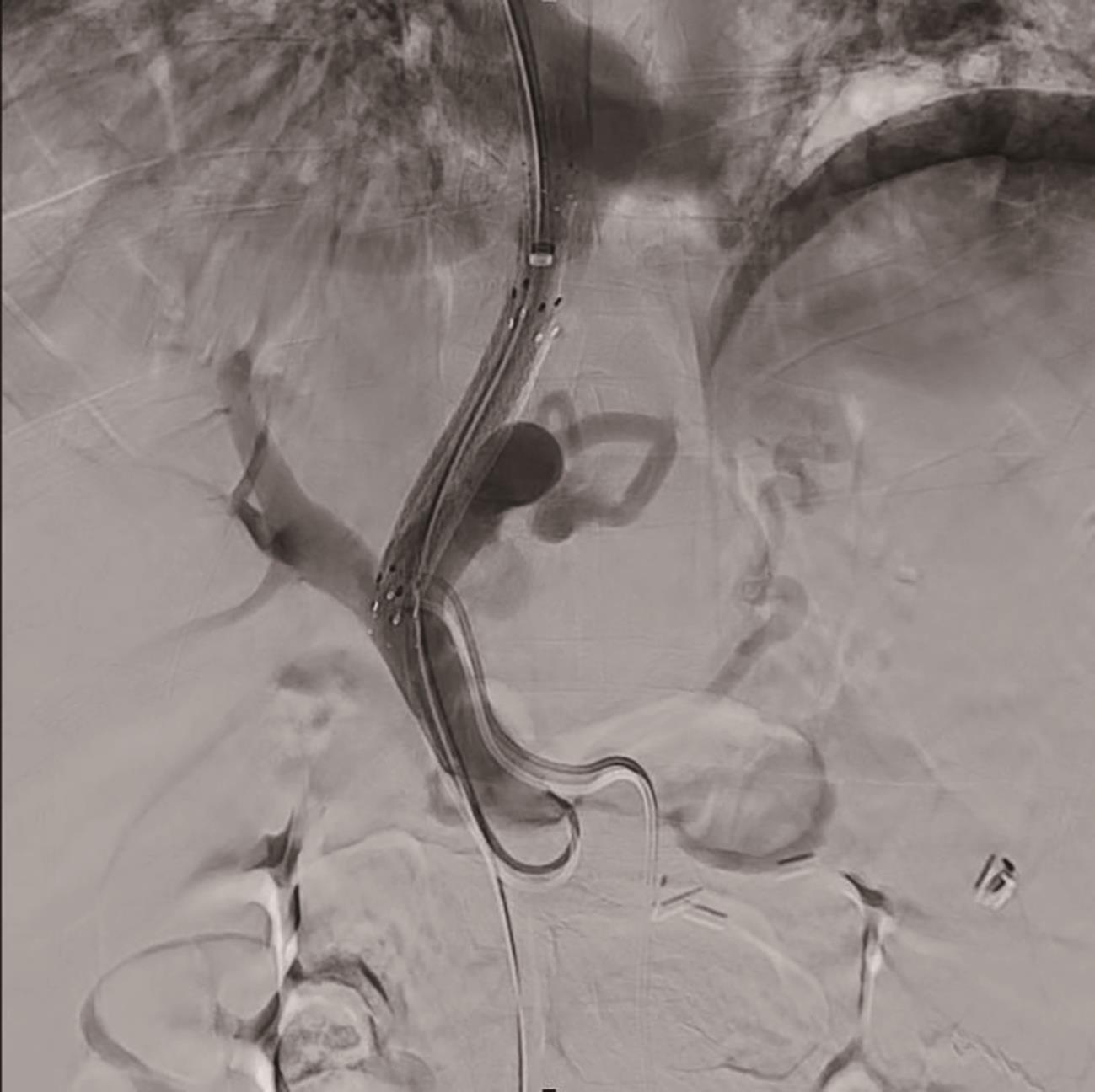
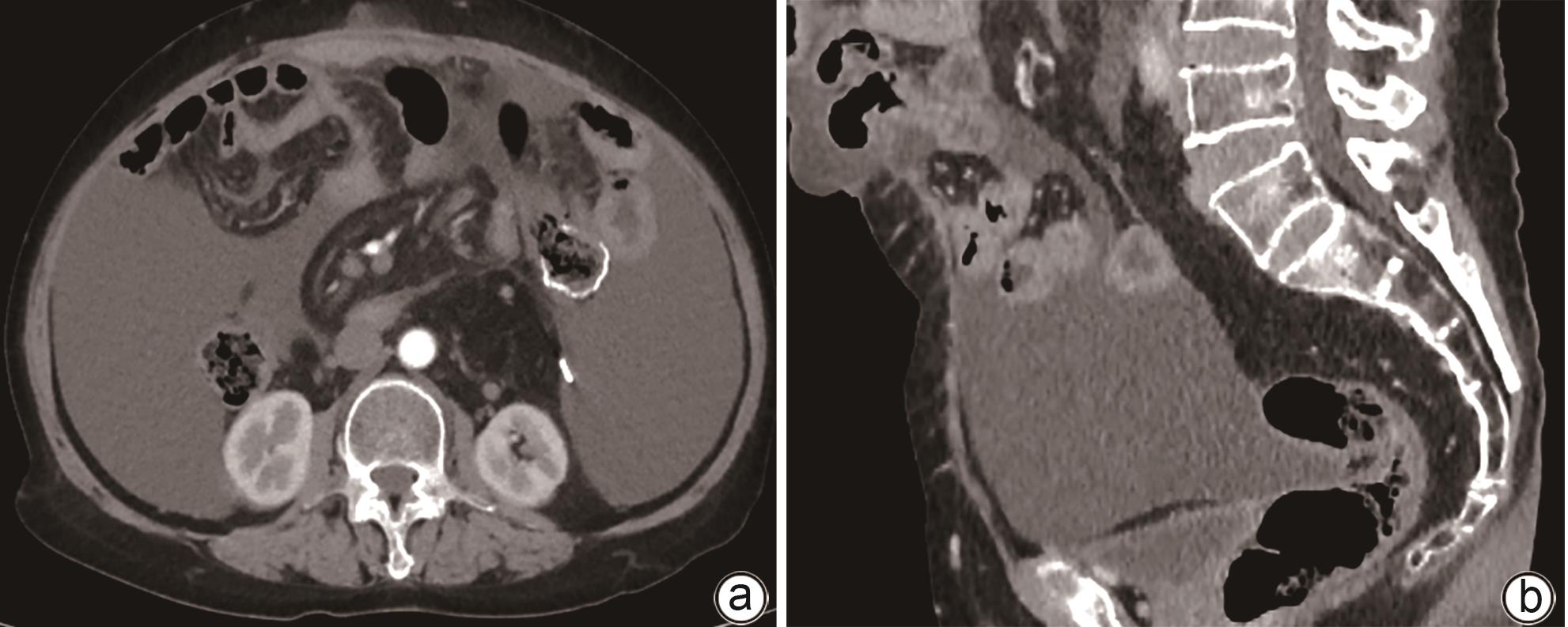
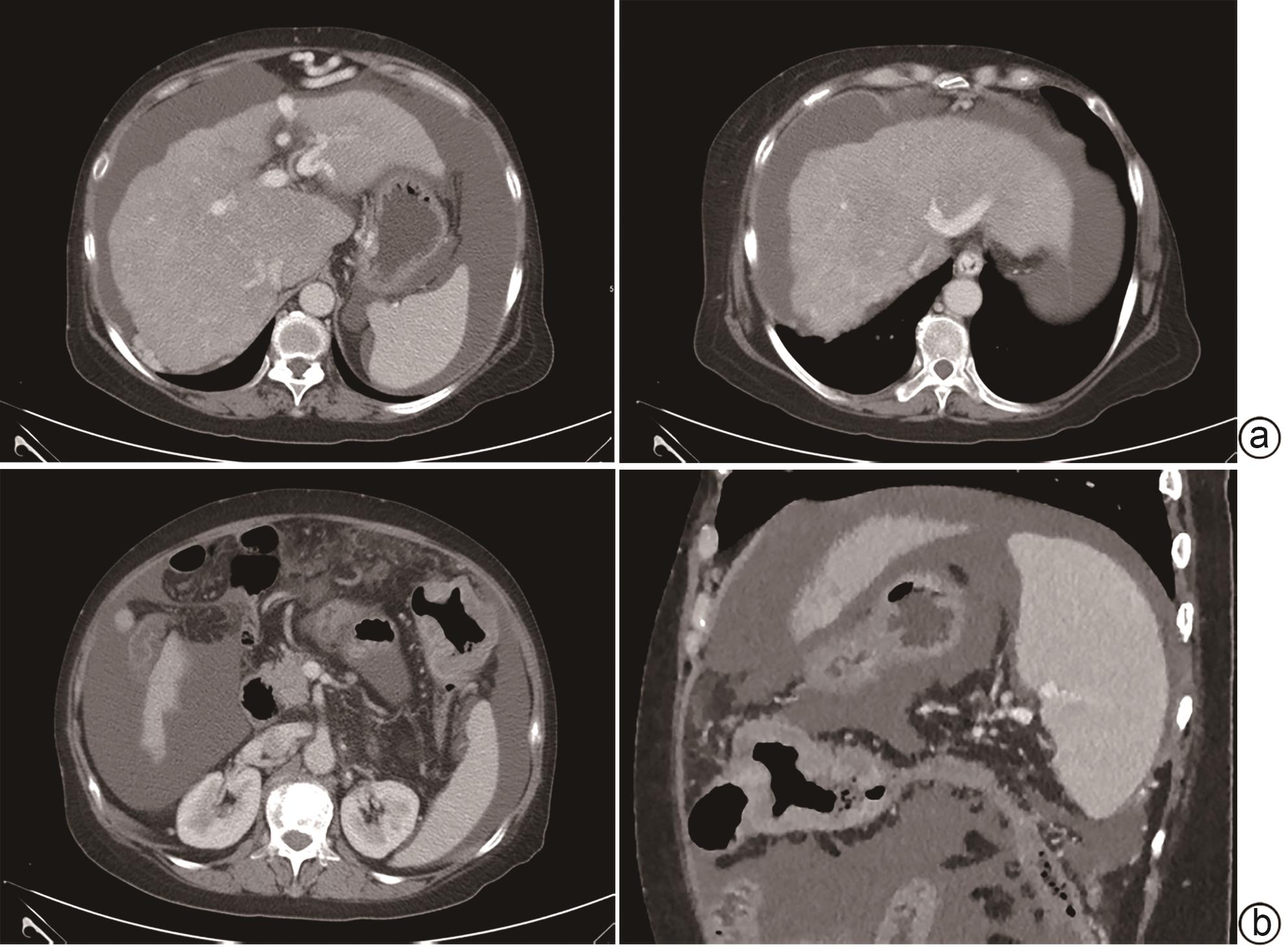
摘要: 多原发癌是指在同一个体中存在一种以上的具有不同组织学和部位的癌症,临床较为罕见。本文报告1例肝硬化失代偿期合并多原发癌的病例,主要讨论了肝硬化失代偿期患者合并多原发癌的诊治经过及临床启示。
-
关键词:
- 肝硬化 /
- 多原发癌 /
- 腹水 /
- 门体分流术, 经颈静脉肝内
Abstract: Multiple primary cancers (MPC) refer to the presence of more than one type of cancer with different histological features and sites in the same individual, and it is relatively rare in clinical practice. This article reports a case of decompensated cirrhosis with MPC and discusses the diagnosis, treatment, and clinical implications of this patient with decompensated cirrhosis and MPC. -
[1] Chinese Society of Hepatology, Chinese Medical Association. Guidelines on the management of ascites and complications in cirrhosis[J]. J Clin Hepatol, 2017, 33( 10): 1847- 1863. DOI: 10.3969/j.issn.1001-5256.2017.10.003.中华医学会肝病学分会. 肝硬化腹水及相关并发症的诊疗指南[J]. 临床肝胆病杂志, 2017, 33( 10): 1847- 1863. DOI: 10.3969/j.issn.1001-5256.2017.10.003. [2] ALLAHYARI A, MAHARATI A, JAFARI-NOZAD AM, et al. Prostate cancer, chronic myelogenous leukemia and multiple myeloma in a single patient: A case report and review of the literature[J]. J Med Case Rep, 2023, 17( 1): 35. DOI: 10.1186/s13256-023-03753-z. [3] IRIMIE A, ACHIMAS-CADARIU P, BURZ C, et al. Multiple primary malignancies: Epidemiological analysis at a single tertiary institution[J]. J Gastrointestin Liver Dis, 2010, 19( 1): 69- 73. [4] COPUR MS, MANAPURAM S. Multiple primary tumors over a lifetime[J]. Oncology, 2019, 33( 7): 629384. [5] WANG S, LIU Z, WANG GY, et al. Research status of multiple primary carcinoma[J]. Cancer Res Clin, 2018, 30( 9): 645- 648. DOI: 10.3760/cma.j.issn.1006-9801.2018.09.019.王松, 刘正, 王贵玉, 等. 多原发癌的研究现状[J]. 肿瘤研究与临床, 2018, 30( 9): 645- 648. DOI: 10.3760/cma.j.issn.1006-9801.2018.09.019. [6] JADAUN SS, SAIGAL S. Surgical risk assessment in patients with chronic liver diseases[J]. J Clin Exp Hepatol, 2022, 12( 4): 1175- 1183. DOI: 10.1016/j.jceh.2022.03.004. [7] ENDALE SIMEGN A, YAREGAL MELESSE D, BELAY BIZUNEH Y, et al. Perioperative management of patients with liver disease for non-hepatic surgery: A systematic review[J]. Ann Med Surg, 2022, 75: 103397. DOI: 10.1016/j.amsu.2022.103397. [8] ABBAS N, FALLOWFIELD J, PATCH D, et al. Guidance document: Risk assessment of patients with cirrhosis prior to elective non-hepatic surgery[J]. Frontline Gastroenterol, 2023, 14( 5): 359- 370. DOI: 10.1136/flgastro-2023-102381. [9] GARCIA-TSAO G, ABRALDES JG, BERZIGOTTI A, et al. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases[J]. Hepatology, 2017, 65( 1): 310- 335. DOI: 10.1002/hep.28906. [10] NEWMAN KL, JOHNSON KM, CORNIA PB, et al. Perioperative evaluation and management of patients with cirrhosis: Risk assessment, surgical outcomes, and future directions[J]. Clin Gastroenterol Hepatol, 2020, 18( 11): 2398- 2414. e 3. DOI: 10.1016/j.cgh.2019.07.051. [11] PATEL P, IRANI M, GRAVISS EA, et al. Impact of pre-operative transjugular intrahepatic portosystemic shunt on post-operative outcomes following non-transplant surgeries in patients with decompensated cirrhosis[J]. Transl Gastroenterol Hepatol, 2023, 8: 9. DOI: 10.21037/tgh-21-133. [12] NORTHUP PG, FRIEDMAN LS, KAMATH PS. AGA clinical practice update on surgical risk assessment and perioperative management in cirrhosis: expert review[J]. Clin Gastroenterol Hepatol, 2019, 17( 4): 595- 606. DOI: 10.1016/j.cgh.2018.09.043. [13] VINET E, PERREAULT P, BOUCHARD L, et al. Transjugular intrahepatic portosystemic shunt before abdominal surgery in cirrhotic patients: A retrospective, comparative study[J]. J Can De Gastroenterol, 2006, 20( 6): 401- 404. DOI: 10.1155/2006/245082. [14] FAGIUOLI S, BRUNO R, VENON WD, et al. Consensus conference on TIPS management: Techniques, indications, contraindications[J]. Dig Liver Dis, 2017, 49( 2): 121- 137. DOI: 10.1016/j.dld.2016.10.011. [15] WU FZ, CHEN XX, CHEN WY, et al. Multiple primary malignancies-hepatocellular carcinoma combined with splenic lymphoma: A case report[J]. World J Clin Cases, 2022, 10( 28): 10130- 10135. DOI: 10.12998/wjcc.v10.i28.10130. [16] QU MM, ZHU YH, LI YX, et al. Synchronous double primary hepatocellular carcinoma and intrahepatic cholangiocarcinoma: A case report and review of the literature[J]. Medicine, 2021, 100( 46): e27349. DOI: 10.1097/MD.0000000000027349. [17] ANTONIOU E, MANTAS D, PARASKEVA P, et al. How can we treat a patient with liver cirrhosis(hepatitis C virus), hepatocellular carcinoma, and synchronous colon cancer?[J]. Transplant Proc, 2012, 44( 9): 2745- 2747. DOI: 10.1016/j.transproceed.2012.09.003. -



 PDF下载 ( 1776 KB)
PDF下载 ( 1776 KB)

 下载:
下载: