红细胞分布宽度与血小板计数比值评估代谢相关脂肪性肝病及肝硬化的价值分析
DOI: 10.3969/j.issn.1001-5256.2022.04.013
Value of red blood cell distribution width-to-platelet ratio in evaluating metabolic-associated fatty liver disease and liver cirrhosis
-
摘要:
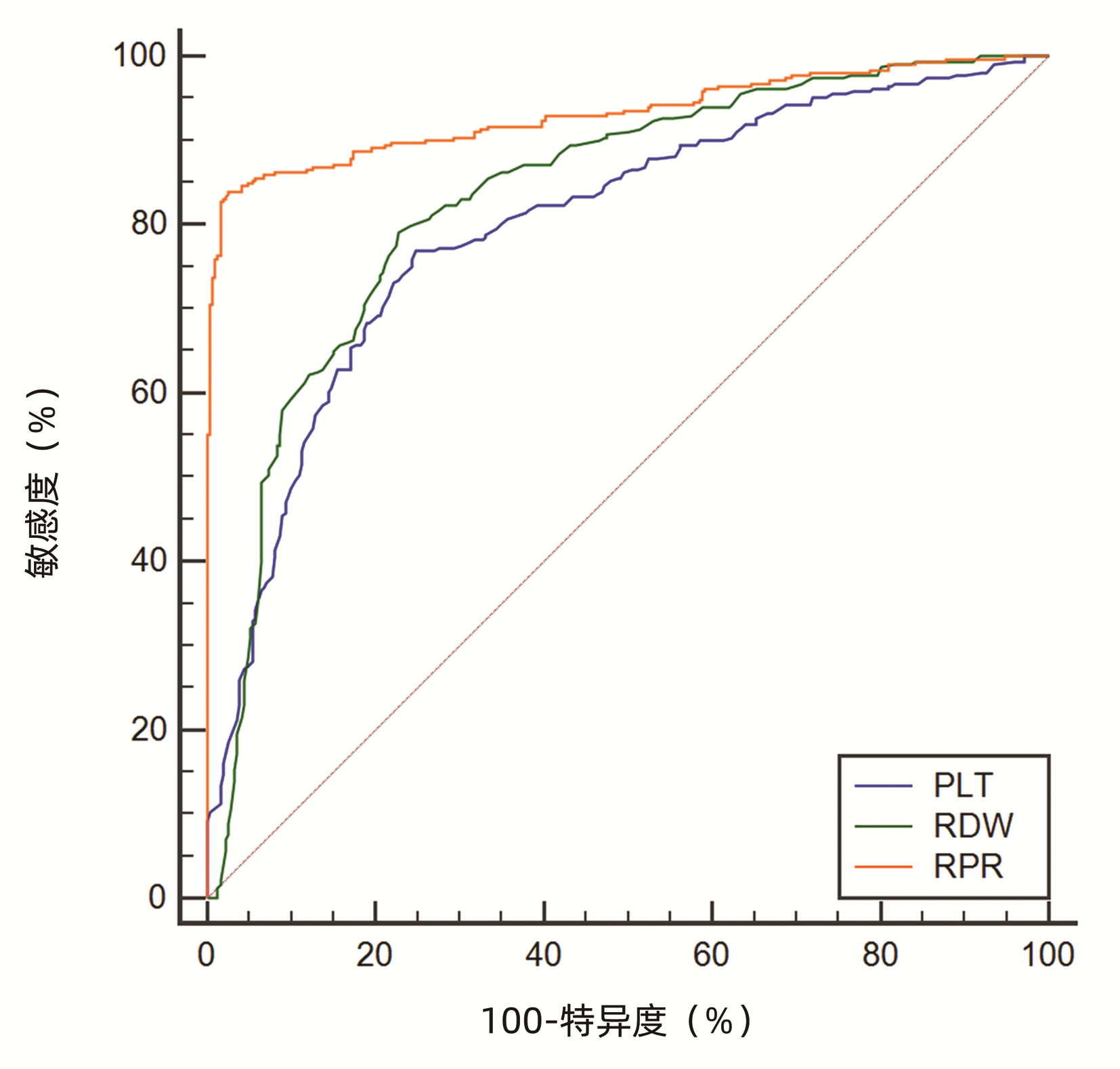
目的 评估红细胞分布宽度与血小板计数比值(RPR指数)在评价代谢相关性脂肪性肝病患者严重程度及预测脂肪肝相关肝硬化中的临床意义。 方法 选取2019年1月—2020年6月中国医科大学附属盛京医院收治的代谢相关性脂肪性肝病患者192例(A组)、脂肪肝相关肝硬化患者210例(B组)、同时期于本院体检中心健康体检的对照组206例(C组)。对研究对象进行一般测量、血细胞分析、血生化检测及腹部CT检查,并通过公式计算RPR、APRI、FIB-4指数。方差齐的计量资料3组间比较采用单因素方差分析,两两比较采用SNK法;方差不齐的计量资料3组间比较采用Kruskal -Wallis H检验,两两比较采用Mann-Whitney U检验;计数资料组间比较采用χ2检验,采用受试者工作特征曲线(ROC曲线)分析各变量预测肝硬化的准确性。 结果 3组间两两比较,RDW-SD、Alb、CREA、BMI、RPR以及APRI差异均有统计学意义(P值均<0.001)。WBC、PLT、ALT、AST、DBil、BUN以及FIB-4在A组与B组比较,差异均有统计学意义(P值均<0.05)。腰围、空腹血糖在A组分别与B组、C组比较时,差异均有统计学意义(P值均<0.001)。针对RPR指数,对轻、中、重度代谢相关性脂肪性肝病3组间进行两两比较,差异均有统计学意义(P值均<0.05)。最后对RPR、APRI、FIB-4三种无创模型预测脂肪肝相关肝硬化的诊断效能进行ROC曲线分析,AUC分别为0.932、0.815、0.877。 结论 RPR指数在肝病的不同阶段存在差异,随着脂肪肝的加重,RPR指数逐渐增高,并且对脂肪肝相关肝硬化的预警价值高于APRI和FIB-4指数。 Abstract:Objective To investigate the clinical significance of red blood cell distribution width-to-platelet ratio (RPR index) in evaluating the severity of metabolic-associated fatty liver disease and predicting fatty liver-associated cirrhosis. Methods A total of 192 patients with metabolic-associated fatty liver disease and 210 patients with fatty liver-associated cirrhosis who were admitted to Shengjing Hospital of China Medical University from January 2019 to June 2020 were enrolled as group A and group B, respectively, and 206 individuals who underwent physical examination in our hospital during the same period of time were enrolled as control group (group C). All subjects underwent general measurement, blood cell analysis, blood biochemical test, and abdominal CT examination, and related formulas were used to calculate RPR, aspartate aminotransferase-to-platelet ratio index (APRI), and fibrosis-4 (FIB-4) index. A one-way analysis of variance was used for comparison of continuous data with homogeneity of variance between groups, and the SNK method was used for comparison between two groups; the Kruskal-Wallis H test was used for comparison of continuous data with heterogeneity of variance between groups, and the Mann-Whitney U test was used for comparison between two groups; the chi-square test was used for comparison of categorical data between groups; the receiver operating characteristic (ROC) curve was used to analyze the accuracy of the prediction of liver cirrhosis. Results There were significant differences in red blood cell distribution width-standard deviation, albumin, creatinine, body mass index, RPR, and APRI between any two groups (all P < 0.001), and there were significant differences in white blood cell count, platelet count, alanine aminotransferase, aspartate aminotransferase, direct bilirubin, blood urea nitrogen, and FIB-4 between group A and group B (all P < 0.05). There were significant differences in waist circumference and fasting blood glucose between groups A and B and between groups A and C (all P < 0.001). There was a significant difference in RPR between any two groups of the mild, moderate, and severe metabolic-associated fatty liver disease groups (all P < 0.05). In terms of diagnostic efficiency, the three noninvasive models RPR, APRI, and FIB-4 had an area under the ROC curve of 0.932, 0.815, and 0.877, respectively, in predicting fatty liver-associated cirrhosis. Conclusion There is a difference in RPR index between different stages of liver disease, and RPR index gradually increases with the aggravation of metabolic-associated fatty liver disease. RPR index has a higher value than APRI and FIB-4 in the warning of fatty liver-associated cirrhosis. -
表 1 纳入患者的临床数据比较
Table 1. Comparison of clinical data of patients
变量 A组(n=192) B组(n=210) C组(n=206) 统计值 P值 男/女(例) 101/91 115/95 99/107 χ2=1.943 0.379 年龄(岁) 49.82±8.68 49.36±7.98 49.49±8.57 F=0.158 0.854 WBC(×109/L) 6.10(4.70~7.54) 3.55(2.54~4.74)1) 5.93(5.14~6.63) H=216.061 <0.001 PLT(×109/L) 236.00(171.00~291.00) 89.00(60.50~127.00)1) 234.00(216.00~253.25) H=429.452 <0.001 RDW-SD(fL) 42.30(39.88~48.00) 53.10(49.80~58.30)1) 40.70(39.60~42.15)1)2) H=336.315 <0.001 Alb(g/L) 37.80(32.10~41.70) 29.80(27.38~32.93)1) 43.60(41.29~46.03)1)2) H=378.093 <0.001 ALT(U/L) 22.50(13.75~36.00) 26.00(17.00~41.50)1) 22.00(15.75~31.00) H=14.133 <0.001 AST(U/L) 21.00(15.00~29.75) 27.50(18.00~52.00)1) 20.53(15.59~30.42) H=27.270 <0.001 DBil(μmol/L) 9.30(7.00~14.70) 18.95(13.35~26.00)1) 11.08(8.98~13.46) H=161.010 <0.001 CREA(μmol/L) 57.20(37.15~74.95) 65.80(54.90~86.00)1) 63.02(53.82~74.20)1)2) H=33.449 <0.001 BUN(mmol/L) 4.00(2.99~5.02) 5.57(4.23~7.48)1) 4.17(3.61~4.81) H=98.987 <0.001 CRP(mg/L) 6.38(5.33~7.78) 6.54(5.24~7.68) 6.43(5.38~7.98) H=0.420 0.809 空腹血糖(mmol/L) 6.38(5.43~9.23) 5.54(4.92~6.59)1) 5.49(5.11~6.13)1) H=48.550 <0.001 BMI(kg/m2) 26.14±4.59 23.29±3.581) 21.77±3.231)2) F=66.620 <0.001 腰围(cm) 88.1±9.2 84.4±12.51) 82.8±10.41) F=12.960 <0.001 注:与A组比较,1)P<0.01;与B组比较,2)P<0.01。 表 2 MAFLD组、肝硬化组及健康组3种无创模型参数比较
Table 2. Comparison of parameters of three non-invasive models among MAFLD group, cirrhosis group and healthy group
变量 A组 B组 C组 H值 P值 RPR 0.19(0.16~0.25) 0.61(0.41~0.95)1) 0.15(0.11~0.20)1)2) 384.398 <0.001 APRI 0.35(0.26~0.59) 1.21(0.79~1.85)1) 0.30(0.23~0.43)1)2) 362.650 <0.001 FIB-4 1.07(0.74~1.48) 4.93(3.13~7.23)1) 0.95(0.76~1.21) 460.801 <0.001 注:与A组比较,1)P<0.01;与B组比较,2)P<0.01。 表 3 轻、中、重度MAFLD患者RPR指数比较
Table 3. Comparison of RPR index among mild, moderate and severe MAFLD patients
组别 例数 RPR 轻度组 64 0.14(0.15~0.18) 中度组 70 0.18(0.16~0.20)1) 重度组 58 0.22(0.19~0.27)1)2) H值 96.638 P值 <0.001 注:与轻度组比较,1)P<0.01;与中度组比较,2)P<0.01。 表 4 RDW-SD、PLT、RPR指数诊断肝硬化效能分析
Table 4. Efficiency analysis of RDW-SD, PLT and RPR indexes in diagnosing liver cirrhosis
无创诊断模型 AUC 95%CI Cut-off 敏感度(%) 特异度(%) P值 RDW-SD 0.833 0.801~0.866 0.563 4 79.17 77.17 <0.000 1 PLT 0.799 0.764~0.834 0.521 6 76.92 75.24 <0.000 1 RPR 0.932 0.910~0.951 0.814 0 83.97 97.43 <0.000 1 表 5 3种无创诊断模型诊断肝硬化效能分析
Table 5. Three efficacy analysis of non-invasive diagnostic models in the diagnosis of liver cirrhosis
无创诊断模型 AUC 95%CI Cut-off 敏感度(%) 特异度(%) P值 RPR 0.932 0.910~0.951 0.814 0 83.97 97.43 <0.000 1 APRI 0.815 0.783~0.845 0.537 9 71.47 82.32 <0.000 1 FIB-4 0.877 0.849~0.902 0.646 9 81.09 83.60 <0.000 1 -
[1] YOUNOSSI ZM, KOENIG AB, ABDELATIF D, et al. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes[J]. Hepatology, 2016, 64(1): 73-84. DOI: 10.1002/hep.28431. [2] XUE R, FAN JG. Brief introduction of an international expert consensus statement: A new definition of metabolic associated fatty liver disease[J]. J Clin Hepatol, 2020, 36(6): 1224-1227. DOI: 10.3969/j.issn.1001-5256.2020.06.007.薛芮, 范建高. 代谢相关脂肪性肝病新定义的国际专家共识简介[J]. 临床肝胆病杂志, 2020, 36(6): 1224-1227. DOI: 10.3969/j.issn.1001-5256.2020.06.007. [3] LEONI S, TOVOLI F, NAPOLI, et al. Current guidelines for the management of non-alcoholic fatty liver disease: A systematic review with comparative analysis[J]. World J Gastroenterol, 2018, 24(30): 3361-3373. DOI: 10.3748/wjg.v24.i30.3361. [4] SHIHA G, ALSWAT K, AL KHATRY M, et al. Nomenclature and definition of metabolic-associated fatty liver disease: A consensus from the Middle East and north Africa[J]. Lancet Gastroenterol Hepatol, 2021, 6(1): 57-64. DOI: 10.1016/S2468-1253(20)30213-2. [5] SHIHA G, IBRAHIM A, HELMY A, et al. Asian-Pacific Association for the Study of the Liver (APASL) consensus guidelines on invasive and non-invasive assessment of hepatic fibrosis: A 2016 update[J]. Hepatol Int, 2017, 11(1): 1-30. DOI: 10.1007/s12072-016-9760-3. [6] WAI CT, GREENSON JK, FONTANA RJ, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C[J]. Hepatology, 2003, 38(2): 518-526. DOI: 10.1053/jhep.2003.50346. [7] WANG H, WANG J, XIA J, et al. Red cell distribution width to platelet ratio predicts liver fibrosis in patients with autoimmune hepatitis[J]. Medicine (Baltimore), 2020, 99(34): e21408. DOI: 10.1097/MD.0000000000021408. [8] ZHU LY, LI YC, DENG LH, et al. Research advances in extrahepatic diseases associated with nonalcoholic fatty liver disease[J]. J Clin Hepatol, 2021, 37(9): 2215-2219. DOI: 10.3969/j.issn.1001-5256.2021.09.043.朱蕗颖, 李雨晨, 邓利华, 等. 非酒精性脂肪性肝病相关肝外疾病的研究进展[J]. 临床肝胆病杂志, 2021, 37(9): 2215-2219. DOI: 10.3969/j.issn.1001-5256.2021.09.043. [9] MOTAMED N, RABIEE B, HEMASI GR, et al. Body roundness index and waist-to-height ratio are strongly associated with non-alcoholic fatty liver disease: A population-based study[J]. Hepat Mon, 2016, 16(9): e39575. DOI: 10.5812/hepatmon.39575. [10] CUI HZ, MA XM, LIU Q, et al. Influence of the interaction between abdominal obesity and hypertriglyceridemia on the development of nonalcoholic fatty liver disease[J]. J Clin Hepatol, 2020, 36(6): 1314-1319. DOI: 10.3969/j.issn.1001-5256.2020.06.025.崔皓哲, 马向明, 刘倩, 等. 腹型肥胖与甘油三酯的交互作用对非酒精性脂肪性肝病发病的影响[J]. 临床肝胆病杂志, 2020, 36(6): 1314-1319. DOI: 10.3969/j.issn.1001-5256.2020.06.025. [11] CETINKAYA E, SENOL K, SAYLAM B, et al. Red cell distribution width to platelet ratio: New and promising prognostic marker in acute pancreatitis[J]. World J Gastroenterol, 2014, 20(39): 14450-14454. DOI: 10.3748/wjg.v20.i39.14450. [12] PUSUROGLU H, CAKMAK HA, AKGUL O, et al. The prognostic value of admission red cell distribution width-to-platelet ratio in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention[J]. Rev Port Cardiol, 2015, 34(10): 597-606. DOI: 10.1016/j.repc.2015.03.014. [13] JIANG X, WANG Y, SU Z, et al. Red blood cell distribution width to platelet ratio levels in assessment of histologic severity in patients with primary biliary cholangitis[J]. Scand J Clin Lab Invest, 2018, 78(4): 258-263. DOI: 10.1080/00365513.2018.1449011. [14] XIE S, CHEN X. Red blood cell distribution width-to-platelet ratio as a disease activity-associated factor in systemic lupus erythematosus[J]. Medicine (Baltimore), 2018, 97(39): e12342. DOI: 10.1097/MD.0000000000012342. [15] CAI Y, LIU D, CUI J, et al. Diagnostic accuracy of red blood cell distribution width to platelet ratio for predicting staging liver fibrosis in chronic liver disease patients: A systematic review and meta-analysis[J]. Medicine (Baltimore), 2019, 98(14): e15096. DOI: 10.1097/MD.0000000000015096. [16] SALVAGNO GL, SANCHIS-GOMAR F, PICANZA A, et al. Red blood cell distribution width: A simple parameter with multiple clinical applications[J]. Crit Rev Clin Lab Sci, 2015, 52(2): 86-105. DOI: 10.3109/10408363.2014.992064. [17] LI N, ZHOU H, TANG Q. Red blood cell distribution width: A novel predictive indicator for cardiovascular and cerebrovascular diseases[J]. Dis Markers, 2017, 2017: 7089493. DOI: 10.1155/2017/7089493. [18] LYU H, ZHU CL, HAO SY. Change and significance of red cell distribution width in patients with non-alcoholic steatohepatitis[J]. J Chin Pract Diagn Ther, 2016, 30(8): 765-766. DOI: 10.13507/j.issn.1674-3474.2016.08.013.吕辉, 祝成亮, 郝世勇. 非酒精性脂肪性肝炎患者红细胞分布宽度变化及意义[J]. 中华实用诊断与治疗杂志, 2016, 30(8): 765-766. DOI: 10.13507/j.issn.1674-3474.2016.08.013. [19] LI Y, DAI ZY, HUANG JJ, et al. Differences of erythrocyte distribution width and prothrombin time in patients with different degrees of liver injury[J]. Chongqing Med, 2017, 46(36): 5074-5075. DOI: 10.3969/j.issn.1671-8348.2017.36.012.李月, 代震宇, 黄佳佳, 等. 不同程度肝损伤患者红细胞分布宽度与凝血酶原时间的差异[J]. 重庆医学, 2017, 46(36): 5074-5075. DOI: 10.3969/j.issn.1671-8348.2017.36.012. [20] MALEHMIR M, PFISTER D, GALLAGE S, et al. Platelet GPIbα is a mediator and potential interventional target for NASH and subsequent liver cancer[J]. Nat Med, 2019, 25(4): 641-655. DOI: 10.1038/s41591-019-0379-5. -



 PDF下载 ( 2520 KB)
PDF下载 ( 2520 KB)

 下载:
下载:



