介入封堵治疗小儿Ⅱ型Abernethy畸形合并肺动脉高压1例报告
DOI: 10.3969/j.issn.1001-5256.2023.11.022
伦理学声明:本例报告已获得患者家属知情同意。
利益冲突声明:本文不存在任何利益冲突。
作者贡献声明:张恒负责课题设计,资料分析,撰写论文;方志成、孟忠吉、杜恩辅参与收集数据,修改论文;江斌负责拟定写作思路,指导撰写文章并最后定稿。
Transcatheter closure of rare type Ⅱ Abernethy malformation with pulmonary hypertension in children: A case report
-
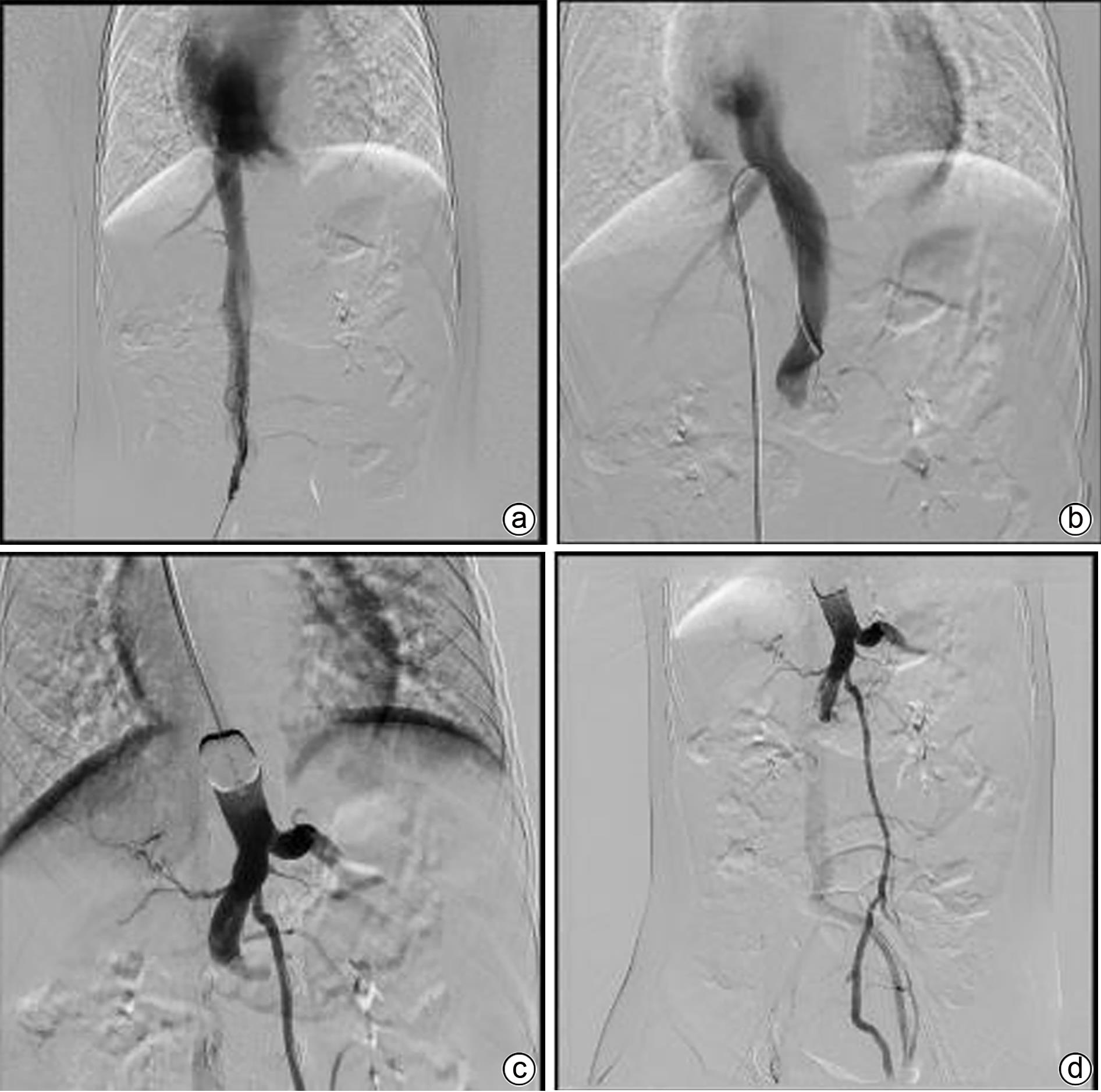
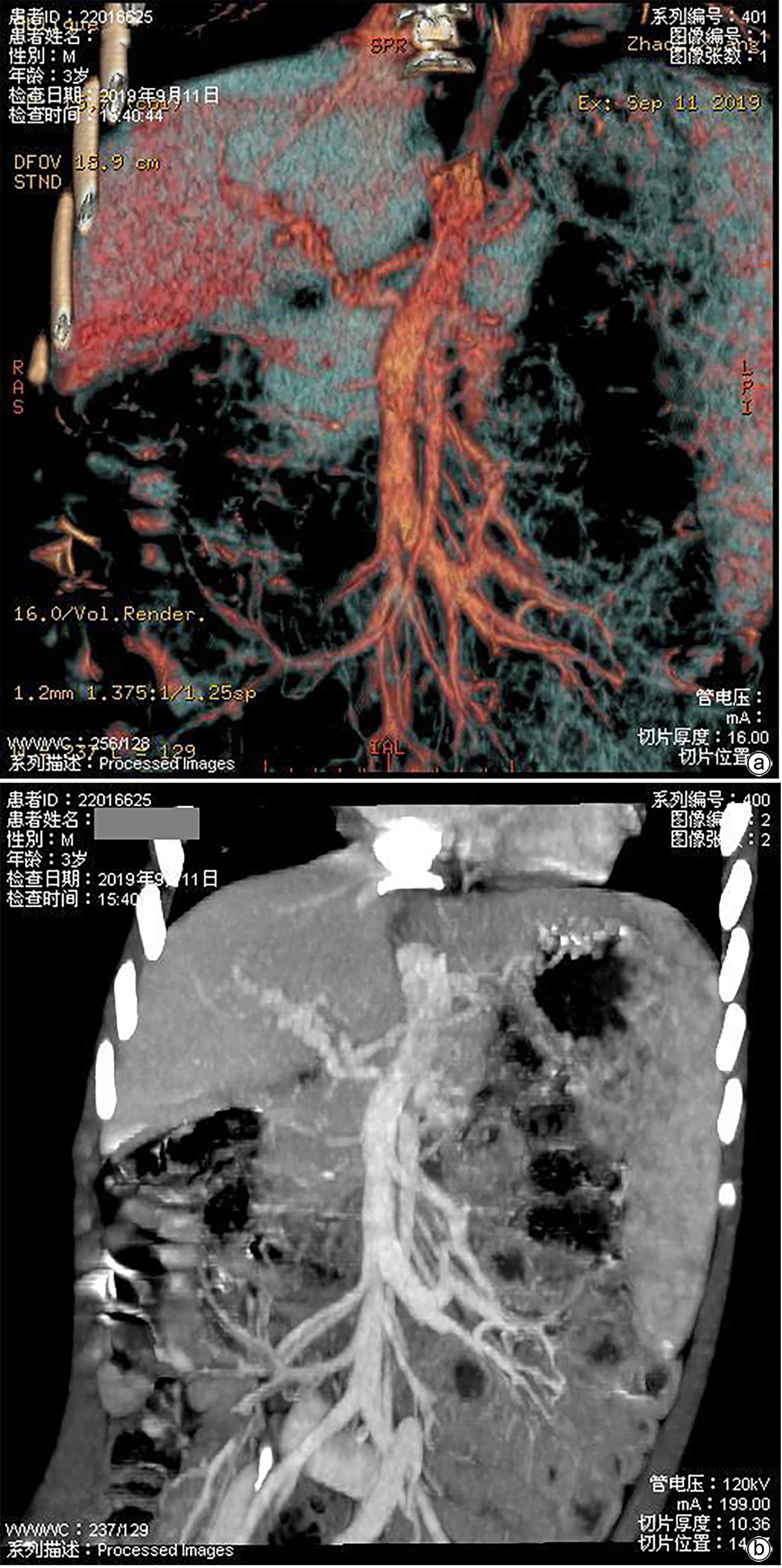
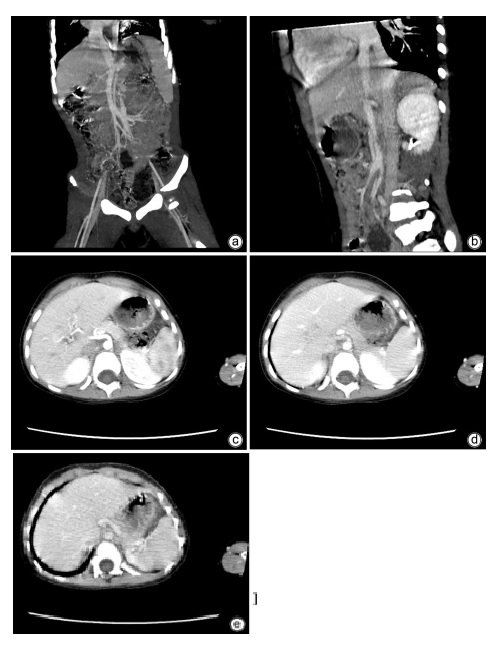
摘要: Abernethy又称先天性门体静脉分流畸形,临床罕见,截至2019年全球文献报道不足300例,该病可合并肺动脉高压、肝脏肿瘤、肝衰竭等严重并发症,总体预后极差,早期诊断、积极有效治疗可降低和延缓并发症发生。本文通过门静脉造影,结合球囊阻断,将原本发育不良、纤细未显影的门静脉显影,从而将原本误诊为Ⅰ型Abernethy畸形的患儿明确为Ⅱ型Abernethy畸形,进而经介入封堵治疗成功救治患儿,现报道如下。
-
关键词:
- Abernethy畸形 /
- 诊断 /
- 介入封堵 /
- 治疗
Abstract: Abernethy malformation, also known as congenital portosystemic shunts, is rare in clinical practice, with less than 300 cases reported in the global literature up to 2019. The disease can have serious complications such as pulmonary hypertension, liver tumor, and liver failure and tends to have an extremely poor prognosis, and early diagnosis and active and effective treatment can reduce and delay the onset of complications. In this case, portography combined with balloon occlusion helped to display the underdeveloped slender portal vein with dysplasia, so that the child who was formerly misdiagnosed with type Ⅰ Abernethy malformation was diagnosed with type Ⅱ Abernethy malformation, and then the child was successfully treated by transcatheter closure. This article gives a detailed report of this case.-
Key words:
- Abernethy Malformation /
- Diagnosis /
- Interventional Closure /
- Management
-
-
[1] BAIGES A, TURON F, SIMÓN-TALERO M, et al. Congenital extrahepatic portosystemic shunts(abernethy malformation): An international observational study[J]. Hepatology, 2020, 71( 2): 658- 669. DOI: 10.1002/hep.30817. [2] MORGAN G, SUPERINA R. Congenital absence of the portal vein: Two cases and a proposed classification system for portasystemic vascular anomalies[J]. J Pediatr Surg, 1994, 29( 9): 1239- 1241. DOI: 10.1016/0022-3468(94)90812-5. [3] TAYDAS O, DANISAN G, OGUL H, et al. A rare cause of congenital portosystemic shunt: Type 2 Abernethy malformation[J]. Folia Morphol, 2020, 79( 1): 172- 175. DOI: 10.5603/FM.a2019.0063. [4] KANAMORI Y, HASHIZUME K, KITANO Y, et al. Congenital extrahepatic portocaval shunt(Abernethy type 2), huge liver mass, and patent ductus arteriosus: A case report of its rare clinical presentation in a young girl[J]. J Pediatr Surg, 2003, 38( 4): E15. DOI: 10.1053/jpsu.2003.50153. [5] LEMOINE C, NILSEN A, BRANDT K, et al. Liver histopathology in patients with hepatic masses and the Abernethy malformation[J]. J Pediatr Surg, 2019, 54( 2): 266- 271. DOI: 10.1016/j.jpedsurg.2018.10.083. [6] SORKIN T, STRAUTNIEKS S, FOSKETT P, et al. Multiple β-catenin mutations in hepatocellular lesions arising in Abernethy malformation[J]. Hum Pathol, 2016, 53: 153- 158. DOI: 10.1016/j.humpath.2016.02.025. [7] LIU Y, CHENG L, XIANG LJ, et al. Type Ⅱ Abernethy malformation misdiagnosed as thrombocytopenia: A case report and literature review[J]. J Hepatopancreatobiliary Surg, 2019, 31( 1): 58- 61. DOI: 10.11952/j.issn.1007-1954.2019.01.015.刘燕, 程黎, 向伦建, 等. Ⅱ型Abernethy畸形误诊为血小板减少症一例并文献复习[J]. 肝胆胰外科杂志, 2019, 31( 1): 58- 61. DOI: 10.11952/j.issn.1007-1954.2019.01.015. [8] SHARMA R, SUDDLE A, QUAGLIA A, et al. Congenital extrahepatic portosystemic shunt complicated by the development of hepatocellular carcinoma[J]. Hepatobiliary Pancreat Dis Int, 2015, 14( 5): 552- 557. DOI: 10.1016/s1499-3872(15)60418-0. [9] GUO C, ZHONG YM, WANG Q, et al. Diagnostic accuracy of multi-slice computed tomography in children with Abernethy malformation[J]. BMC Med Imaging, 2019, 19( 1): 97. DOI: 10.1186/s12880-019-0396-3. [10] KIM ES, LEE KW, CHOE YH. The characteristics and outcomes of abernethy syndrome in Korean children: A single center study[J]. Pediatr Gastroenterol Hepatol Nutr, 2019, 22( 1): 80- 85. DOI: 10.5223/pghn.2019.22.1.80. [11] HUANG SG. Progress in diagnosis and treatment of congenital portosystemic shunt[J]. J Clin Surg, 2013, 21( 8): 646- 649. DOI: 10.3969/j.issn.1005-6483.2013.08.027.黄顺根. 先天性门体分流诊治进展[J]. 临床外科杂志, 2013, 21( 8): 646- 649. DOI: 10.3969/j.issn.1005-6483.2013.08.027. [12] SUN ZP, JIANG B, SHEN XB, et al. A case of congenital extrahepatic portal vein shunt complicated with lower gastrointestinal bleeding treated by inferior mesenteric vein-inferior vena cava shunt[J]. Chin J Hepatobiliary Surg, 2017, 23( 8): 525, 529. DOI: 10.3760/cma.j.issn.1007-8118.2017.08.006.孙增鹏, 蒋波, 沈贤波, 等. 肠系膜下静脉-下腔静脉分流治疗先天性肝外门腔静脉分流并发下消化道出血一例[J]. 中华肝胆外科杂志, 2017, 23( 8): 525, 529. DOI: 10.3760/cma.j.issn.1007-8118.2017.08.006. [13] KUMAR P, BHATIA M, GARG A, et al. Abernethy malformation: A comprehensive review[J]. Diagn Interv Radiol, 2022, 28( 1): 21- 28. DOI: 10.5152/dir.2021.20474. [14] BUENO J, PÉREZ M, LOPEZ-BEN S, et al. Radiological and surgical differences between congenital end-to-side(Abernethy malformation) and side-to-side portocaval shunts[J]. J Pediatr Surg, 2020, 55( 9): 1897- 1902. DOI: 10.1016/j.jpedsurg.2020.01.053. [15] ZHANG H, JIANG B, MENG ZJ. The neglected portal intrahepatic shunts[J]. Am J Gastroenterol, 2023, 118( 5): 909. DOI: 10.14309/ajg.0000000000002177. [16] LI L, GOU CY, LI JY, et al. Abernethy malformation misdiagnosed as liver cirrhosis: A report of one case[J]. J Clin Hepatol, 2014, 30( 9): 932- 934. DOI: 10.3969/j.issn.1001-5256.2014.09.024.李丽, 勾春燕, 李晶滢, 等. Abernethy畸形误诊为肝硬化1例报告[J]. 临床肝胆病杂志, 2014, 30( 9): 932- 934. DOI: 10.3969/j.issn.1001-5256.2014.09.024. [17] THIRAPATTARAPHAN C, TREEPONGKARUNA S, RUANGWATTANAPAISARN N, et al. Congenital extrahepatic portosystemic shunt(Abernethy malformation) treated with surgical shunt ligation: A case report and literature review[J]. Int J Surg Case Rep, 2020, 66: 4- 7. DOI: 10.1016/j.ijscr.2019.11.014. [18] ZHANG JS, LI L, LI Q, et al. Surgical treatment of Abernethy malformation type Ⅱ: A report of five cases[J]. Chin J Surg, 2017, 55( 12): 947- 950. DOI: 10.3760/cma.j.issn.0529-5815.2017.12.014.张金山, 李龙, 李颀, 等. Ⅱ型Abernethy畸形五例的外科疗效[J]. 中华外科杂志, 2017, 55( 12): 947- 950. DOI: 10.3760/cma.j.issn.0529-5815.2017.12.014. -



 PDF下载 ( 1074 KB)
PDF下载 ( 1074 KB)

 下载:
下载: